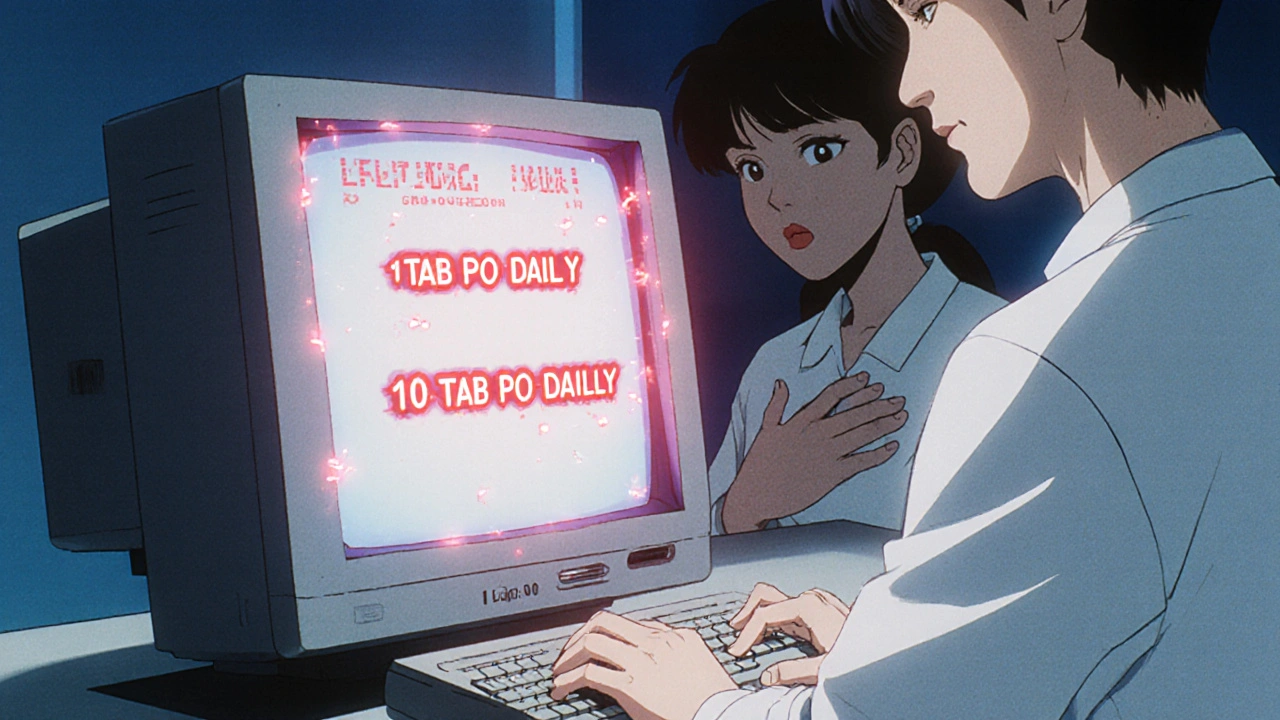
Electronic prescribing was supposed to fix medication errors. No more scribbled handwriting, no more misread abbreviations. But here’s the problem: transcription errors haven’t disappeared-they’ve just changed shape. Instead of a doctor’s messy script, you now get a digital prescription that gets scrambled between systems. A patient gets told to take one tablet daily. The system sends it as '1 TAB PO DAILY'. The pharmacy’s software misreads it as '10 TAB PO DAILY'. That’s not a typo. That’s a dangerous glitch. And it’s happening more often than you think.
Why E-Prescribing Created New Mistakes
When e-prescribing took off in the U.S. after 2009, it cut overall prescribing errors by up to 99% in some studies. That’s huge. But the remaining errors? A shocking 37-41.5% of them are now transcription errors. That’s when data moves from one digital system to another-and gets corrupted along the way. It’s not the doctor’s fault. It’s not the pharmacist’s fault. It’s the systems talking past each other. Think of it like texting someone in another country. You say ‘I’ll be there at 5.’ They get ‘I’ll be there at 50.’ Why? Because your phone uses a different format than theirs. That’s exactly what’s happening between Epic, Cerner, QS/1, and Pioneer pharmacy systems. One system sends ‘take 1 tablet by mouth daily.’ Another reads it as ‘1 TAB PO DAILY’ and auto-converts it wrong. The result? A patient gets ten times the dose they were supposed to.The Biggest Culprits Behind Transcription Errors
Not all e-prescribing systems are built the same. There are two main types: integrated and standalone. Integrated systems like Epic or Cerner connect directly to the hospital’s electronic health record. Standalone systems like DrFirst Rcopia work on their own. Here’s the twist: standalone systems actually have fewer transcription errors-42% fewer, according to a 2019 KLAS report. Why? Because they don’t try to force data through a messy EHR. They keep things simple. But integrated systems dominate the market. They hold 68% of hospital share. And here’s the catch: they only reduce transcription errors by 55% more than standalone ones if they’re fully connected to the pharmacy. Most aren’t. That means pharmacists still manually retype prescriptions. And humans make mistakes. A 2022 Surescripts report found that 41% of pharmacists spend 15-30 minutes a day fixing e-prescription errors. That’s half an hour per day, per pharmacist, just untangling digital messes. The worst offenders? Poorly formatted instructions. A study from a Reddit pharmacy forum showed that 27% of prescriptions from Epic systems arrive with sigs that don’t match the pharmacy’s system. 'Take one tablet daily' becomes '1 TAB PO DAILY'-and the system interprets 'TAB' as '10 tablets.' That’s not a stretch. It’s a known bug.How to Fix It: Six Proven Strategies
The Agency for Healthcare Research and Quality (AHRQ) laid out six evidence-backed fixes. These aren’t theoretical. They’ve been tested in clinics and pharmacies across the U.S.- Standardize the sig format-Use plain language like 'take one tablet by mouth once a day.' No abbreviations. No codes. Systems that use structured sigs cut transcription errors by 41%.
- Use CancelRx-This protocol lets doctors electronically cancel old prescriptions. Without it, patients get two prescriptions for the same drug-one old, one new. Pharmacists have to guess which one to fill. CancelRx cuts those errors by 63%.
- Build a single shared medication list-When a patient’s entire drug history is visible to both doctor and pharmacist, refills get automated correctly. One practice using Epic and CVS saw 100% fewer refill errors.
- Add medication indications-Instead of just writing 'metformin,' write 'for type 2 diabetes.' This stops doctors from accidentally prescribing the wrong dose. One study showed it eliminated 79% of indication-drug mismatches.
- Connect pharmacy and prescriber systems directly-Use HL7 FHIR Release 4.0.1, the latest interoperability standard. It cuts manual re-entry by 92%. If your system can’t do this, it’s outdated.
- Redesign how prescriptions are modified-If a doctor needs to change a prescription after it’s sent, the system should alert the pharmacy automatically. Right now, many systems don’t. That’s why pharmacists get conflicting orders. Fixing this cuts confusion errors by 67%.
What Systems Should You Use?
Not all e-prescribing platforms are created equal. If you’re a small practice with fewer than 10 providers, standalone systems like DrFirst Rcopia might be your best bet. They’re simpler, cheaper, and have fewer integration headaches. If you’re part of a hospital or large group, go for an ONC-certified integrated system like Epic or Cerner. But only if it’s fully connected to your pharmacy’s system. Check if your pharmacy uses QS/1, Pioneer, or another major system-and confirm the two can talk to each other using the NCPDP SCRIPT Standard Version 201900. Don’t fall for the myth that ‘more features = better.’ A system that shows 17 alerts for every prescription? That’s alert fatigue. Providers start ignoring them. Dr. Joan Ash from Oregon Health & Science University found that 34% of transcription errors happen because doctors just click past warnings. Less is more.Real-World Impact: Numbers That Matter
The numbers don’t lie. Here’s what happens when you fix these problems:- Practices using full interoperability saw a 67% drop in transcription-related medication errors (AHRQ, 2020).
- When medication indications were added, dosing errors like weekly vs. daily methotrexate dropped by 78% (Dr. David Bates, Harvard).
- Pharmacies using the Surescripts Pharmacy Health Information Exchange cut transcription errors by 88% in pilot sites.
- Patients on systems with shared medication lists had 52% fewer reconciliation errors.
What’s Changing in 2025?
The game is shifting fast. The ONC’s 2023 Interoperability Roadmap demands all e-prescribing systems use API-based connections by 2025. That means no more manual re-entry. If your system isn’t ready, you’ll be non-compliant. The DEA’s 2021 rule requiring electronic transmission of controlled substances (EPCS) already cut transcription errors for Schedule II drugs by 57%. Now, the focus is on FHIR-the new language all systems must speak. HL7 International’s Da Vinci Project showed 98% error reduction in 2023 pilots using FHIR. Even AI is stepping in. Epic’s DoseMeRx, in pilot phase since 2023, uses machine learning to flag incorrect dosing before it’s sent. Early results? A 65% drop in errors. It’s not science fiction. It’s here.What You Can Do Today
You don’t need to wait for a system upgrade. Here’s what you can do right now:- Ask your EHR vendor: ‘Are we using FHIR and NCPDP SCRIPT 201900?’ If they don’t know, they’re not ready.
- Require all prescriptions to use plain-language sigs. No 'QD,' 'BID,' or 'TAB.' Just 'once a day,' 'twice a day.'
- Turn on CancelRx in your system. Make sure every cancellation is sent electronically.
- Ask your pharmacy: ‘Do you get our prescriptions without manual correction?’ If they say yes, ask for proof.
- Train your staff. Providers need 4.7 hours of training. Pharmacists need 3.2. Don’t skip it.
Final Thought: It’s Not About Technology-It’s About Trust
E-prescribing isn’t broken. It’s just poorly connected. The technology works. The standards exist. The fixes are proven. What’s missing is the will to implement them fully. When a patient gets the wrong dose because two systems couldn’t agree on what 'TAB' means, that’s not a technical issue. That’s a failure of care. We can fix it. But only if we stop treating e-prescribing as a checkbox and start treating it as a lifeline.What are transcription errors in e-prescribing?
Transcription errors in e-prescribing happen when prescription data gets corrupted during digital transfer between systems-like from a doctor’s EHR to a pharmacy’s software. These aren’t handwriting mistakes. They’re format mismatches, like 'take one tablet daily' turning into '1 TAB PO DAILY' and being misread as '10 tablets.' These errors cause incorrect dosing, missed refills, and dangerous drug interactions.
Why do e-prescribing systems still have errors if they’re digital?
Because different systems don’t speak the same language. Epic, Cerner, QS/1, and other platforms use different formats for instructions, drug codes, and dosing. Even if a prescription is sent electronically, if the receiving system can’t interpret the format correctly, it auto-converts it wrong. That’s why 41% of pharmacists spend 15-30 minutes a day fixing these errors.
What’s the difference between standalone and integrated e-prescribing systems?
Standalone systems like DrFirst Rcopia work independently and have fewer integration issues, leading to 42% fewer transcription errors. Integrated systems like Epic or Cerner connect to a hospital’s full electronic health record, offering more features but requiring perfect connectivity to the pharmacy. When fully connected, they reduce errors by 55% more than standalone systems-but only 32% of U.S. pharmacies have true interoperability.
How can pharmacies reduce transcription errors?
Pharmacists can reduce errors by insisting on standardized, plain-language sigs (no abbreviations), using systems that support CancelRx for electronic cancellations, and working with prescribers who use ONC-certified systems connected via FHIR and NCPDP SCRIPT 201900. Training staff to recognize common format mismatches and using shared medication lists also cuts errors significantly.
Is AI helping reduce e-prescribing errors?
Yes. AI tools like Epic’s DoseMeRx, currently in pilot, analyze prescriptions in real time and flag incorrect dosing or drug interactions before they’re sent. Early results show a 65% reduction in errors. These tools learn from past mistakes and are expected to become standard by 2026. But they only work if the underlying data is clean and standardized.
What’s the role of FHIR in fixing e-prescribing errors?
FHIR (Fast Healthcare Interoperability Resources) is the new global standard for exchanging health data. It replaces outdated formats with a common language that all systems can understand. HL7 International’s Da Vinci Project showed 98% error reduction in 2023 pilots using FHIR. The U.S. government requires all e-prescribing systems to use FHIR-based APIs by 2025. Until then, transcription errors will persist.

Margo Utomo
November 16, 2025 AT 17:35George Gaitara
November 18, 2025 AT 10:36Deepali Singh
November 18, 2025 AT 13:10Sylvia Clarke
November 19, 2025 AT 13:49Jennifer Howard
November 21, 2025 AT 09:38Abdul Mubeen
November 23, 2025 AT 06:06mike tallent
November 24, 2025 AT 23:12Joyce Genon
November 24, 2025 AT 23:33John Wayne
November 26, 2025 AT 18:26Julie Roe
November 28, 2025 AT 11:53jalyssa chea
November 29, 2025 AT 20:50Gary Lam
November 29, 2025 AT 23:01Peter Stephen .O
November 30, 2025 AT 23:24Andrew Cairney
December 1, 2025 AT 04:50Rob Goldstein
December 1, 2025 AT 17:44