When your blood clots too easily, it can lead to dangerous blockages in your legs, lungs, or brain. But if it doesn’t clot enough, even a small cut can become life-threatening. Finding the right balance is the core challenge of anticoagulation therapy - and it’s not as simple as just taking a pill.
What Exactly Are Clotting Disorders?
Clotting disorders aren’t one condition - they’re a group of problems where your body either makes too many clots or can’t stop them from forming. The most common ones include deep vein thrombosis (DVT), where clots form in the deep veins of your legs, and pulmonary embolism (PE), where those clots break loose and travel to your lungs. People with atrial fibrillation - an irregular heartbeat - are also at high risk because blood pools in the heart and can clot there, leading to strokes.
These aren’t rare. About 1 in 1,000 adults develops a blood clot each year. And for those with atrial fibrillation, the risk of stroke jumps five times higher than in people with normal heart rhythms. That’s why doctors reach for anticoagulants - blood thinners - to reduce that risk. But these drugs don’t actually thin your blood. They interfere with the proteins and enzymes that make clots form.
INR: The Old-School Way to Monitor Blood Thinners
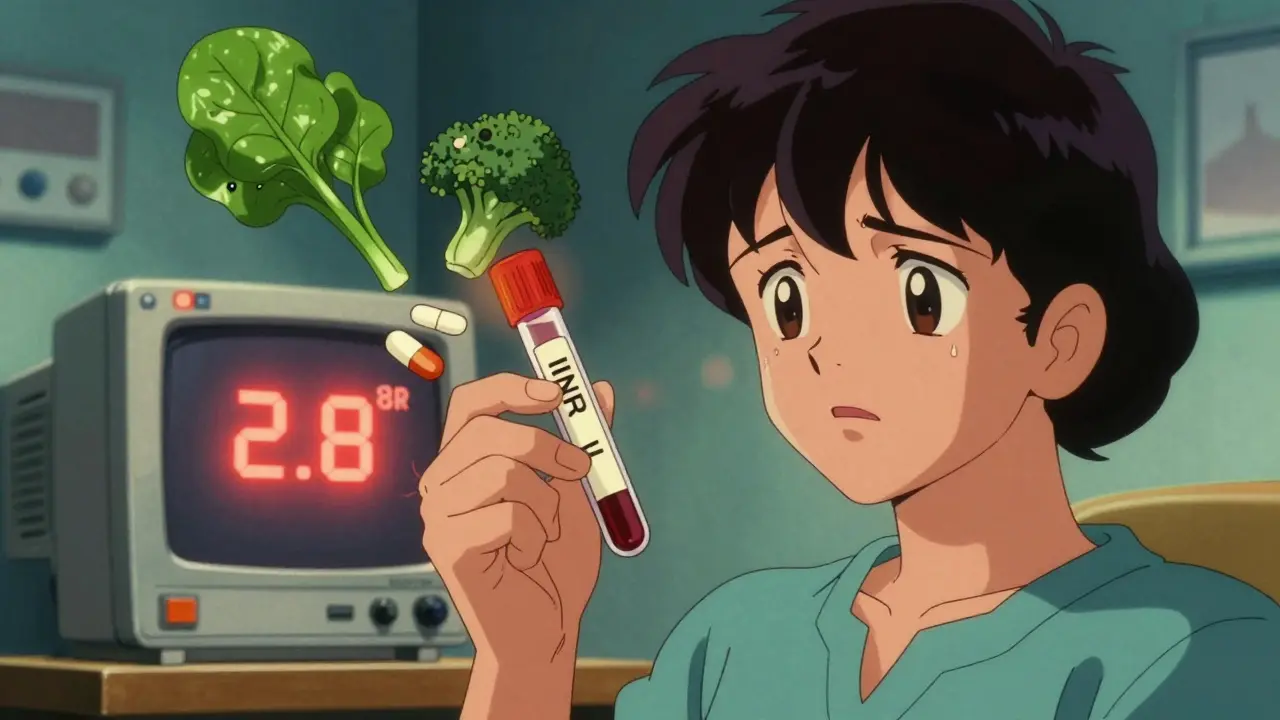
For decades, warfarin was the only option. It’s been around since the 1940s, originally developed as rat poison before doctors realized it could save human lives. Warfarin works by blocking vitamin K, which your body needs to make clotting factors. But here’s the catch: vitamin K is in leafy greens, broccoli, and even some oils. That means your diet can change how well warfarin works.
To make sure you’re getting the right dose, you need regular blood tests to check your INR - International Normalized Ratio. This number tells doctors how long it takes your blood to clot compared to a standard. For most people, the target is 2.0 to 3.0. Too low, and you’re still at risk for clots. Too high, and you’re at risk for bleeding.
Getting that number right is hard. Studies show only about 70% of patients on warfarin stay in the ideal range most of the time. That means nearly 1 in 3 people are either under- or over-treated. Weekly blood draws are common when starting, then every few weeks once stable. Some people need genetic testing because variations in the CYP2C9 and VKORC1 genes can make them sensitive to tiny doses - or require much higher amounts than average.
DOACs: The New Generation of Blood Thinners
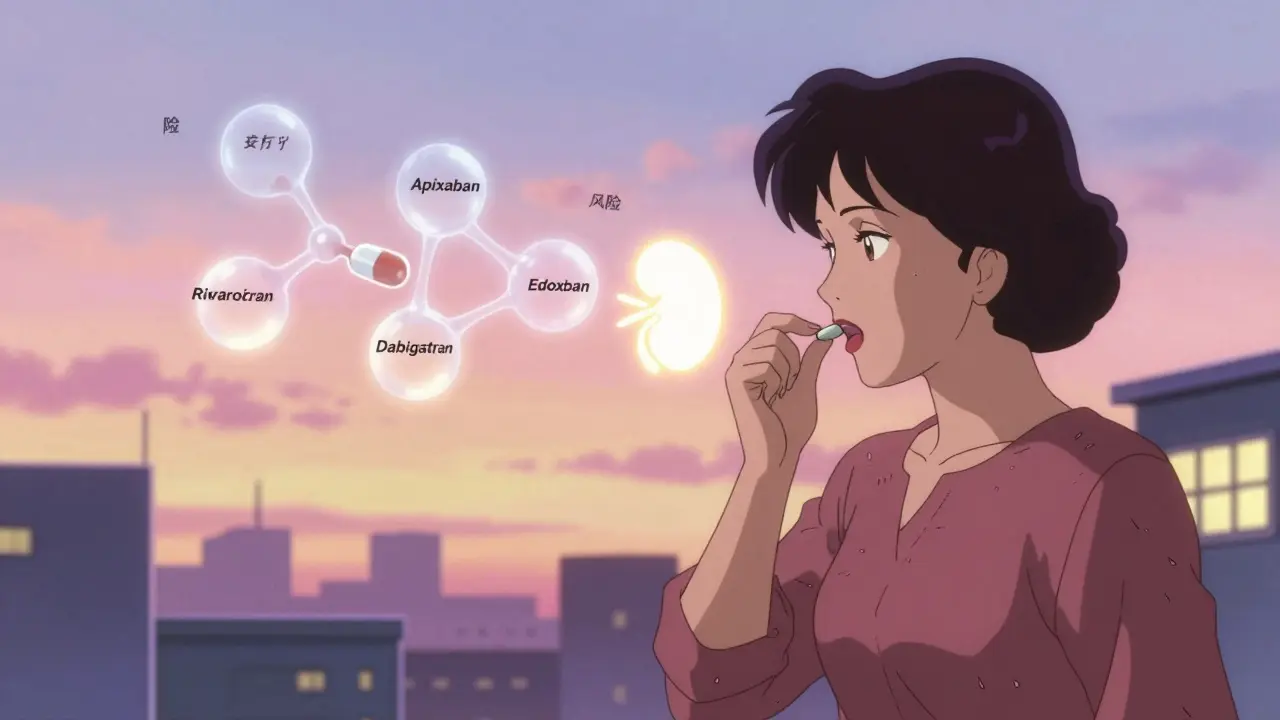
Between 2010 and 2015, four new drugs hit the market: apixaban (Eliquis), rivaroxaban (Xarelto), dabigatran (Pradaxa), and edoxaban (Savaysa). These are called direct oral anticoagulants, or DOACs. They work differently than warfarin. Instead of blocking vitamin K, they target specific clotting proteins - either factor Xa or thrombin.
The biggest advantage? No routine blood tests. No worrying about broccoli. No weekly finger pricks. You take the same dose every day, and that’s it. For most people with atrial fibrillation and no mechanical heart valves, DOACs are now the first choice, according to guidelines from the American Heart Association and American College of Cardiology.
They’re also safer in some ways. The ARISTOTLE trial showed apixaban reduced major bleeding by 31% compared to warfarin. And in real-world use, DOACs cut stroke risk by 60-70% in high-risk patients - just like warfarin - but with fewer brain bleeds and less need for hospitalization due to bleeding.
But DOACs Aren’t Perfect
Here’s the downside: if something goes wrong - like a bad fall or internal bleeding - you can’t just check a number to see how much drug is in your system. There’s no INR equivalent. Doctors can order specialized blood tests, but they’re expensive, slow, and not always available.
Reversal agents exist, but they’re costly. Idarucizumab (Praxbind) reverses dabigatran, but one dose costs about $5,000. Andexanet alfa reverses apixaban and rivaroxaban, but one dose runs close to $18,000. That’s not something most hospitals stock on the shelf. And even if they do, it’s not a magic fix - it only works if given quickly.
Another issue: kidney function. DOACs are cleared through the kidneys. If your kidneys aren’t working well - common in older adults - the drug can build up and increase bleeding risk. That’s why doctors check your creatinine clearance before starting and every 6 to 12 months after. Some DOACs aren’t approved at all if your kidney function drops below 15-30 mL/min.
And then there’s the cost. Warfarin costs $4 to $30 a month. DOACs? $350 to $550. Even with insurance, copays can hit $200 or more. A 2023 study found nearly 3 out of 10 Medicare patients stopped taking DOACs within a year because they couldn’t afford them.
When Warfarin Still Wins
Despite all the hype around DOACs, warfarin hasn’t disappeared. It’s still the only option for people with mechanical heart valves. DOACs simply don’t work well enough in those cases - the risk of clotting on the valve is too high. Same goes for moderate-to-severe mitral stenosis.
Warfarin also has an edge in certain cancers. For people with gastrointestinal or prostate cancer who develop clots, low-molecular-weight heparin (like Lovenox) is still preferred over DOACs because DOACs increase bleeding risk by 55% in these cases, according to the Hokusai VTE Cancer trial.
And if you’re on a tight budget, warfarin is hard to beat. Plus, if you bleed, doctors know exactly what to do: give you vitamin K or fresh frozen plasma. It’s old, but reliable.
Safety First: Bleeding Risks and What to Watch For
All anticoagulants increase bleeding risk. That’s not a side effect - it’s the point. But knowing the signs can save your life.
Watch for:
- Bleeding that won’t stop after 10 minutes
- Unusual bruising, especially large or painful ones
- Bloody or black stools
- Red or pink urine
- Severe headaches, dizziness, or vision changes (could mean brain bleed)
- Swelling or pain in joints (could mean internal bleeding)
One study found that 78% of people on anticoagulants notice more bruising. That’s normal. But if you’re bruising easily without injury, or if bruises grow bigger, call your doctor.
INR above 4.0 increases major bleeding risk by 2.5 times. That’s why some patients on warfarin get emergency care when their INR spikes. With DOACs, you don’t have that safety net - so you need to be even more careful.
What About Procedures and Surgery?
If you need a dental extraction, colonoscopy, or surgery, you’ll need to pause your blood thinner. But how long? That’s where warfarin and DOACs differ.
For warfarin, doctors often stop it 5 days before surgery and use heparin shots as a bridge. That’s risky - bridging increases bleeding by 20-30%. With DOACs, you usually just skip 1 or 2 doses. For most procedures, holding for 24 to 48 hours is enough, especially if your kidneys are working well.
But here’s the catch: if you’re on a DOAC and need spinal anesthesia or an epidural, your doctor might delay it. There’s a small but real risk of spinal hematoma - a dangerous bleed around the spine. The FDA has boxed warnings for this with all DOACs.
Real People, Real Choices
A nurse named Juliet, featured in a 2023 patient education guide, ignored her own symptoms of a blood clot because she was focused on her child. She ended up with a pulmonary embolism. She’s not alone. Many patients, even healthcare workers, delay care because they don’t recognize the signs.
On Reddit, 68% of 142 anticoagulant users said they switched from warfarin to DOACs because they hated the blood tests. One user wrote: “I used to dread my weekly INR check. Now I just take my pill and forget about it.” But another said: “I stayed on warfarin because I can’t afford Eliquis. My copay is $25. His is $400.”
And then there’s the GI bleeding. A 2022 survey found 41% of rivaroxaban users reported stomach issues - nausea, cramps, even vomiting blood. Apixaban had the lowest GI bleeding rate among DOACs. That’s why some doctors now prefer it as a first-line choice.
The Future: New Drugs and Smarter Care
Things are changing fast. In November 2023, the FDA approved milvexian - a new drug that targets factor XIa, a protein involved in clotting but not in stopping bleeding. Early trials show it prevents clots just as well as apixaban but with 22% less bleeding. That’s huge.
Researchers are also testing RNA-based drugs like fitusiran, which lowers antithrombin levels. And AI tools are being trained to predict who’s most likely to bleed based on age, kidney function, medications, and even genetic markers. One model in Nature Medicine predicted bleeding risk with 82% accuracy.
But for now, the choice comes down to this: Do you want convenience and less monitoring (DOACs), or lower cost and better reversal options (warfarin)? For most people, DOACs win. But not everyone can afford them. Not everyone’s kidneys can handle them. And not everyone’s condition is safe for them.
There’s no one-size-fits-all. Your doctor needs to know your age, kidney function, other meds, lifestyle, and even your budget. Because the best anticoagulant isn’t the newest one - it’s the one you can take safely, consistently, and without fear.
What If You Miss a Dose?
Missing a dose of warfarin? It’s not an emergency. Your INR will drop slowly. But with DOACs, timing matters. If you miss a morning dose of apixaban, take it as soon as you remember - but only if it’s within 6 hours. If it’s been longer, skip it and take your next dose at the regular time. Never double up.
For rivaroxaban, if you miss your dose, take it as soon as you remember on the same day. If it’s already the next day, skip it. Don’t take two at once.
Always check your drug’s specific instructions. A missed dose on a DOAC can mean your blood isn’t protected for hours - long enough for a clot to form.
Final Thoughts: It’s About Control, Not Just Pills
Anticoagulation isn’t just about taking a pill. It’s about understanding your body, knowing your risks, and being honest with your doctor. It’s about choosing a drug you can stick with - whether that’s because of cost, convenience, or side effects.
Don’t let fear stop you. Blood clots kill. But so can uncontrolled bleeding. The goal isn’t to eliminate risk - it’s to manage it wisely. And with the right information, you can do exactly that.
What does INR stand for, and why is it important?
INR stands for International Normalized Ratio. It’s a standardized way to measure how long your blood takes to clot. For people on warfarin, keeping INR between 2.0 and 3.0 means the drug is working right - low enough to prevent clots, high enough to avoid dangerous bleeding. Outside that range, your risk goes up significantly.
Can I switch from warfarin to a DOAC on my own?
No. Switching from warfarin to a DOAC requires careful planning. Your doctor must stop warfarin, wait for your INR to drop below 2.0, then start the DOAC. Doing this on your own can lead to dangerous gaps in protection or overdose. Always follow medical guidance.
Are DOACs safer than warfarin for older adults?
Generally, yes - but with caveats. DOACs reduce the risk of brain bleeds and don’t require frequent blood tests, which is helpful for seniors. But if kidney function declines with age, DOACs can build up in the body. Doctors must check creatinine clearance regularly. Apixaban is often preferred in older patients because it has the lowest bleeding risk among DOACs.
What should I do if I start bleeding while on a blood thinner?
Call 911 or go to the ER immediately if you have uncontrolled bleeding, blood in stool or urine, severe headache, confusion, or weakness on one side of your body. Don’t wait. For minor bleeding like nosebleeds or cuts, apply pressure and call your doctor. Never ignore signs of internal bleeding.
Can I drink alcohol while taking anticoagulants?
Moderate alcohol - one drink a day - is usually okay. But heavy drinking increases bleeding risk and can interfere with how warfarin works. With DOACs, alcohol doesn’t directly interact, but it can irritate your stomach lining and raise the chance of GI bleeding. Avoid binge drinking and always talk to your doctor about your habits.
Why can’t I take aspirin with my blood thinner?
Aspirin also thins the blood by affecting platelets. Combining it with warfarin or a DOAC greatly increases bleeding risk - especially in the stomach and brain. Only take aspirin if your doctor specifically prescribes it for heart protection. Never self-medicate with OTC pain relievers while on anticoagulants.
How long do I need to stay on anticoagulants?
It depends. For a first blood clot caused by surgery or injury, 3 to 6 months is typical. If the clot happened without a clear cause (unprovoked), doctors often recommend lifelong treatment - especially if your bleeding risk is low. For atrial fibrillation, it’s usually lifelong unless your stroke risk drops significantly. Your doctor will reassess annually.
Next Steps: What to Do Today
If you’re on an anticoagulant, here’s what to do now:
- Know which drug you’re taking - and why.
- Check your kidney function if you’re on a DOAC - ask your doctor for your creatinine clearance number.
- Write down the signs of bleeding and show them to a family member.
- Keep a list of all your meds, including supplements - even garlic or fish oil can interact.
- If you’re on warfarin, ask if your INR has been in range over the last 6 months. If not, ask what you can do to improve it.
- If you’re on a DOAC and can’t afford it, ask about patient assistance programs. Many manufacturers offer them.
Anticoagulation isn’t a one-time decision. It’s an ongoing conversation with your health. Stay informed. Stay vigilant. And don’t let fear keep you from living - just make sure you’re doing it safely.