Most people think taking two stomach meds together means better relief. But when it comes to H2 blockers and PPIs, combining them often does more harm than good. These drugs are both designed to reduce stomach acid, but they work in completely different ways-and putting them together doesn’t give you double the benefit. Instead, it raises your risk of infections, kidney damage, and unnecessary side effects-all while costing the healthcare system billions.
How H2 Blockers and PPIs Actually Work
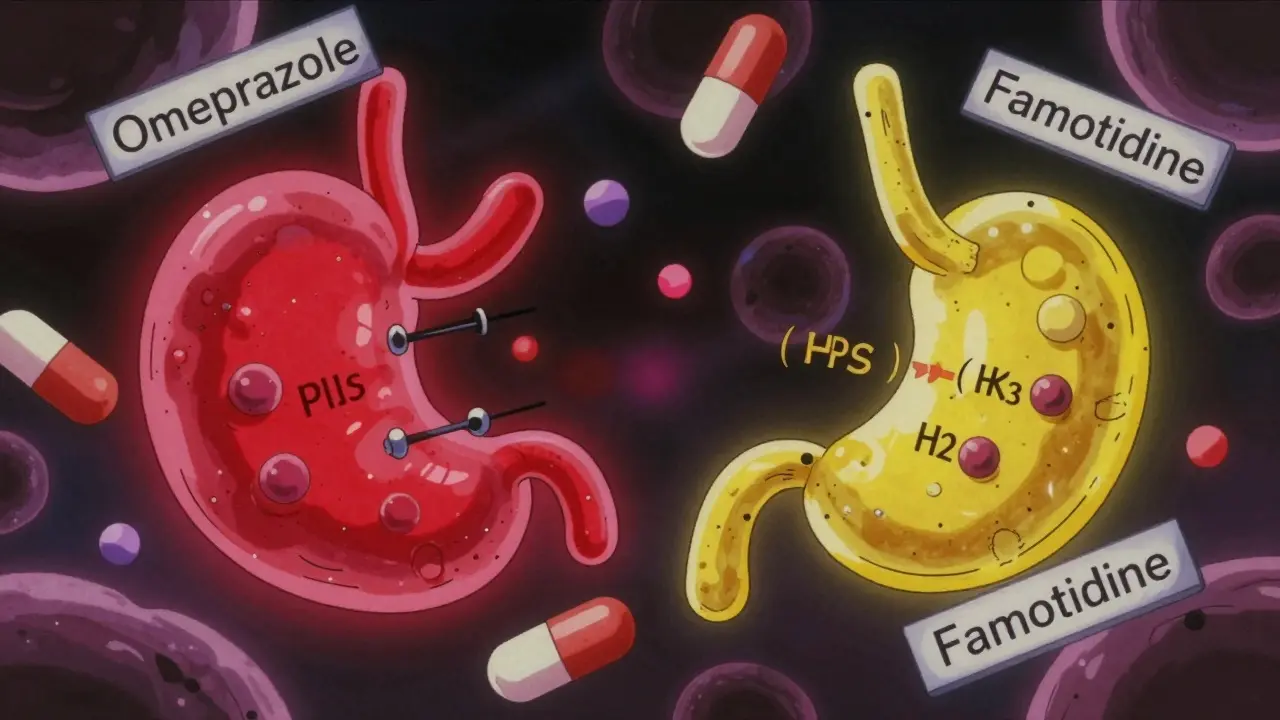
H2 blockers like famotidine (Pepcid) and cimetidine (Tagamet) block histamine from signaling your stomach to make acid. They kick in fast-within an hour-and cut acid production by about half. But their effect fades after 6 to 12 hours. That’s why people used to take them at bedtime to prevent nighttime heartburn.
PPIs like omeprazole (Prilosec) and esomeprazole (Nexium) go further. They shut down the actual acid-producing pumps in your stomach cells. This isn’t a quick fix-it takes 2 to 5 days to reach full power. But once it does, it suppresses acid by 90% or more, all day long. That’s why PPIs became the go-to for chronic GERD, ulcers, and acid reflux.
At first glance, combining them seems logical: hit acid from two angles. But here’s the problem-PPIs suppress acid so thoroughly that there’s almost no histamine left to stimulate the stomach. That means H2 blockers lose their target. A 2022 study in the Journal of Clinical Gastroenterology found that adding ranitidine to omeprazole only lowered nighttime acid by 5%. Not enough to matter. And that’s the pattern across nearly every trial.
Why Doctors Still Prescribe Both (And Why They Shouldn’t)
Despite the evidence, about 15-20% of hospitalized patients still get both drugs at the same time. Why? Tradition. Habit. Fear. Some doctors think if one drug helps, two must help more. Others prescribe them together out of caution-especially in ICU patients where stress ulcers are a concern.
But the data says otherwise. A landmark 2014 study in JAMA Internal Medicine tracked nearly 80,000 ICU patients. Those on PPIs had a 30% higher risk of pneumonia and a 32% higher risk of Clostridium difficile infection than those on H2 blockers alone. Even more surprising: PPI users had a 22% higher risk of gastrointestinal bleeding. That’s the opposite of what you’d expect if acid suppression was protective.
The American College of Gastroenterology updated its guidelines in 2022 to say this clearly: “Long-term combination therapy with H2RAs and PPIs does not offer additional benefit for the management of GERD.” That’s not a suggestion. It’s a fact backed by 12 clinical trials and over 2,800 patients.
The Hidden Dangers of Long-Term Use
PPIs are safe for short-term use. But when taken for months or years, they start to cause real problems.
- Kidney damage: A 2021 study of 3,600 people with chronic kidney disease found PPI users were 28% more likely to progress to end-stage kidney disease than those on H2 blockers.
- Vitamin and mineral loss: PPIs interfere with absorption of magnesium, calcium, and vitamin B12. Low magnesium can cause muscle cramps, irregular heartbeat, and seizures. Low B12 leads to nerve damage and anemia.
- Bone fractures: The FDA warned in 2014 that long-term, high-dose PPI use increases fracture risk-especially in older adults.
- Rebound acid: After stopping PPIs, many people experience worse heartburn than before. This isn’t “addiction”-it’s your stomach overcompensating after being shut down for too long.
On Drugs.com, 68% of users report side effects from PPIs. Headaches, diarrhea, bloating, fatigue-these aren’t rare. They’re common. And when you add an H2 blocker on top, you’re not fixing the problem. You’re adding another layer of drugs with their own risks.
When Is Combining Them Actually Okay?
There’s one scenario where adding an H2 blocker to a PPI might make sense-and it’s rare.
If you’re on a twice-daily PPI and still have nighttime heartburn, your doctor might suspect “nocturnal acid breakthrough.” That’s when your stomach acid rises above safe levels between midnight and 6 a.m., even while on PPIs. The only way to confirm this is with a 24-hour pH monitoring test.
If the test shows your stomach pH drops below 4 for more than 60 minutes overnight, then adding an H2 blocker at bedtime for a few weeks might help. But here’s the catch: you must retest after 4 to 8 weeks. If symptoms don’t improve, the H2 blocker gets stopped. No exceptions.
The Department of Veterans Affairs recommends a “PPI time-out” every 90 days. Ask yourself: Do I still have symptoms? Can I lower my dose? Do I even need this anymore? Most people can stop PPIs safely with gradual tapering and lifestyle changes.
Drug Interactions You Can’t Ignore
Not all H2 blockers are the same. Cimetidine (Tagamet) is an old drug that blocks liver enzymes responsible for breaking down other medications. That means it can make PPIs, blood thinners, antidepressants, and even some antibiotics stick around in your body longer-raising the risk of overdose or side effects.
Famotidine (Pepcid) doesn’t do this. It’s safer. But even then, you’re still stacking two drugs that affect your stomach. The more meds you take, the more likely you are to experience something unexpected. And most patients don’t even know why they’re on both.
A 2022 survey by the American College of Gastroenterology found that 31% of patients on dual therapy couldn’t explain why they were taking both drugs. And 64% didn’t know the possible side effects. That’s not informed consent. That’s prescription inertia.
What You Should Do Instead
If you’re on a PPI and thinking about adding an H2 blocker, pause. Ask these questions:
- Am I on this medication because I have a confirmed diagnosis, or just because I felt better once?
- Have I tried lifestyle changes-eating smaller meals, avoiding late-night snacks, losing weight, cutting caffeine and alcohol?
- Has my doctor confirmed I have true GERD, or am I just self-diagnosing heartburn?
- How long have I been on this drug? Is it still necessary?
For most people, the answer is simple: stop the PPI, or at least lower the dose. Use an H2 blocker only if you need short-term relief. Try antacids like Tums or Maalox for quick fixes. Elevate your head while sleeping. Avoid trigger foods. These non-drug approaches work better than stacking medications.
And if your doctor insists on combining them, ask for the evidence. Show them the 2022 ACG guidelines. Ask if they’ve reviewed your 24-hour pH test results. If they can’t answer, it’s time to get a second opinion.
The Bigger Picture: Overprescribing Is Costing Us Billions
The U.S. spends $12.3 billion a year on acid-suppressing drugs. PPIs make up 78% of those prescriptions. But research shows that up to 70% of PPI prescriptions are unnecessary. Add H2 blockers to the mix, and you’re looking at $1.5 billion wasted annually on drugs that don’t work-and may harm you.
Medicare is catching on. Starting in 2024, hospitals that prescribe inappropriate dual acid suppression to more than 15% of their patients could lose reimbursement. That’s not a penalty. It’s a wake-up call.
And it’s not just about money. It’s about your health. Every extra pill you take adds risk. Every unnecessary drug weakens your body’s natural balance. You don’t need two acid blockers to feel better. You need the right one-and only if you truly need it.
Can I take famotidine and omeprazole together?
You can, but you shouldn’t unless you have confirmed nocturnal acid breakthrough despite twice-daily PPI therapy. Even then, it should be temporary-no longer than 4 to 8 weeks-and only after a 24-hour pH test confirms the issue. For most people, this combination adds no benefit and increases risk.
Are H2 blockers safer than PPIs?
For long-term use, yes. H2 blockers like famotidine have fewer serious side effects than PPIs. They don’t increase the risk of kidney disease, bone fractures, or C. diff infections nearly as much. They’re also less likely to interfere with nutrient absorption. If you need ongoing acid control, an H2 blocker is often the safer choice.
Why do doctors keep prescribing both drugs together?
Many doctors prescribe both out of habit, fear of missing something, or because they were taught to do so years ago. There’s also pressure to “do something” for patients with persistent symptoms. But guidelines have changed. The American College of Gastroenterology and the American Gastroenterological Association both recommend against routine combination therapy. It’s outdated practice.
What are the signs I’m taking too many acid-reducing drugs?
Watch for frequent headaches, diarrhea, muscle cramps, fatigue, tingling in your hands or feet, or unexplained bone pain. These can signal low magnesium, B12 deficiency, or early kidney issues. If you’ve been on PPIs for more than 3 months without a clear diagnosis, it’s time to talk to your doctor about tapering off.
Can I stop PPIs cold turkey?
No. Stopping suddenly can cause rebound acid hypersecretion, making heartburn worse than before. Instead, work with your doctor to gradually reduce the dose over 2-4 weeks. Switch to an H2 blocker or antacid as needed during the taper. Lifestyle changes-like eating earlier and avoiding triggers-help reduce withdrawal symptoms.

Emma Hooper
December 31, 2025 AT 16:50Y’all are still taking two acid pills like it’s a smoothie shot? 😅 I was on PPIs for 3 years thinking I needed them-turns out I just needed to stop eating pizza at midnight and sleep on a wedge pillow. My stomach thanked me. No drugs. No drama. Just… less fire.
Harriet Hollingsworth
January 1, 2026 AT 00:25This is why people are dying from lazy medicine. Doctors don’t care. They just prescribe. You think your body needs this? No. It needs rest. It needs discipline. It needs you to stop treating your stomach like a broken faucet you can just turn off with chemicals.
Chandreson Chandreas
January 3, 2026 AT 00:12Life’s funny, right? We’ve got labs that can sequence DNA but still can’t teach doctors to stop stacking meds like Legos. 🤷♂️ Sometimes the body just needs space to heal-not more chemicals. I stopped my PPIs last year. No rebound. Just peace. And better sleep. 🌙
Branden Temew
January 3, 2026 AT 15:01Oh wow, so the medical industrial complex isn’t just selling cancer drugs and antidepressants-now they’re selling *two* acid blockers for the price of one? Groundbreaking. Next up: combining Tylenol and ibuprofen because ‘two is better than one.’ 🙃
Hanna Spittel
January 5, 2026 AT 13:52Big Pharma paid the doctors. They know. They’re all in on it. PPIs = profit. H2 blockers = cheaper. But they don’t want you to know you can just eat less sugar and sleep upright. They want you addicted. 🕵️♀️💊
anggit marga
January 6, 2026 AT 00:33Who even are these American doctors anyway? In India we don’t mix these pills unless we have to. You think your stomach is so weak? Try eating street food for a week then come back with your fancy PPIs
Joy Nickles
January 7, 2026 AT 00:54OMG I’ve been on both for 2 years and I just realized… I have NO IDEA why. I think my doctor said ‘it’s better for the night’?? But I don’t even have night symptoms anymore. I’m terrified to stop. What if I die?? 😭
Martin Viau
January 8, 2026 AT 13:49Per the 2022 ACG guidelines, the concomitant use of H2RAs and PPIs lacks pharmacodynamic synergy in the majority of GERD cohorts, and confers a statistically significant elevation in C. diff and CKD risk profiles. The cost-benefit ratio is untenable in primary care settings without pH-metry confirmation. Also, famotidine’s CYP3A4 profile is negligible, unlike cimetidine-which is basically a drug interaction grenade.
Marilyn Ferrera
January 9, 2026 AT 07:43If you’ve been on PPIs longer than 3 months without a diagnosis, it’s time to taper. Not quit. Taper. And yes, you can do it. Start with H2 blockers, then antacids as needed. Eat early. Sleep elevated. You’ve got this.
Deepika D
January 11, 2026 AT 07:05Hey, I was just like you-on PPIs for years, felt like I couldn’t live without them. Then I started walking after dinner, stopped drinking soda, and ate my last meal at 6 p.m. No magic. Just habits. I’m off the meds now, and my digestion feels like it’s finally breathing again. You don’t need a pill to feel okay. You just need a little patience and a lot of self-kindness. 🌱💛
Bennett Ryynanen
January 12, 2026 AT 19:12My dad was on both for 5 years. Got kidney damage. Then they told him ‘oh, just stop the PPI.’ But he was terrified. I had to sit with him for 3 weeks while he tapered. Now he eats curry without fear. And he’s alive. That’s the win.
Darren Pearson
January 13, 2026 AT 10:42It is an unfortunate epistemological failure of contemporary gastroenterological practice that clinicians continue to conflate pharmacological potency with therapeutic efficacy. The notion that additive acid suppression yields additive clinical benefit is a fallacy rooted in reductionist thinking and is empirically untenable in light of contemporary meta-analyses.
Stewart Smith
January 13, 2026 AT 22:49So… you’re telling me the thing I’ve been paying $200/month for since 2020… doesn’t actually do anything? And I’ve been feeling tired because my body’s trying to absorb vitamins through acid-blocked walls? 😅 Well. Guess I’m calling my doctor tomorrow. Thanks for the nudge.
Aaron Bales
January 15, 2026 AT 17:00Just stopped my PPI last month. Tapered with famotidine. No rebound. No panic. Just… normal digestion. And I haven’t had heartburn since I stopped eating nachos before bed. Sometimes the solution isn’t more drugs. It’s less junk.