When a fungal infection turns serious-like candidiasis in the bloodstream or aspergillosis in the lungs-it’s not something you can treat with cream or spray. You need strong, targeted antifungal drugs. Two main classes of these drugs, azoles and echinocandins, are the backbone of modern treatment for life-threatening fungal infections. But choosing between them isn’t just about effectiveness. It’s about safety, cost, how they’re given, and how they interact with everything else a patient is taking.
Azoles: The Oral Workhorses
Azoles include fluconazole, itraconazole, voriconazole, and posaconazole. They’ve been around for decades, with ketoconazole being the first, approved in 1981. Today, they’re the most commonly prescribed systemic antifungals in the U.S., making up nearly 70% of all prescriptions.
How do they work? They block a key enzyme in fungi called lanosterol 14-alpha-demethylase. Without this enzyme, the fungus can’t build a strong cell membrane. The result? The fungal cells fall apart.
The big advantage? Most azoles come as pills. Fluconazole, for example, is absorbed almost perfectly-90% of the pill makes it into your bloodstream. That makes it ideal for outpatient care, long-term treatment, or follow-up after hospital discharge. It also reaches good levels in the brain and urine, which matters for infections like fungal meningitis or bladder infections.
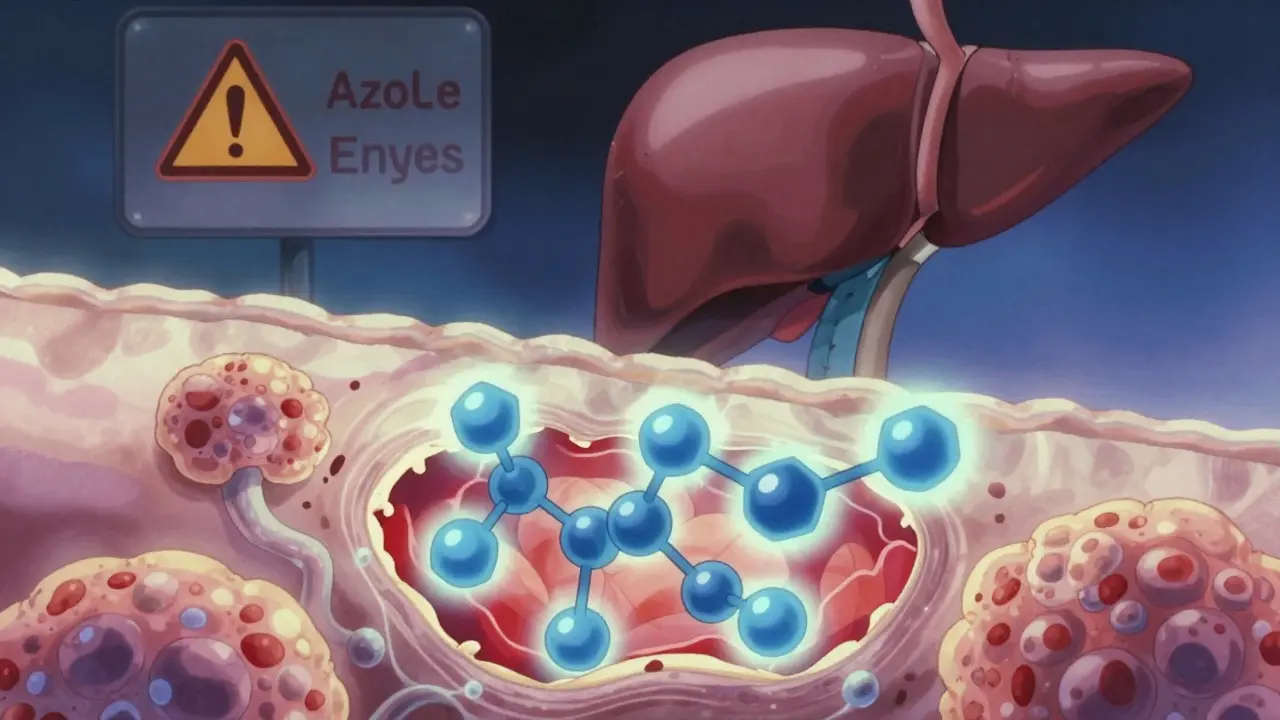
But here’s the catch: azoles don’t just target fungi. They also interfere with human liver enzymes, especially CYP3A4 and CYP2C9. These are the same enzymes that break down blood thinners, seizure meds, statins, and even some antidepressants. A 2022 study found azoles have over 1,100 moderate to severe drug interactions. That means if you’re on warfarin, cyclosporine, or phenytoin, adding fluconazole or voriconazole can be dangerous-sometimes deadly. One doctor on Reddit described three cases where voriconazole doubled phenytoin levels in just two days, forcing emergency dose cuts.
Another major concern is liver damage. The FDA requires quarterly liver tests for anyone on long-term azole therapy. About 12% of patients on azoles develop noticeable liver injury, compared to under 5% on echinocandins. Ketoconazole was pulled from the U.S. market in 2013 because it caused liver failure in too many people-228 times more likely than in non-users.
Echinocandins: The IV Powerhouses
Echinocandins-caspofungin, micafungin, and anidulafungin-are newer. The first one, caspofungin, hit the market in 2001. Unlike azoles, they don’t touch cell membranes. Instead, they smash the fungal cell wall by blocking glucan synthesis. Think of it like removing the bricks from a wall. The fungus collapses.
They’re only available as IV infusions. That’s a drawback for outpatient use. But in the ICU, it’s a strength. Critically ill patients often can’t absorb pills properly. Echinocandins work reliably regardless of gut function.
They’re also much gentler on the liver and kidneys. Studies show echinocandins cause acute kidney injury in just 1.2% of patients, while azoles do so in over 8%. That’s why the Infectious Diseases Society of America (IDSA) recommends echinocandins as first-line for invasive candidiasis in patients with sepsis or shock.
Drug interactions? Minimal. Only about 340 moderate to severe interactions total-less than a third of azoles. That’s a huge win in complex hospital cases where patients are on 10+ medications.
But they’re expensive. A seven-day course of caspofungin costs around $1,250. Fluconazole? About $150. That’s why hospitals often switch patients from echinocandins to oral azoles once they’re stable.
When to Use Which?
There’s no one-size-fits-all. Here’s how doctors decide:
- Invasive candidiasis (bloodstream infection): Start with echinocandin in ICU patients. Use fluconazole if the patient is stable and the infection is likely caused by Candida albicans.
- Invasive aspergillosis: Voriconazole is the gold standard. It’s the only azole with proven survival benefit-21% lower death rate than amphotericin B. But it causes visual disturbances in 38% of patients: blurred vision, light sensitivity, color changes. These are temporary, but scary if you don’t expect them.
- Prophylaxis (prevention): Posaconazole is preferred for high-risk patients like those with leukemia. It’s taken as a tablet or liquid. Trough levels must be checked-below 1 μg/mL, and it won’t work.
- Chronic or mild infections: Fluconazole remains the go-to for vaginal yeast, oral thrush, or skin infections that don’t respond to topical treatments.
Safety First: What You Must Monitor
Antifungals aren’t harmless. Even the safest ones need watching.
For azoles:
- Check liver enzymes before starting, then weekly for the first month, then every 4 weeks.
- Stop the drug if ALT or AST rises above 5 times the normal limit.
- Test for QT prolongation before starting voriconazole or posaconazole-especially if the patient is on macrolide antibiotics. Cases have been reported where QT intervals ballooned past 500ms, risking sudden cardiac arrest.
- Monitor drug levels for voriconazole and posaconazole. About 37% of patients need dose changes to hit the right blood concentration.
For echinocandins:
- Only adjust dose for severe liver failure (Child-Pugh Class C).
- Watch for infusion reactions-flushing, fever, or low blood pressure during the first few minutes. Slowing the drip often fixes it.
- No routine blood monitoring needed, but keep an eye on kidney function anyway.
Don’t mix antifungals with steroid creams like clotrimazole-betamethasone. The steroid can make fungal skin infections worse. It’s a common mistake in dermatology clinics.
Pregnancy and Special Populations
Azoles are Pregnancy Category D-meaning there’s clear evidence they can harm a developing fetus. Avoid them in pregnancy unless absolutely necessary. Echinocandins are Category C-risk can’t be ruled out, but data is limited. In pregnant women with life-threatening fungal infections, echinocandins are often preferred.
Older adults and those with kidney disease need lower doses of azoles. Echinocandins are mostly safe in kidney failure, since they’re not cleared by the kidneys.

The Future: Resistance and New Drugs
Fungi are fighting back. Azole resistance in Aspergillus fumigatus has jumped from 1.8% in 2012 to 8.4% in 2022. Why? Agricultural fungicides with the same chemical structure as medical azoles are spraying crops-and training fungi to survive.
That’s why new drugs are urgent. Rezafungin, a new echinocandin approved in March 2023, works with just one weekly injection. That’s a game-changer for long-term care. Olorofim, a brand-new class called an orotomide, showed 56% effectiveness in patients whose infections resisted all azoles. It’s in Phase 3 trials now.
But access remains unequal. Only 15% of low-income countries can reliably get second-line antifungals. In places like sub-Saharan Africa or rural Southeast Asia, fluconazole is often the only option-even when resistance is rising.
What Patients Say
Real-world experience tells a mixed story. On Drugs.com, fluconazole has a 6.8/10 rating. People say it works-but 42% report nausea. Caspofungin scores 5.2/10. Patients hate the IV line, the cost, and the slow infusion. Nurses report that 92% of patients tolerate topical antifungals fine, with only minor skin irritation.
But when it comes to serious infections, the stakes are high. One patient in a 2022 survey said: "I was on voriconazole for 6 months. My vision was weird, my liver was shaky, but I lived. Without it, I wouldn’t have made it."
Antifungals aren’t glamorous. They’re not the first thing you think of when you hear "medicine." But for the 1.5 million people they save each year worldwide, they’re everything.
Are azoles safe for long-term use?
Azoles can be used long-term, but only with strict monitoring. Liver function tests must be checked every 4 weeks. Drug interactions are common and can be dangerous-especially with blood thinners, seizure meds, and cholesterol drugs. If you’re on azoles for more than 3 months, your doctor should review all your other medications. Never stop or change the dose without medical advice.
Can echinocandins be taken orally?
No, echinocandins are not absorbed through the gut and must be given intravenously. There are no oral forms available today. However, research is underway to develop an oral version. F2G Limited is working on a new orotomide that may offer similar benefits with pills, possibly by 2026.
Why is voriconazole preferred for aspergillosis?
Voriconazole has the best survival rate for invasive aspergillosis. Studies show it reduces death by over 20% compared to older drugs like amphotericin B. It penetrates lung tissue well and is active against most strains of Aspergillus. The downside is side effects: visual disturbances in nearly 40% of patients, liver stress, and many drug interactions. But when the infection is life-threatening, the benefits outweigh the risks.
Do antifungals cause resistance?
Yes, especially azoles. Overuse in agriculture and medicine has led to resistant strains of Aspergillus and Candida. In some regions, up to 10% of Aspergillus infections no longer respond to fluconazole or voriconazole. That’s why doctors now avoid azoles unless necessary, and why new drugs like rezafungin and olorofim are so important.
Is there a cheaper alternative to caspofungin?
For invasive candidiasis, fluconazole is much cheaper-about $150 for a week’s course versus $1,250 for caspofungin. But it’s only suitable if the infection is likely caused by Candida albicans and the patient is stable. In ICU patients with sepsis, switching to fluconazole too early can be deadly. The key is using the right drug for the right situation-not just the cheapest one.
What should I do if I miss a dose of my antifungal?
If you miss an oral azole dose, take it as soon as you remember-unless it’s close to the next dose. Then skip the missed one. Never double up. For IV echinocandins, contact your care team immediately. Missing a dose can allow the infection to rebound. Hospitals often use electronic alerts to prevent missed infusions.

Brian Furnell
December 20, 2025 AT 14:44Okay, so azoles are basically the Swiss Army knife of antifungals-cheap, oral, versatile-but they’re also the guy who shows up to a dinner party with 17 different medications in his pocket and expects everyone to know how they interact. The CYP3A4 inhibition is wild; it’s like giving your liver a full-body massage with a chainsaw. And don’t get me started on voriconazole’s visual side effects-38% of patients seeing the world like a neon Picasso painting? That’s not a side effect, that’s a psychedelic experience with a prescription label.
Meanwhile, echinocandins are the quiet, expensive bodyguard who never talks but always shows up when you need them. IV-only? Fine. $1,250 a week? Ouch. But zero renal toxicity and 340 drug interactions instead of 1,100? That’s not a feature-it’s a goddamn miracle in ICU settings. Why aren’t we pushing this harder in outpatient care? Because money, obviously.
Siobhan K.
December 21, 2025 AT 06:20Let’s be real-the entire antifungal landscape is a corporate chess game disguised as medicine. Azoles are old, cheap, and profitable for Big Pharma because they’ve been around since the Reagan era. Echinocandins? New, expensive, and patented. So of course hospitals switch patients from one to the other as soon as they’re stable-not because it’s safer, but because the insurance formulary says so.
And don’t even mention rezafungin’s weekly injection. That’s not innovation-it’s a cost-cutting measure wrapped in a lab coat. You’re trading daily pills for a weekly IV clinic visit. Who benefits? Not the patient. Not the nurse. Definitely not the person trying to work a 40-hour week while managing a fungal infection.
Orlando Marquez Jr
December 22, 2025 AT 09:59It is imperative to underscore that the pharmacokinetic profiles of azoles and echinocandins necessitate a highly individualized therapeutic approach, particularly in light of the heterogeneous nature of patient comorbidities and polypharmacy regimens. The inhibition of cytochrome P450 isoforms by azoles constitutes a clinically significant pharmacodynamic interaction that demands vigilant therapeutic drug monitoring and meticulous medication reconciliation. Furthermore, the renal excretion profile of echinocandins, while largely independent of renal function, does not preclude the necessity of baseline and periodic assessment of hepatic enzymes and electrolyte homeostasis.
As per the Infectious Diseases Society of America guidelines, echinocandins remain the preferred first-line agents for invasive candidiasis in critically ill patients, a recommendation grounded in robust clinical trial data and meta-analytic evidence. However, the economic burden associated with these agents must be contextualized within broader healthcare resource allocation frameworks, particularly in resource-constrained environments.
Stacey Smith
December 24, 2025 AT 07:48US hospitals are still using 1980s-era protocols because they’re cheap. Meanwhile, Europe and Canada are already switching to rezafungin. We’re letting patients die because someone’s spreadsheet says fluconazole is ‘good enough.’
Ben Warren
December 25, 2025 AT 10:08There is a systemic failure in modern medical education regarding antifungal stewardship. The overreliance on azoles, particularly fluconazole, is not merely a pharmacological oversight-it is a moral lapse. Physicians are trained to prioritize cost over clinical outcome, and patients are treated as variables in a reimbursement algorithm rather than individuals with complex physiological systems. The fact that 12% of patients on long-term azole therapy develop hepatotoxicity, while echinocandins-superior in safety and specificity-remain underutilized due to pricing structures, is not an accident. It is a consequence of profit-driven healthcare policy masquerading as evidence-based medicine.
Furthermore, the notion that ‘fluconazole is fine for stable patients’ ignores the reality that ‘stable’ is a transient state in immunocompromised populations. A patient may appear stable at Day 5, but fungal burden is insidious. Delaying echinocandin initiation until deterioration occurs is tantamount to therapeutic negligence. The IDSA guidelines are clear; adherence is not optional. It is obligatory.
And let us not ignore the global disparity: while affluent nations debate cost-benefit analyses, sub-Saharan Africa and Southeast Asia are forced to use fluconazole even when resistance exceeds 10%. This is not a medical crisis. It is a human rights violation.
Sandy Crux
December 26, 2025 AT 08:37Actually, the entire premise here is flawed. Azoles aren’t ‘workhorses’-they’re outdated, toxic relics of a pre-genomic era. And echinocandins? They’re not ‘powerhouses’-they’re just the latest pharmaceutical fad, funded by venture capital and pushed by reps with free lunches. The real breakthrough isn’t rezafungin or olorofim-it’s phage therapy and microbiome modulation. But no, we’d rather keep throwing expensive IVs at fungi while ignoring that most infections arise from dysbiosis in the first place.
Also, why is no one talking about the fact that agricultural azole use (in fungicides) is literally breeding super-fungi? The same chemical structures. The same enzyme targets. We’re farming resistance into existence. And then we wonder why our patients are dying. It’s not magic. It’s cause and effect. But sure, let’s keep blaming the patients for not taking their pills.
Hannah Taylor
December 27, 2025 AT 00:38ok so i read this and now i think the fda and big pharma are in cahoots. why? because they let azoles stay on the market even tho they kill people’s livers, but they make you pay 1500 for echinocandins?? and then they say ‘oh its for your safety’?? no. its for their profits. also i heard that the visual bugs from voriconazole are actually a government mind control experiment. why else would it be so common? i mean, 38%?? that’s not a side effect, that’s a program.
also, why do they say ‘no oral echinocandins’? what if they just don’t want us to have them? like, what if they’re hiding the pill form?? i think the truth is out there. and it’s in the 2023 FDA documents that got redacted.
Jason Silva
December 27, 2025 AT 22:21Bro. Azoles are basically the villain in this movie. 😵💫 Liver damage? Drug interactions? Vision going full Matrix? 😳 And echinocandins? The quiet hero who shows up in a lab coat and saves your life… but costs a mortgage. 💸
Also, rezafungin? ONE shot a week?? 🤯 That’s not medicine-that’s sci-fi. I’m so ready for this. Also, why isn’t this in Walmart yet???
And yes, the agricultural fungicides are making super-fungi. 🌱🦠 We’re basically training the enemy. Like, what were they thinking??
mukesh matav
December 28, 2025 AT 00:42Interesting read. I work in a rural clinic in India where fluconazole is the only option we have. We see a lot of candidiasis in diabetics. We know it’s not ideal, but we don’t have a choice. The cost of echinocandins is beyond our reach. We monitor liver enzymes as best we can, but labs are unreliable. Still, we save lives with what we have. It’s not perfect. But it’s something.
Peggy Adams
December 28, 2025 AT 12:25Why are we even talking about this? No one cares. I got a yeast infection once, used clotrimazole, it worked. Done. Why do we need all this science? Just give me a cream.
Sarah Williams
December 29, 2025 AT 04:58Thank you for writing this. So many people don’t realize how complex antifungals are. I’ve had a friend on voriconazole-vision weird, liver checks every week, meds adjusted constantly. She said it felt like playing Russian roulette with her body. But she’s alive. That’s the real win. We need more awareness, not just more drugs.
Theo Newbold
December 29, 2025 AT 08:25The data is clear: azoles are a liability. The 1,100+ drug interactions aren’t theoretical-they’re documented in adverse event databases. The fact that hospitals still default to fluconazole for non-severe cases without confirming Candida species is negligent. And the lack of routine trough level monitoring for voriconazole? That’s not standard of care-that’s malpractice waiting to happen. This post should be mandatory reading for every resident in infectious disease.
Jay lawch
December 29, 2025 AT 17:11Let me tell you something they don’t want you to know: antifungals are just the tip of the iceberg. The real enemy is the global monoculture of agriculture-fungicides sprayed on wheat, rice, and corn since the 1970s. These chemicals are identical to medical azoles. The fungi in your soil learned to survive. Then they jumped to humans. This isn’t evolution. This is sabotage. Who benefits? The same corporations that sell you the drugs and the pesticides. The FDA? They’re asleep. The WHO? They’re funded by the same pharma giants. This is a controlled pandemic. And we’re being fed lies about ‘stewardship’ and ‘cost-benefit’ while the super-fungi multiply. Wake up.
Christina Weber
December 31, 2025 AT 03:45There is a critical omission in this analysis: the distinction between pharmacokinetic and pharmacodynamic drug interactions. While the CYP3A4 inhibition by azoles is well-documented, the clinical significance of these interactions must be evaluated not merely by the number of listed interactions, but by the magnitude of the area under the curve (AUC) increase, the half-life prolongation, and the therapeutic index of the co-administered agents. For instance, a 2.5-fold increase in cyclosporine AUC may be clinically insignificant in a stable transplant recipient, whereas a 1.8-fold increase in phenytoin may precipitate toxicity in an elderly patient with borderline renal function.
Furthermore, the assertion that echinocandins are ‘gentler’ on the kidneys is misleading. While they do not exhibit nephrotoxicity in the classical sense, they are associated with transient elevations in serum transaminases and, in rare cases, anaphylactoid infusion reactions that may precipitate acute kidney injury via hypotensive mechanisms. The 1.2% incidence cited is statistically valid but clinically underreported in observational cohorts.
Finally, the reference to ‘topical antifungals’ as universally benign is incorrect. The combination of antifungal and corticosteroid agents, such as clotrimazole-betamethasone, is contraindicated in tinea corporis due to the immunosuppressive effects of the steroid, which may facilitate deep fungal invasion-particularly in patients with undiagnosed diabetes or immunodeficiency. This is not a ‘common mistake’-it is a preventable iatrogenic harm.
Stacey Smith
December 31, 2025 AT 12:54And yet, we still let primary care docs prescribe fluconazole for ‘possible yeast’ without a culture. That’s not medicine. That’s guesswork with a stamp.