Calan (Verapamil) vs Alternatives: Drug Selector Tool
Recommended Medications for Your Profile
Detailed Comparison
Decision Tree Guidance
When doctors prescribe Calan (Verapamil) it’s because they need a reliable calcium channel blocker that can lower blood pressure, relieve angina, and control certain arrhythmias. But the market offers several other options, and patients often wonder which drug fits their lifestyle, health profile, and budget best. This guide walks you through the most common alternatives, highlights key differences, and gives you a practical checklist to decide what’s right for you.
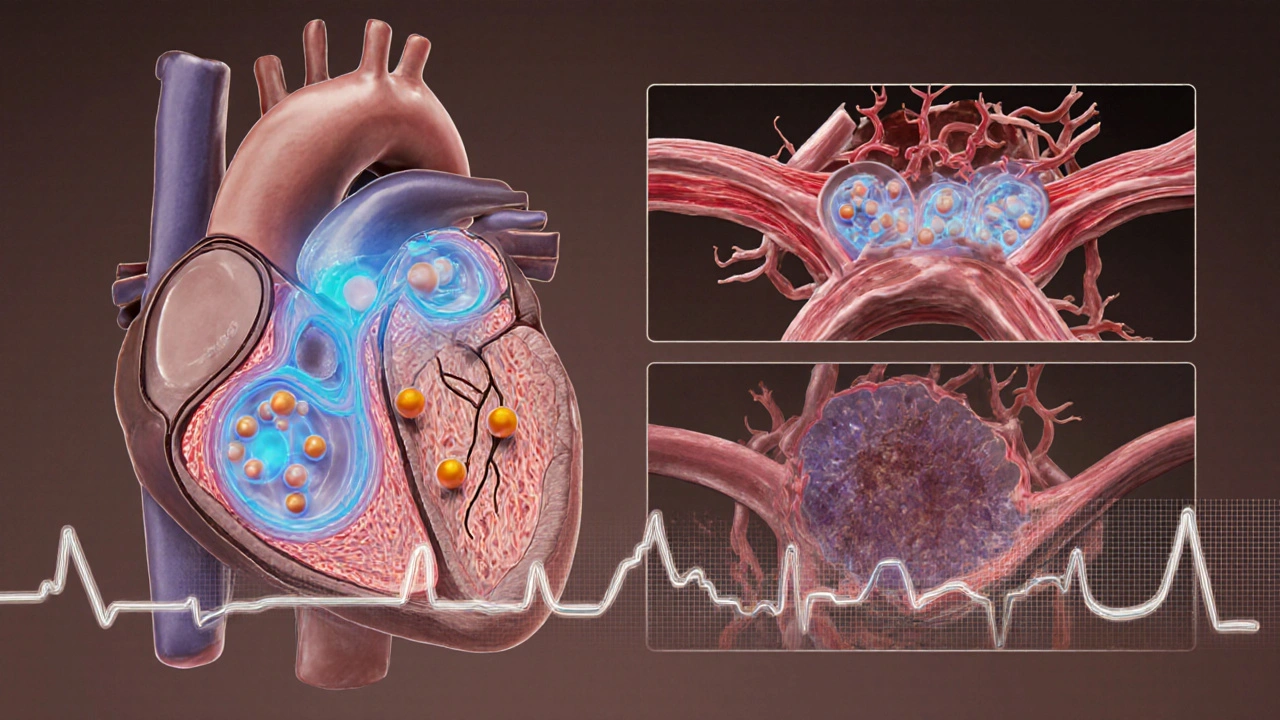
How Verapamil Works
Verapamil blocks L‑type calcium channels in the heart and blood‑vessel walls. By limiting calcium entry, it relaxes smooth muscle, reduces arterial resistance, and slows the electrical conduction through the AV node. This triple action makes it useful for three main indications: high blood pressure (hypertension), chest pain caused by reduced blood flow (angina), and rapid heart rhythms such as atrial fibrillation.
When to Look at Alternatives
Even though Verapamil is effective, several factors might push you toward another drug:
- Side‑effect profile - Some patients experience constipation, swelling, or a slow heart rate that can be uncomfortable.
- Drug interactions - Verapamil interacts with several antibiotics, antifungals, and statins, which can complicate multi‑drug regimens.
- Specific condition focus - If your primary issue is high blood pressure without heart rhythm concerns, a pure antihypertensive may be simpler.
- Cost and insurance coverage - Generic versions exist, but some alternatives are covered more broadly by formularies.
Below we compare the most frequently considered alternatives, grouped by drug class.
Comparison Table
| Drug (Brand) | Class | Typical Uses | Usual Dose Range | Common Side Effects | Onset of Action |
|---|---|---|---|---|---|
| Calan (Verapamil) | Calcium Channel Blocker (non‑DHP) | Hypertension, Angina, Atrial Fibrillation | 80‑480mg/day (divided) | Constipation, edema, bradycardia | 30‑60min (oral) |
| Norvasc (Amlodipine) | Calcium Channel Blocker (DHP) | Hypertension, Chronic Angina | 2.5‑10mg/day | Swelling, flushing, dizziness | 4‑6hrs |
| Cardizem (Diltiazem) | Calcium Channel Blocker (non‑DHP) | Hypertension, Angina, Rate control in AF | 120‑360mg/day | Headache, edema, constipation | 1‑2hrs |
| Procardia (Nifedipine) | Calcium Channel Blocker (DHP) | Hypertension, Severe Angina | 30‑90mg/day (extended‑release) | Facial flushing, headache, tachycardia | 30‑60min |
| Lopressor (Metoprolol) | Beta‑Blocker | Hypertension, Angina, Heart Failure, AF rate control | 25‑200mg/day | Fatigue, cold extremities, depression | 1‑2hrs |
| Zestril (Lisinopril) | ACE Inhibitor | Hypertension, Heart Failure, Post‑MI care | 5‑40mg/day | Cough, hyperkalemia, dizziness | 1‑2hrs |
Pros and Cons of Each Option
- Calan (Verapamil)
- Pros: strong evidence for rhythm control in atrial fibrillation; works well for angina.
- Cons: can significantly slow heart rate; constipation is common.
- Norvasc (Amlodipine)
- Pros: minimal effect on heart rate; once‑daily dosing.
- Cons: peripheral edema can be troublesome; less effective for arrhythmia control.
- Cardizem (Diltiazem)
- Pros: balances blood‑pressure reduction with moderate heart‑rate control; useful in both hypertension and angina.
- Cons: still carries constipation risk; interacts with many CYP3A4 drugs.
- Procardia (Nifedipine)
- Pros: rapid onset, good for acute angina episodes.
- Cons: can cause reflex tachycardia, making it a poor choice for patients with existing arrhythmias.
- Lopressor (Metoprolol)
- Pros: well‑studied for heart‑failure mortality benefit; helps with anxiety‑related palpitations.
- Cons: may worsen asthma, can cause fatigue.
- Zestril (Lisinopril)
- Pros: protects kidneys in diabetic patients; low incidence of metabolic side effects.
- Cons: dry cough is a frequent reason for discontinuation; not ideal for patients with high potassium.

Choosing the Right Drug - A Practical Decision Tree
- Identify your primary indication:
- If you need rhythm control for atrial fibrillation, Verapamil or Diltiazem are the only calcium‑channel options that directly affect AV‑node conduction.
- If you only need blood‑pressure lowering, consider Amlodipine, Lisinopril, or Metoprolol based on comorbidities.
- Review your existing medication list for possible interactions. Verapamil is a strong CYP3A4 inhibitor; avoid combining with certain statins (e.g., simvastatin) unless dose‑adjusted.
- Check for contraindications:
- Severe heart‑block or sick‑sinus syndrome → avoid Verapamil and Diltiazem.
- Asthma or severe COPD → avoid non‑selective beta‑blockers like Metoprolol.
- History of chronic cough → consider alternatives to Lisinopril.
- Factor in side‑effect tolerance:
- If constipation is a deal‑breaker, lean toward Amlodipine or Lisinopril.
- If swelling is unacceptable, avoid DHP‑type calcium blockers.
- Discuss cost with your pharmacist. Generics of Verapamil, Amlodipine, and Metoprolol are often the cheapest; brand‑only formulations may add expense.
Key Takeaways
- Verapamil shines when you need both blood‑pressure control and atrial‑fibrillation rate management.
- DHP calcium blockers like Amlodipine and Nifedipine are better for pure hypertension or angina without rhythm effects.
- Beta‑blockers such as Metoprolol offer mortality benefits in heart failure but may cause fatigue.
- ACE inhibitors (e.g., Lisinopril) protect kidneys but can provoke a cough.
- Always match the drug’s side‑effect profile and interaction risk to your personal health picture.
Frequently Asked Questions
Can I switch from Verapamil to Amlodipine without a washout period?
Because both are calcium‑channel blockers but work on different sub‑types, a short overlap is usually safe. However, doctors often pause Verapamil for 24‑48hours to monitor blood‑pressure changes before starting Amlodipine.
Is Verapamil suitable for patients with heart‑failure?
Verapamil can worsen systolic heart‑failure because it reduces contractility. For reduced‑ejection‑fraction heart‑failure, doctors prefer beta‑blockers or ACE inhibitors.
Why does Verapamil cause constipation?
The drug relaxes smooth muscle not only in blood vessels but also in the gastrointestinal tract, slowing transit and leading to constipation. Increasing fiber intake or using a mild laxative can help.
How does the side‑effect profile of Diltiazem differ from Verapamil?
Both are non‑DHP blockers, but Diltiazem has a slightly weaker effect on the AV node, so it’s less likely to cause severe bradycardia. Its constipation rate is also a bit lower, though headache and edema remain common.
Can Verapamil be used during pregnancy?
It’s classified as Category C, meaning animal studies showed risk but human data are limited. Doctors usually reserve it for pregnant patients only when benefits clearly outweigh potential hazards.
Which drug is best for a patient with both hypertension and chronic migraines?
Amlodipine may help because it lowers blood pressure without causing significant central nervous system effects, and it’s less likely to trigger migraine aura compared to some beta‑blockers.
What monitoring is required after starting Verapamil?
Doctors usually check blood pressure and heart rate within the first week, then repeat ECG after two weeks to ensure the QT interval isn’t prolonged. Kidney and liver function tests are also advised for long‑term use.


Taryn Esses
October 5, 2025 AT 23:33Verapamil can be handy, but watch the constipation.
Albert Lopez
October 6, 2025 AT 21:46The exposition excels in delineating pharmacodynamic nuances; however, the prose occasionally drifts into pedantic territory. One must appreciate the rigor of the side‑effect matrix, yet the omission of real‑world adherence data feels like an oversight. Moreover, the decision‑tree, while aesthetically pleasing, could benefit from probabilistic weighting. In sum, the guide is commendably thorough but not without its scholarly pretensions.
Halle Redick
October 7, 2025 AT 17:13The guide gives a solid overview of Verapamil’s role in heart health. It explains how the drug slows the AV node and eases blood‑vessel tension. For patients juggling hypertension and occasional atrial fibrillation, that dual action is a real plus. The comparison table nicely lines up side‑effects so you can see that constipation is more common with Verapamil than with Amlodipine. Meanwhile, Amlodipine’s swelling issue can be a deal‑breaker for those prone to edema. The section on beta‑blockers reminds us that Metoprolol helps heart‑failure mortality but may worsen asthma. I also like the decision‑tree format; it walks you through “what’s most important to you?” step by step. If rhythm control is your primary goal, the guide correctly points you toward Verapamil or Diltiazem. On the other hand, pure blood‑pressure control without rhythm concerns can be met with Lisinopril or ACE inhibitors. The cost note is practical because generic Verapamil and Amlodipine are cheap, but brand‑only forms can add up. One subtle point is the drug‑interaction warning about CYP3A4; many patients don’t realize statins can clash. The FAQ section clears up common myths, like the idea that Verapamil is safe in all heart‑failure cases-it isn’t. It even mentions pregnancy categorisation, which is often omitted in quick drug charts. Overall the guide feels balanced, giving you pros and cons without pushing a single brand. Bottom line: read the side‑effect list, match it to your comorbidities, and discuss the choice with your cardiologist.
Erica Harrington
October 8, 2025 AT 07:06Great rundown! I love how the guide keeps the focus on patient‑centered choices. It’s refreshing to see encouragement to talk with your doctor rather than just self‑prescribing. The practical tips on monitoring heart rate are spot on. Keep the momentum going – knowledge really does empower.
Patricia Mombourquette
October 9, 2025 AT 10:53this article is fine but i cant stand the extra words. verapamil cause constipation its a fact. amlodipine cause swelling its known. stop beating around the bush.
karl lewis
October 10, 2025 AT 00:46While I respect the brevity, let us not reduce the discourse to mere bullet points. A lazy reiteration risks overlooking the philosophical underpinnings of therapeutic choice. One must contemplate not only efficacy but also the existential burden of side‑effects upon the patient’s daily life. In the grand tapestry of medicine, each nuance contributes to the overall narrative.
Amy Martinez
October 10, 2025 AT 14:40Reading through this made me think of the countless evenings patients spend worrying about a pill’s after‑taste. The vivid colors of the side‑effect table paint a picture of real lives affected. I appreciate the empathy woven into the FAQ – it feels like a warm hand reaching across the screen. Let’s keep sharing stories, because behind every drug name is a human heart.
Josh Grabenstein
October 11, 2025 AT 04:33Sure the guide looks nice but have you considered that pharma labs might be pulling strings behind the scenes? The data you see could be filtered
trust the hidden agenda. It’s not just about constipation, it’s about control.
Nidhi Jaiswal
October 11, 2025 AT 18:26The comparison is decent yet simplistic. A more rigorous statistical analysis would elevate it. Patients deserve clearer guidance, not just a list of pros and cons.
Sunil Sharma
October 12, 2025 AT 08:20Thanks for the feedback! Let’s add some real‑world numbers to make the guide even more useful. A quick glance at prevalence rates can help anyone decide faster. Happy to collaborate on that update.
Jenn Zee
October 12, 2025 AT 22:13It is evident that the author has undertaken an exhaustive survey of the pharmacologic landscape, yet the exposition still suffers from a certain lack of aristocratic flair. One must acknowledge the meticulous tabulation of side‑effects, but the narrative voice remains unsatisfactorily pedestrian. In the realm of medical literature, a touch of eloquence can transform a mere pamphlet into a masterpiece of persuasive advocacy. Moreover, the decision‑tree, while functional, could be embellished with nuanced probabilistic thresholds, thereby granting the reader a more sophisticated decision‑making apparatus. The omission of bespoke patient anecdotes, however, leaves a void where lived experience might have fortified the argument. It is not merely a question of data, but of the human story that undergirds each dosage adjustment. Consequently, I would implore the author to contemplate a more florid style, interweaving clinical precision with literary poise, to truly capture the reader’s imagination and trust.
don hammond
October 13, 2025 AT 12:06Oh wow, a guide about drugs? How original 🙄. I guess we’re all just thrilled to read another table of side‑effects. 🎉 But hey, at least there’s an emoji for everything, right?
Ben Rudolph
October 14, 2025 AT 02:00While sarcasm is entertaining, it detracts from the seriousness of medication safety. Readers may miss crucial warnings amid the jokes. Let’s keep the tone respectful and focused on the facts.