Every year, millions of people take generic drugs because they’re affordable, effective, and widely available. But what if the pill in your bottle isn’t what it claims to be? Fake generic drugs aren’t just a distant problem-they’re hiding in plain sight, slipping into supply chains across the world. And they’re getting smarter.
How fake drugs are made
Counterfeit generic drugs don’t come from labs with white coats and safety goggles. They’re made in hidden factories, often in countries with weak oversight. Places like parts of Southeast Asia, Eastern Europe, and even some regions in Africa have become hotspots for this illegal trade. These operations don’t need advanced tech-just access to cheap printing equipment, chemical suppliers, and a basic understanding of what real pills look like. The goal? Pure profit. A single blister pack of a popular generic blood pressure medication might cost $0.10 to produce. On the market, it sells for $5 or more. That’s a 5,000% markup. And since generics make up over 80% of all prescriptions filled in the U.S. and similar numbers globally, they’re the perfect target. The fake pills look real. Really real. Packaging is copied down to the font size, color shade, and even the way the foil seals. Some counterfeiters use the same batch numbers. Others replicate QR codes that scan to fake verification sites. In 2023, Europol seized counterfeit cancer drugs with holograms so accurate, even trained pharmacists struggled to tell them apart without lab tests. The ingredients? That’s where it gets dangerous. Instead of the real active ingredient, you might get chalk, sugar, or worse-chemicals that look similar but do nothing, or worse, cause harm. In 2008, contaminated heparin from China led to 149 deaths in the U.S. because it was laced with a toxic industrial compound. That wasn’t a random mistake. It was deliberate substitution.How fake drugs get into the real supply chain
You’d think pharmacies and hospitals are safe. But the supply chain is long, complex, and full of gaps. One major route is parallel importation. A drug approved in one country might be cheaper than in another. Some distributors buy it legally abroad, then resell it in markets where it’s not officially authorized. No one checks if the product has been stored properly, or if it’s even real. It just gets mixed in with legitimate stock. Then there’s the grey market. This is where unauthorized distributors-sometimes even former employees of legitimate suppliers-mix fake drugs into shipments. They don’t replace the whole batch. Just a few bottles here and there. Hard to spot. Hard to trace. The biggest loophole? Online pharmacies. The National Association of Boards of Pharmacy found in 2022 that 95% of online pharmacies selling prescription drugs operate illegally. You don’t need a prescription. You don’t get a receipt with a serial number. You get a box with pills that look right but might contain nothing but starch. Even legitimate distributors can be tricked. In 2018, a recall of certain blood pressure medications revealed that carcinogenic impurities had entered the supply chain through raw material suppliers in India and China. The problem wasn’t counterfeiting-it was poor quality control. But the same weak links that allow contamination also allow fakes to slip through.Why generics are the main target
Generic drugs are cheaper because they don’t require new clinical trials. Manufacturers just need to prove their version is “bioequivalent” to the brand-name drug. That means the active ingredient must be the same, in the same amount, and absorbed the same way. But here’s the catch: the rules don’t always get enforced. In countries with weak regulatory systems, manufacturers can cut corners. They might use cheaper fillers. They might skip stability tests. Or they might just skip the active ingredient entirely. The global generic drug market hit $438.7 billion in 2022. That’s a huge target. Counterfeiters don’t go after rare specialty drugs-they go for the big sellers: antibiotics, heart meds, diabetes pills, and antimalarials. These are taken daily, by millions. Even a small percentage of fakes means massive profits. The World Health Organization estimates that in some low-income countries, up to 30% of medicines are fake. In Africa, that number is even higher-42% of all substandard or falsified medicines globally come from there. That’s not just a health risk. It’s a public health crisis.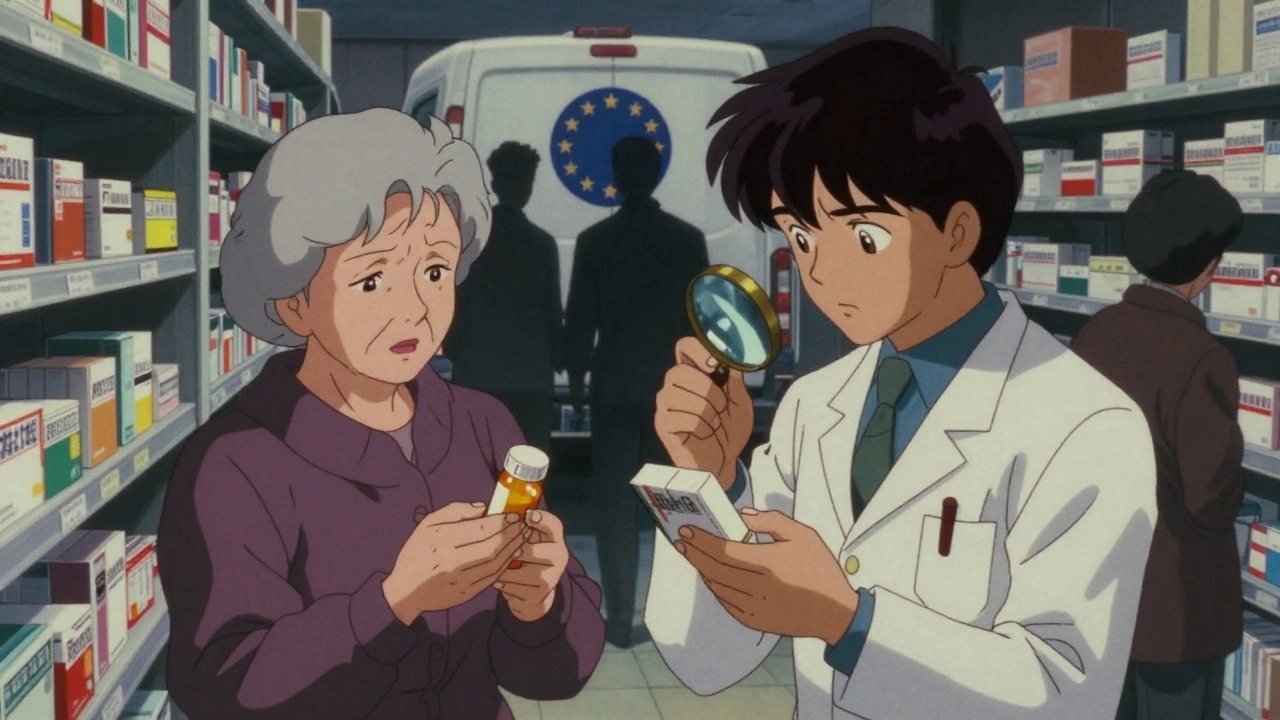
What’s being done-and what’s not
Some countries are fighting back. The U.S. passed the Drug Supply Chain Security Act in 2013, requiring full traceability of every package by 2023. That means every bottle, every box, every pallet has a unique serial number. If something looks off, you can trace it back. The European Union’s Falsified Medicines Directive, rolled out in 2019, requires tamper-proof packaging and a digital verification system. Since then, counterfeit penetration in Europe has dropped by an estimated 18%. But globally? Only 22 of 194 WHO member states have fully operational track-and-trace systems. Most low-income countries can’t afford the technology. A single security tag on a pill bottle costs 2 to 5 cents. Sounds small. But when you’re producing millions of pills a month, that adds up fast. Some companies are using invisible markers-DNA tags, chemical tracers, even micro-printed patterns only visible under UV light. Pfizer’s anti-counterfeiting program has stopped over 302 million fake doses since 2004. But these tools aren’t mandatory. And they’re not used everywhere. Meanwhile, counterfeiters are adapting. AI now helps them design packaging that passes visual inspections. One Europol operation in early 2023 uncovered cancer drugs with AI-generated holograms that fooled even automated scanning systems.How to spot a fake (and what to do)
You can’t always tell a fake by sight. But you can look for red flags:- Changes in color, shape, or size compared to your usual prescription
- Unfamiliar branding or misspelled words on the label
- Packaging that feels flimsy or looks off under a phone flashlight
- Online pharmacies that don’t require a prescription or don’t list a physical address
- Pills that taste strange or don’t dissolve the way they used to

What you can do to stay safe
Buy from licensed pharmacies only. If you’re buying online, use sites verified by the National Association of Boards of Pharmacy (NABP) or your country’s equivalent. Look for the VIPPS seal in the U.S., or the EU’s common logo for legal online pharmacies. Never buy from social media ads, pop-up websites, or vendors offering “discounted” brand-name drugs. If it sounds too good to be true, it is. Keep your prescription records. If your pill looks different, compare it to your last bottle. Note the imprint code, color, shape. Report anything unusual to your doctor or local health authority. And if you’re traveling abroad, avoid buying medication locally unless it’s from a reputable hospital or pharmacy. Many countries don’t have the same standards as the U.S., Canada, or the EU.The bigger picture
Fake drugs aren’t just about fraud. They’re about survival. A counterfeit antibiotic might not kill you right away-but it can let an infection grow stronger, leading to drug-resistant superbugs. A fake malaria drug might cause a child to die because the treatment didn’t work. A fake heart pill might trigger a stroke because the dose was wrong. This isn’t a problem that will fix itself. It needs global cooperation, better laws, more funding for regulators, and public awareness. Right now, we’re playing catch-up. The criminals are using AI. We’re still using flashlights and magnifying glasses. The good news? We know how to stop it. We have the tools: serialization, digital verification, forensic testing, international sharing of data. What we lack is the will to make them universal. Until every country enforces the same standards, until every pill can be traced from factory to patient, the risk won’t go away. And as long as people are desperate for cheap medicine, counterfeiters will keep finding ways in.Frequently Asked Questions
How common are fake generic drugs?
In high-income countries, fake drugs make up about 1% of the market. But in low- and middle-income countries, that number can jump to 30% or higher. Africa alone accounts for 42% of all substandard and falsified medicines worldwide. The World Health Organization estimates that over 1 million deaths each year are linked to fake or poor-quality medicines.
Can I tell if a pill is fake just by looking at it?
Sometimes-but not always. Many counterfeit pills are nearly identical to the real thing. Packaging, color, size, and even imprint codes can be copied perfectly. The only sure way to know is through lab testing. But you can spot warning signs: misspelled names, unusual texture, odd taste, or packaging that feels cheap. If something looks off, don’t take it.
Are online pharmacies safe?
Most aren’t. The National Association of Boards of Pharmacy found that 95% of online pharmacies operating without a license sell counterfeit or unsafe drugs. Only use websites that are verified by official bodies like NABP’s VIPPS program or your country’s pharmacy regulator. If a site doesn’t require a prescription or doesn’t list a physical address, avoid it.
What should I do if I think I have a fake drug?
Stop taking it immediately. Bring the medication to your pharmacist or doctor. They can report it to health authorities. Don’t throw it away-keep the packaging and pills as evidence. In many countries, you can also report suspected counterfeits directly to your national drug regulatory agency.
Why are generic drugs targeted more than brand-name drugs?
Because they’re everywhere. Generics make up over 80% of prescriptions in most countries. They’re cheaper, so more people buy them-and counterfeiters know that. Plus, since generics don’t have the same brand recognition as name-brand drugs, it’s easier to pass off fakes as the real thing. The profit margin is huge, and the risk of getting caught is low.
Is there a global system to track fake drugs?
Not yet. Some countries, like the U.S. and those in the EU, have strong track-and-trace systems. But globally, only 22 out of 194 WHO member states have fully operational systems. Without universal standards, counterfeiters exploit gaps between countries. Efforts are underway to create a global network, but progress is slow due to cost and political barriers.


Lara Tobin
December 13, 2025 AT 09:41I just got my blood pressure meds last week, and the pills looked a little different... I didn't think much of it until I read this. 😔 I'm so glad I didn't take them yet. Going to my pharmacist tomorrow. Thanks for the heads-up.
Jamie Clark
December 13, 2025 AT 18:52It's not about counterfeit pills-it's about the entire capitalist framework that turns life-saving medicine into a commodity. We've outsourced ethics to profit margins. The real crime isn't the fake drugs-it's the system that lets them exist in the first place.
Keasha Trawick
December 15, 2025 AT 02:56Okay, so imagine this: AI-generated holograms on cancer meds. 🤯 We're not just fighting snake oil anymore-we're fighting *algorithmic deception*. These aren't guys in basements with glue guns anymore. They're using GANs to clone packaging. The FDA's still using magnifying glasses while the bad guys are running neural nets. We're in a pharmacological Cold War, and we're losing.
Webster Bull
December 16, 2025 AT 16:53Don't panic. But DO act. Check your scripts. Know your pills. Use NABP sites. Your life’s worth more than a $5 shortcut. 💪 You got this.
Donna Hammond
December 17, 2025 AT 22:37There's a critical gap between regulatory policy and implementation. The DSCSA and FMD are excellent frameworks, but without mandatory global adoption and funding for low-income nations, they're just digital paperweights. We need WHO-led international enforcement units with forensic capabilities-not just guidelines. This isn't a national issue; it's a planetary health emergency.
Richard Ayres
December 19, 2025 AT 01:04It's sobering to consider how much we take for granted-pills we swallow without question, trusting systems we never see. Perhaps the real question isn't how fakes enter the supply chain, but why we've allowed our trust in medicine to become so passive. Awareness is the first step, but responsibility must follow.
Sheldon Bird
December 19, 2025 AT 18:58Hey, I know this sounds corny, but you’re not alone. If you're worried about your meds, talk to your pharmacist-they’re the real heroes here. 🙌 And hey, if you see something weird? Report it. You're not being paranoid-you're being smart.
Karen Mccullouch
December 21, 2025 AT 01:30Of course this is happening. China and India are running medicine factories like they're printing Monopoly money. And we just sit here with our Starbucks and our 'buy from verified sites' memes. Wake up, America. This is war. And we're losing. 🇺🇸💣
Ronan Lansbury
December 22, 2025 AT 20:42Let’s be honest: this is all a psyop. The FDA, WHO, and Big Pharma are *using* counterfeit drugs to justify increased surveillance and control over the population. The 'AI-generated holograms' are a distraction. Real medicine is already being replaced by nanotech implants. This article? Just a Trojan horse to normalize biometric tracking. You think you're safe? You're already tagged.
Himmat Singh
December 23, 2025 AT 04:14It is an incontrovertible fact that the proliferation of substandard pharmaceuticals is a direct consequence of the deregulatory ethos that has permeated global trade policy since the 1990s. The commodification of essential medicines has resulted in a structural erosion of quality assurance mechanisms, thereby rendering the pharmaceutical supply chain vulnerable to systemic exploitation. The solution lies not in consumer vigilance, but in the reestablishment of sovereign pharmaceutical sovereignty.
kevin moranga
December 23, 2025 AT 07:30Man, I never thought about this until my grandma got sick last year. She was taking her diabetes meds from some 'discount pharmacy' online-said it saved her $100 a month. Turned out the pills were just sugar with a little dye. She ended up in the ER. We switched to CVS, got the real stuff, and she’s doing way better now. I’m telling everyone I know: don’t risk it. Your grandma’s life? Worth every penny. And if you’re buying online? Make sure it’s got that VIPPS seal. No excuses. Seriously. 🙏
Alvin Montanez
December 23, 2025 AT 17:42People think they're saving money by buying from sketchy online pharmacies? That’s not saving-it’s suicide with a discount coupon. You’re not being frugal, you’re being reckless. And now you want to blame the system? No. You chose the cheap pill. You chose to ignore the warnings. You chose to believe a website that says 'Buy 1000 pills for $20.' And now you’re surprised when your body starts shutting down? Wake up. This isn't a conspiracy. This is consequence. You don't get to play Russian roulette and then cry when the bullet fires. Your laziness is killing people. And you're the reason this problem keeps getting worse.