When you’re managing heart disease, it’s common to take several medications at once. Maybe it’s a beta blocker for your blood pressure, a statin for cholesterol, a diuretic to reduce swelling, and an anticoagulant to prevent clots. But here’s the thing: combining multiple heart medications isn’t just adding pills-it’s adding risk. Every new drug you take doesn’t just work on its own. It talks to the others. And sometimes, those conversations turn dangerous.
Why Heart Medications Are Especially Risky to Mix
Your heart doesn’t just need one thing to stay healthy. It needs a whole team of drugs working together-sometimes in delicate balance. But that balance is easy to disrupt. The liver and kidneys process most heart medications, and when two or more drugs are processed by the same pathway, they can compete, slow each other down, or speed things up in ways that change how much of each drug actually reaches your bloodstream. A 2019 study found that nearly 8 out of 10 heart patients in a hospital setting were taking at least two drugs that could interact. And it gets worse with more pills. If you’re on four medications, your chance of a harmful interaction jumps to 38%. If you’re on seven or more? That number soars to 82%. That’s not a small risk. That’s a major health threat. Older adults are especially vulnerable. About 40% of high-risk interaction cases involve people over 65. And it’s not just about age. Many older patients have multiple conditions-diabetes, kidney disease, depression-all needing their own meds. The result? A medicine cabinet that looks like a pharmacy shelf.Unsafe Combinations You Need to Know
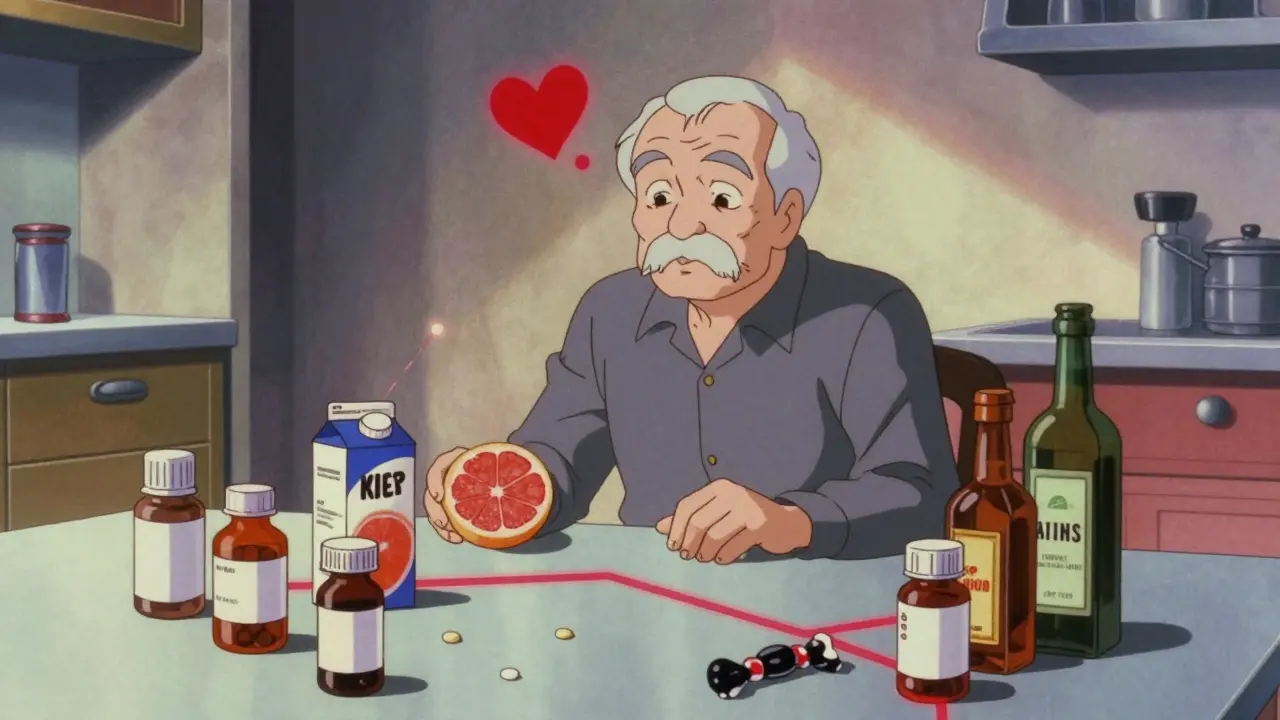
Some drug mixes are so dangerous they’re textbook examples of what not to do. Here are the ones that come up again and again in clinical reports and safety alerts.Grapefruit Juice + Statins
If you’re taking a statin like atorvastatin, simvastatin, or lovastatin, grapefruit juice isn’t just a healthy breakfast addition-it’s a ticking time bomb. Grapefruit blocks an enzyme called CYP3A4 that normally breaks down these drugs. Without it, your body can’t clear the statin. Levels build up fast. Just one quart a day can reduce enzyme activity by nearly half. That means your muscle tissue starts breaking down. You might feel extreme fatigue, dark urine, or muscle pain. Left unchecked, this can lead to rhabdomyolysis-a condition that can destroy muscle and cause kidney failure.St. John’s Wort + Heart Drugs
People turn to St. John’s wort for mild depression. It sounds natural, so it must be safe, right? Wrong. This supplement speeds up how quickly your body breaks down several heart medications, including some beta blockers and calcium channel blockers. That means the drug leaves your system too fast. Your blood pressure spikes. Your heart rate goes wild. The effect? Your treatment stops working, and you’re left with uncontrolled symptoms.Black Licorice + Blood Pressure Meds
Black licorice isn’t just candy. It contains glycyrrhizin, a compound that mimics aldosterone-a hormone that makes your body hold onto salt and water. That raises blood pressure. When you take it with beta blockers or calcium channel blockers, it fights against the medication’s purpose. The result? Your blood pressure doesn’t drop. It might even climb higher than before you started treatment. And it doesn’t take much. A few pieces a day over weeks can do the damage.Alcohol + Any Heart Medication
Alcohol doesn’t just affect your liver. It affects how your heart responds to drugs. It can lower blood pressure too much when mixed with antihypertensives, cause irregular rhythms when combined with antiarrhythmics, or make you dizzy and prone to falls when taken with diuretics. The National Institute on Alcohol Abuse and Alcoholism says alcohol interacts with over 150 medications. For heart patients, that’s a recipe for emergency room visits.NSAIDs + Blood Pressure or Anticoagulant Drugs
Ibuprofen, naproxen, diclofenac-these common painkillers seem harmless. But they interfere with blood pressure meds like ACE inhibitors and ARBs. They reduce the drug’s ability to relax blood vessels. That means your pressure stays high. And if you’re on warfarin or apixaban? NSAIDs increase bleeding risk. A simple headache pill could turn into a stomach bleed or a stroke.Antidepressants + MAOIs + Certain Foods
If you’re on an MAOI antidepressant (like phenelzine or tranylcypromine), you can’t eat aged cheeses, cured meats, or even chocolate. These foods contain tyramine, which MAOIs can’t break down. That causes tyramine to build up, triggering a sudden, dangerous spike in blood pressure. This isn’t a mild headache. It’s a hypertensive crisis-possible stroke, heart attack, or death.What’s Actually Safe to Combine
Not all combinations are dangerous. In fact, many are carefully designed to work together. For example:- ACE inhibitors and diuretics are often paired to treat high blood pressure and heart failure.
- Aspirin and statins are routinely used together to reduce heart attack risk.
- Metoprolol and lisinopril are commonly combined for patients with post-heart attack care.

How to Protect Yourself
You don’t have to live in fear. But you do need to be smart.Use One Pharmacy
If you fill prescriptions at different places, no one sees the full picture. A single pharmacy can run all your meds through an interaction checker. They’ll catch things your doctor might miss-like that new OTC cold medicine you picked up at the grocery store.Do a Brown Bag Review
Once a year, or after any new prescription, bring everything you take to your doctor: pills, patches, gummies, herbal teas, supplements. Don’t leave anything out. That fish oil? That magnesium? That turmeric capsule? They all matter. Many patients don’t even think to mention them. But they can change how your heart meds work.Know Your High-Risk OTCs
These over-the-counter products are common culprits:- Antacids (like Tums or Maalox) can block absorption of heart drugs like digoxin or thyroid meds.
- First-gen antihistamines (like Benadryl) can prolong QT interval, raising risk of dangerous heart rhythms.
- Decongestants (like pseudoephedrine) raise blood pressure and heart rate.
- NSAIDs (like Advil) reduce the effect of blood pressure meds and increase bleeding.
Keep an Updated List
Write down every medication, including doses and times. Update it after every doctor visit. Carry it with you. If you end up in the ER, this list could save your life.Ask About Alternatives
If you’re on five or more medications, ask: “Is there a safer option?” Sometimes, switching from a statin that interacts with grapefruit to one that doesn’t (like pravastatin or rosuvastatin) makes a big difference. Or replacing an NSAID with acetaminophen for pain. Small changes, big safety wins.The Bigger Problem: Polypharmacy
Taking too many drugs isn’t just about interactions. It’s about burden. Side effects add up. Dizziness. Fatigue. Confusion. Falls. Memory problems. A 2023 study from the University of Rochester found that polypharmacy is linked to higher death rates in older adults with cancer-and heart patients are even more at risk. And here’s the emotional side: many people are afraid to stop taking meds. They think if their doctor prescribed it, it must be necessary. But sometimes, a drug was started years ago and never re-evaluated. That’s why deprescribing-safely removing unnecessary meds-is becoming a critical part of care. It’s not giving up. It’s getting smarter.
What’s Changing in 2026
Technology is catching up. Most electronic health records now flag potential interactions. But they still miss about 23% of serious ones because they don’t account for your unique genetics, diet, or kidney function. The future is personal. Researchers are now testing pharmacogenomic screening-checking your DNA to see how you metabolize drugs. Some people naturally break down statins slowly. Others clear beta blockers fast. Knowing that ahead of time means prescriptions can be tailored to your body, not just your diagnosis. For now, the best tool you have is awareness. And action.What to Do Today
1. Look at your medication list. Count how many you’re taking. 2. Check for grapefruit, alcohol, licorice, or OTC painkillers on that list. 3. Schedule a brown bag review with your doctor. 4. Ask: “Could any of these be interacting?” 5. Write down the answers. Keep them with your meds. You don’t need to be a pharmacist to protect your heart. You just need to ask the right questions-and not assume everything’s fine because it’s been that way for years.Can I still drink grapefruit juice if I take a statin?
No. If you’re taking atorvastatin, simvastatin, or lovastatin, grapefruit juice can cause dangerous drug buildup. Even one quart a day can block the enzyme that clears the statin from your body. This raises your risk of muscle damage and kidney failure. Switch to orange juice or skip citrus altogether. Pravastatin and rosuvastatin are safer options if you want to keep citrus in your diet.
Are herbal supplements safe with heart medications?
Many are not. St. John’s wort can make blood pressure and heart rhythm drugs ineffective. Turmeric can increase bleeding risk when taken with anticoagulants. Garlic and ginkgo can also thin the blood. Just because something is natural doesn’t mean it’s safe. Always tell your doctor about every supplement you take-even if you think it’s harmless.
Why do I need to bring all my meds to my doctor?
Because you might forget something. Or think it’s not important. But over-the-counter painkillers, sleep aids, vitamins, and even herbal teas can interact with your heart meds. A brown bag review lets your doctor see the full picture. It’s the only way to catch hidden risks that electronic systems miss.
Can I stop taking a heart medication if I feel fine?
Never stop without talking to your doctor. Even if you feel fine, the medication is likely doing its job behind the scenes. Stopping suddenly can cause rebound high blood pressure, chest pain, or irregular heartbeats. If you’re concerned about side effects or too many pills, ask about deprescribing. That’s when your doctor helps you safely reduce or stop meds that may no longer be needed.
How do I know if a drug interaction is happening to me?
Watch for new or worsening symptoms after starting a new drug: unexplained muscle pain or weakness, dizziness, confusion, unusual fatigue, swelling in your legs, irregular heartbeat, or bleeding that won’t stop. These aren’t normal side effects-they could be signs of a dangerous interaction. Call your doctor immediately if you notice them.
Is it safe to take over-the-counter pain relievers with heart meds?
It depends. NSAIDs like ibuprofen and naproxen can raise blood pressure and reduce the effectiveness of your heart meds. They also increase bleeding risk if you’re on blood thinners. Acetaminophen (Tylenol) is usually safer for occasional use. But even that can be risky if you have liver disease. Always check with your pharmacist or doctor before taking any OTC painkiller.
Can alcohol be safely consumed with heart medications?
It’s best to avoid alcohol entirely. It can lower blood pressure too much, cause dizziness, worsen heart rhythm problems, and increase liver damage when combined with statins. Even moderate drinking can interfere with how your body processes heart drugs. If you choose to drink, limit it to one drink a day and talk to your doctor first. But for many heart patients, zero is the safest number.

Joni O
January 17, 2026 AT 21:53OMG I just realized I’ve been drinking grapefruit juice with my statin for YEARS 😳 I thought it was ‘healthy’… I’m switching to orange juice today. Thanks for the wake-up call. My heart is literally screaming at me now.
Max Sinclair
January 18, 2026 AT 11:26This is one of the most well-researched and clinically relevant posts I’ve read in months. The breakdown of interactions-especially the NSAID and anticoagulant risk-is terrifyingly accurate. I’ve seen patients end up in the ER over ibuprofen they thought was ‘harmless.’ Always check with your pharmacist. They’re the unsung heroes of medication safety.
Praseetha Pn
January 18, 2026 AT 23:18Let me tell you something they don’t want you to know-Big Pharma doesn’t care if you live or die. They profit from you taking TEN pills a day. Grapefruit juice? That’s a natural warning system. The FDA? They’re bought off. St. John’s Wort? It’s been banned in Europe for decades. Why? Because it’s too cheap and too real. Your doctor’s ‘evidence-based’ combo? Probably funded by a drug company with a yacht. I’ve been off all my meds for 3 years. I eat turmeric, garlic, and raw garlic. My BP is 105/68. They can’t scare me with their charts. The system is rigged.
Nishant Sonuley
January 18, 2026 AT 23:41Look, I get it. We all want to believe that if we just take enough pills, we’ll be fine. But here’s the uncomfortable truth: polypharmacy isn’t medicine-it’s triage. We’re not treating disease anymore, we’re managing the side effects of the side effects. I had an 82-year-old patient on 11 medications. She couldn’t walk without falling, had zero energy, and was on three blood pressure drugs that canceled each other out. We cut it to four. She started gardening again. Sometimes, the most powerful drug is the one you stop taking. And yes, I know that sounds radical. But radical is what happens when you stop listening to the noise and start listening to the patient.
Emma #########
January 20, 2026 AT 07:30I just did my brown bag review last week. Turned out I was taking two different magnesium supplements I didn’t even know about. One was from my ‘heart health’ gummy pack. My doctor was shocked. I felt like an idiot… but also relieved. Thanks for reminding me to be honest-even about the ‘tiny’ stuff.
kenneth pillet
January 20, 2026 AT 19:29NSAIDs are the silent killer. I took ibuprofen for a headache last month and ended up with a GI bleed. No warning. No symptoms until I passed out. Don’t be like me. Tylenol is your friend. Unless you’re a drinker. Then… maybe don’t.
Jodi Harding
January 21, 2026 AT 15:58They call it ‘polypharmacy’ like it’s a clinical term. It’s just medical hoarding. We’re treating symptoms like they’re separate problems instead of one broken system. You don’t need ten pills. You need a life that doesn’t require them.
Zoe Brooks
January 21, 2026 AT 18:55My grandma used to say ‘if it’s not on your list, it’s not real.’ So now I keep a sticky note on my fridge with every pill I take. I even write down the ‘vitamins.’ My pharmacist laughs but she says it’s saved her from two bad interactions. Small habits, big saves 💪
Kristin Dailey
January 23, 2026 AT 01:54Stop taking supplements. America’s obsessed with ‘natural’ nonsense. If your doctor prescribed it, take it. If not, don’t. Grapefruit? Don’t. Alcohol? Don’t. Simple. No conspiracy. No herbal nonsense. Just science.