Opioid Antiemetic Timing Calculator
Why Timing Matters
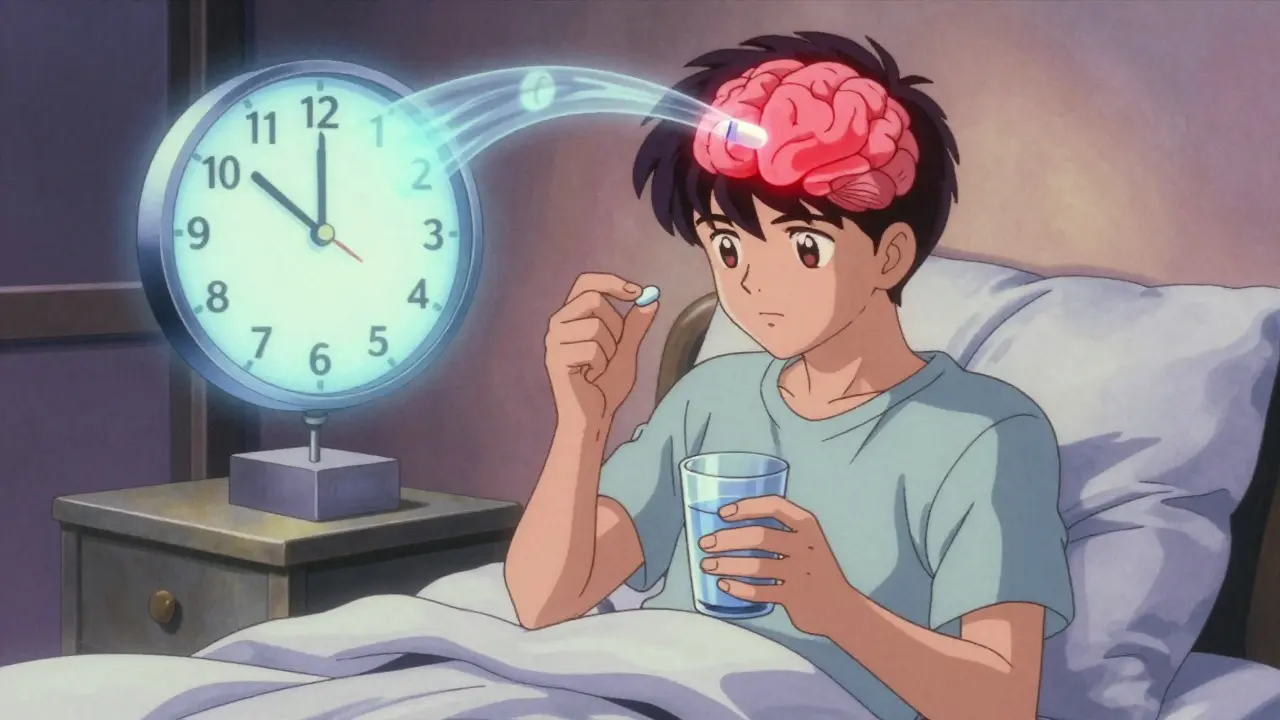
Opioids peak in your bloodstream 60-90 minutes after you swallow them. If you want to stop nausea before it starts, take your antiemetic 30-60 minutes before your opioid dose. This simple shift cuts nausea severity by up to 50% in clinical practice.
Pro Tip: Take your antiemetic 30-60 minutes before your opioid dose. For example: If you take morphine at 8 a.m., take prochlorperazine at 7:15 a.m. This isn't guesswork—it's pharmacology.
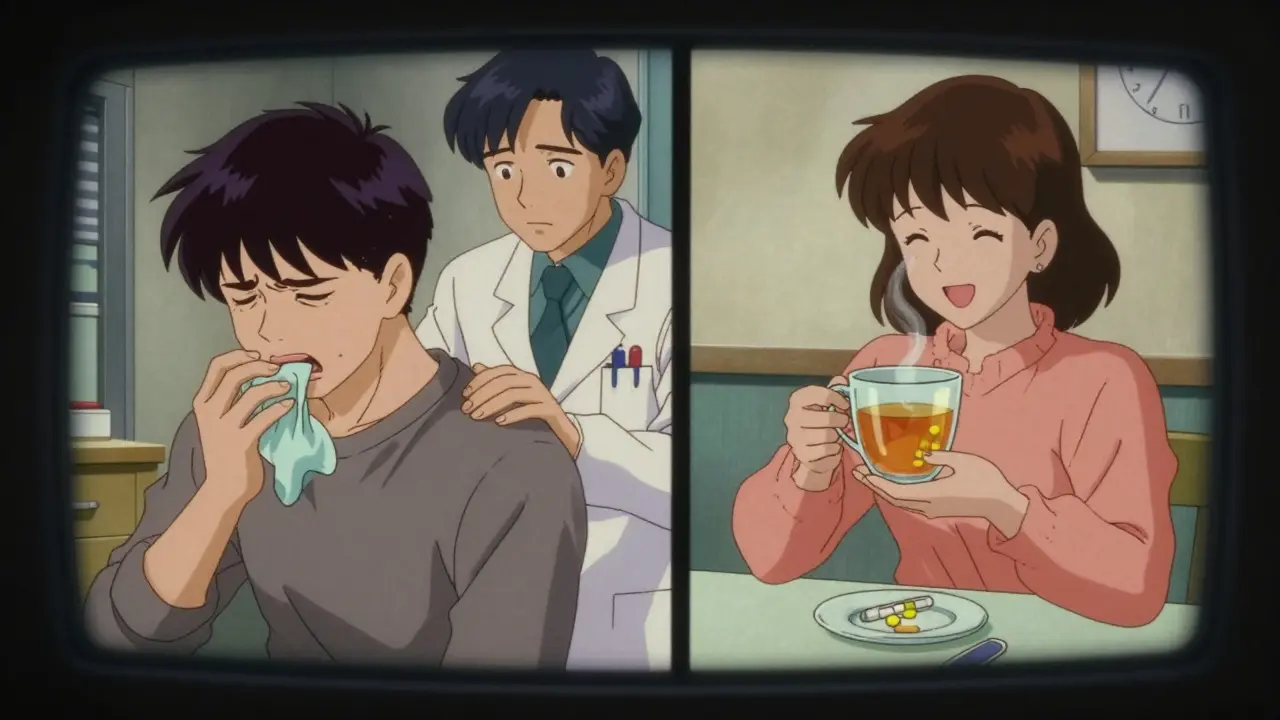
When you start taking opioids for pain, nausea isn’t just an inconvenience-it can make you quit the medication entirely. About 30-40% of people new to opioids experience nausea and vomiting, especially in the first few days. It’s not weakness or bad luck. It’s biology. Opioids bind to receptors in your brainstem, specifically the chemoreceptor trigger zone, and your body reacts like it’s been poisoned. The good news? This isn’t permanent. Most people build tolerance within 3 to 7 days. But until then, you need a plan.
Why Opioids Make You Nauseous (And Why It’s Not Just in Your Head)
Opioids don’t just block pain signals-they also activate areas in your brain that control vomiting. This is why nausea hits fast, often within hours of your first dose. It’s not about your stomach being upset. It’s your brain sending the wrong signal. Even if you haven’t eaten, even if you’re not sick, you still feel like you’re going to throw up. That’s opioid-induced nausea and vomiting (OINV), and it’s one of the most common reasons people stop taking opioids, even when they’re helping with their pain.
Studies show that 30-35% of cancer patients abandon opioid therapy because nausea becomes unmanageable. That’s not just a side effect-it’s a treatment failure. But here’s the thing: you don’t have to accept it. There are proven ways to fight it.
Which Antiemetics Actually Work?
Not all anti-nausea drugs are created equal when it comes to opioids. Some work well. Others barely help. Here’s what the evidence says:
- Haloperidol (0.5-2 mg daily): A dopamine blocker that targets the brain’s vomiting center. Cheap-under $0.05 per pill-and effective for 70-75% of people. But it can cause stiffness or tremors in older adults, especially over 65.
- Prochlorperazine (5-10 mg every 6-8 hours): A phenothiazine that’s often recommended as a first-line option. It’s gentler than haloperidol for many people and works well for both nausea and vomiting.
- Metoclopramide (5-10 mg every 6-8 hours): The only prokinetic drug available in the U.S. for this use. It speeds up your stomach emptying, which helps if your nausea is tied to slow digestion or constipation. Works in 65-70% of cases, but high doses can cause muscle spasms.
- Ondansetron (4-8 mg every 8 hours): Blocks serotonin, which helps with chemo nausea-but it’s less reliable for opioid-induced nausea. Studies show it’s only moderately effective, and it’s expensive. A single 4 mg tablet can cost $3.50.
- Dexamethasone (4-8 mg IV or oral): Used in hospitals, especially for cancer patients. Helps about half the time, but we don’t fully understand how.
Pro tip: Avoid using ondansetron as your first choice unless you’ve tried dopamine blockers and they didn’t work. It’s not wrong-it’s just not the most effective tool for this job.
Timing Matters: When to Take the Antiemetic
Most people take their anti-nausea pill after they feel sick. That’s too late. Opioids peak in your bloodstream 60 to 90 minutes after you swallow them. If you want to stop nausea before it starts, you need the antiemetic ready.
Take your antiemetic 30 to 60 minutes before your opioid dose. That way, the antiemetic is already working when the opioid hits your brain. This simple shift cuts nausea severity by up to 50% in clinical practice.
For example: If you take morphine at 8 a.m., take prochlorperazine at 7:15 a.m. If you take oxycodone at 4 p.m., take metoclopramide at 3 p.m. This isn’t guesswork-it’s pharmacology.
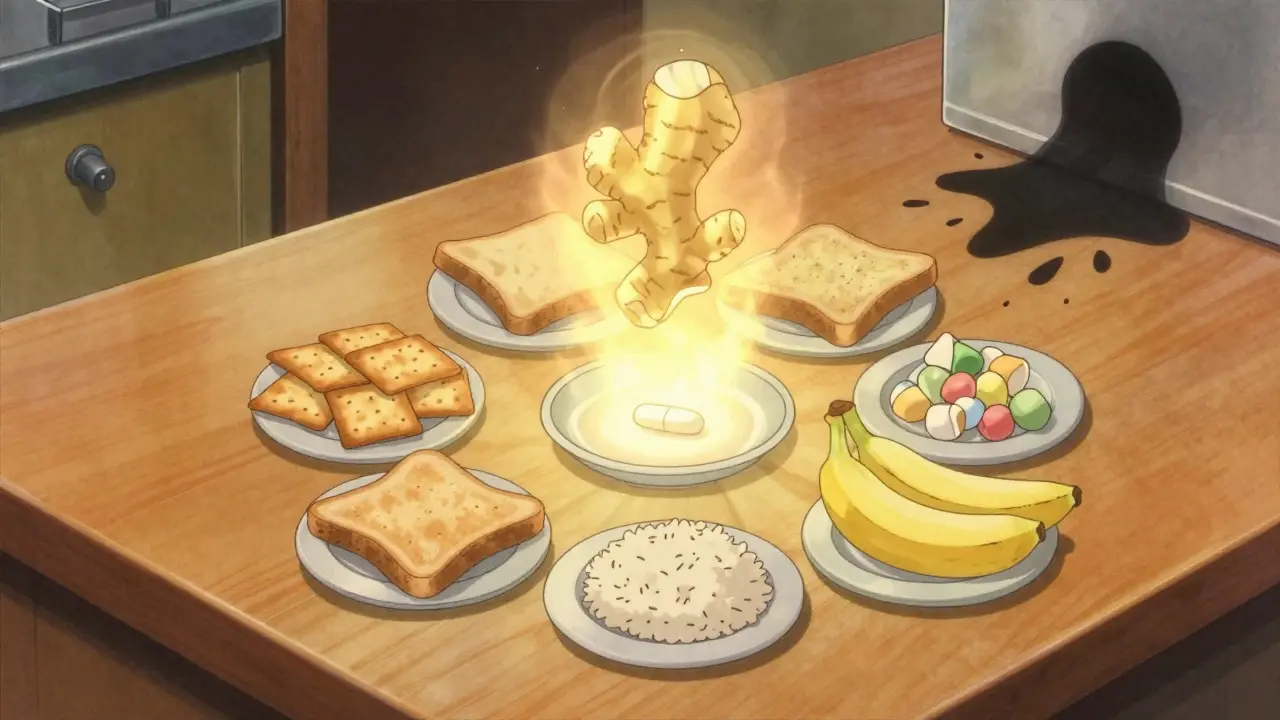
Diet Adjustments That Actually Help
There’s no magic food that cures opioid nausea, but what you eat-and when-can make a big difference.
- Eat small, frequent meals. Large meals slow digestion and make nausea worse. Try 5-6 small snacks instead of 3 big meals.
- Avoid greasy, spicy, or sweet foods. These are harder to digest and can trigger nausea more easily.
- Stick to bland, dry foods. Crackers, toast, rice, and bananas are easier on the stomach. Ginger tea or ginger candies can help too-some studies show ginger reduces nausea in cancer patients on opioids.
- Don’t lie down after eating. Wait at least 30 minutes. Gravity helps keep food down.
- Stay hydrated, but sip slowly. Chugging water can make nausea worse. Try sipping ice chips, clear broth, or electrolyte drinks.
One overlooked factor: constipation. Opioids slow your bowels. That buildup can make you feel nauseous even if your stomach is empty. If you’re constipated, treating that with stool softeners or laxatives often reduces nausea too.
The ‘Start Low, Go Slow’ Method
One of the most effective ways to prevent opioid nausea isn’t a pill-it’s how you start the medication.
Instead of jumping to a standard dose, begin with 25-50% of the usual starting amount. For example, if the typical starting dose of morphine is 10 mg every 4 hours, begin with 2.5-5 mg instead. Increase slowly-only by 25-50% every 24-48 hours-until your pain is controlled.
This approach reduces nausea by 35-40%, according to palliative care experts. It also gives your body time to adjust. You might take 7-10 days to reach your full pain dose, but you’ll avoid the worst of the nausea.
Many doctors skip this step because they want quick pain relief. But if you’re too nauseated to take your meds, you’re not getting pain control at all.
When to Switch Opioids
If nausea sticks around after 7-10 days, even with antiemetics and diet changes, it might be time to switch opioids.
Not all opioids cause the same level of nausea. Here’s what the data shows:
- Morphine → Oxycodone: May help a little. Evidence is weak.
- Morphine → Methadone: Better chance of success. Methadone has a different chemical structure and often causes less nausea. But switching requires careful dosing-don’t do this without a specialist.
- Morphine → Hydromorphone: Newer data from the NCCN suggests 40-50% of patients see reduced nausea after switching.
- Tramadol → Codeine or Hydrocodone: Tramadol is more likely to cause nausea than other opioids. Switching can help.
Don’t switch just because you’re nauseous. Wait at least 5-7 days on a stable dose with antiemetics first. But if nausea is still breaking your tolerance, talk to your doctor about rotation.
What Doesn’t Work
Some strategies sound logical but don’t hold up in studies:
- Prophylactic antiemetics (taking them before starting opioids): A 2019 review of 619 patients found they don’t prevent nausea. Only treating it after it starts works.
- Antihistamines like dimenhydrinate (Dramamine): They help with motion sickness, but not opioid nausea.
- Waiting it out without any intervention: Yes, tolerance develops-but many people quit before that happens. Don’t suffer needlessly.
What to Do If Nothing Seems to Work
If you’ve tried antiemetics, timing, diet, and opioid rotation-and you’re still nauseous-talk to your doctor about two things:
- Can you lower your opioid dose? Surprisingly, reducing your dose by 25-33% can still give you good pain relief while eliminating nausea in about 60% of cases.
- Are there non-opioid options? For some types of pain (nerve pain, arthritis), medications like gabapentin, duloxetine, or even physical therapy can reduce opioid needs.
Remember: Pain control and nausea control aren’t enemies. They can be balanced. You don’t have to choose between them.
Final Thoughts: You’re Not Alone
Opioid-induced nausea is common, frustrating, and often misunderstood. But it’s not inevitable. With the right combination of timing, medication, diet, and dose adjustment, most people get through it. The key is acting early-not waiting until you’re vomiting every time you take your pill.
Work with your doctor. Track your symptoms. Try one change at a time. And don’t give up. Better pain control is possible-and you don’t have to suffer to get it.
How long does opioid nausea last?
For most people, opioid-induced nausea lasts 3 to 7 days after starting the medication or increasing the dose. Tolerance usually develops by then, and nausea fades. If it lasts longer than 10 days, other factors like constipation, dehydration, or an unsuitable opioid may be involved.
Can I take anti-nausea medicine with my opioid?
Yes, and you should. Antiemetics like haloperidol, prochlorperazine, and metoclopramide are safe to take with opioids. They don’t interfere with pain relief. Always check with your doctor about possible interactions, especially if you’re on other medications like antidepressants or antifungals, which can affect liver enzymes.
Is it safe to use ginger for opioid nausea?
Ginger is generally safe and may help reduce nausea. Studies show it can be effective for chemotherapy-related nausea, and many patients report similar benefits with opioids. Try ginger tea, ginger chews, or capsules (500 mg up to 4 times daily). It’s not a replacement for prescribed antiemetics, but it can be a helpful addition.
Why do some people get nausea and others don’t?
Genetics, age, and prior exposure play roles. Older adults and people with a history of motion sickness or migraines are more likely to experience opioid nausea. People who’ve taken opioids before may have built tolerance. Also, the type and dose of opioid matter-morphine and codeine are more likely to cause nausea than methadone or fentanyl.
Can I stop my opioid if the nausea is too bad?
Don’t stop abruptly without talking to your doctor. Sudden withdrawal can cause other symptoms like anxiety, sweating, and increased pain. Instead, ask about lowering your dose, switching opioids, or adjusting your antiemetic. You can manage the nausea and still get pain relief.
Do antiemetics cause side effects?
Yes, but they’re usually mild. Haloperidol can cause drowsiness or muscle stiffness, especially in older adults. Metoclopramide may cause restlessness or spasms at high doses. Prochlorperazine can cause dry mouth or dizziness. These are often worth the trade-off for relief from vomiting. If side effects are severe, your doctor can switch you to another antiemetic.

Vinayak Naik
January 7, 2026 AT 05:31Man, this post is a godsend. I was about to quit my pain meds after day 2 of nausea like I’d swallowed a whole fish tank. Tried haloperidol at 7:15 before my morphine-boom, no more vomiting. Just felt like a zombie for a bit, but hey, I can actually eat toast now. 🙌
Kiran Plaha
January 7, 2026 AT 23:04Thanks for sharing this. I didn’t know timing mattered this much. I was taking my anti-nausea pill after I felt sick. Big mistake. Will try it before next dose.
Amy Le
January 8, 2026 AT 20:04Wow. Finally someone who doesn’t treat opioids like magic fairy dust. Also, ginger? Cute. But if you’re still vomiting after 7 days, maybe you’re just not supposed to be on opioids. 💅
Pavan Vora
January 9, 2026 AT 19:55Interesting… very interesting. I’ve seen this in my uncle-he switched from morphine to methadone after 11 days of misery. But the dosing? Oh my god, it’s like threading a needle with a chainsaw. Please, please, please consult a specialist. I don’t want anyone to die because they googled it.
Indra Triawan
January 10, 2026 AT 16:44I’ve been on opioids for 6 months now. Nausea never went away. I cried every morning. I felt so alone. I thought it was me. Like I was weak. But reading this… I don’t feel so broken anymore.
Tom Swinton
January 12, 2026 AT 01:22Let me just say-this is the kind of information that should be handed out with every opioid prescription. Not just a little pamphlet that says ‘side effects may include nausea’-no, give people this. Give them the full playbook. Because if you’re suffering and you don’t know what to do, you’re not failing-you’re just uneducated. And that’s on the system, not you. You deserve to feel better. You deserve to live without vomiting every time you take your medicine. Don’t let anyone make you feel like you’re overreacting. You’re not. You’re surviving. And you’re not alone.
Venkataramanan Viswanathan
January 13, 2026 AT 00:50While the pharmacological details are commendable, one must also consider the cultural context in which such interventions are implemented. In many parts of India, for instance, access to haloperidol or even prochlorperazine is severely restricted. Moreover, the notion of ‘timing’-taking medication 30 minutes prior-is often impractical for laborers or those without refrigeration or consistent meal schedules. A systemic solution is required, not merely a pharmacological one.
Kelly Beck
January 14, 2026 AT 08:45You guys are doing amazing work just by sharing this. Seriously. I know how scary it is to start opioids-you feel like you’re betraying yourself by needing them. But you’re not. You’re healing. And if you’re reading this and you’re scared? I’ve been there. I took metoclopramide before my oxycodone and I didn’t throw up once for two weeks. You can do this. One pill at a time. You’re not weak. You’re brave. 💪❤️
Katie Schoen
January 15, 2026 AT 17:00So… you’re telling me I didn’t need to suffer for 10 days because I was ‘just being dramatic’? Wow. Mind blown. Also, ginger tea is now my new best friend. Who knew?
Beth Templeton
January 16, 2026 AT 22:11Ondansetron is overpriced junk. Done.
Dana Termini
January 17, 2026 AT 14:37This is so helpful. I’ve been trying to help my mom through this, and I had no idea about the timing thing. I’m going to print this out and take it to her doctor tomorrow. Thank you.
Isaac Jules
January 19, 2026 AT 06:55Of course the answer is ‘just switch opioids’-because that’s totally easy when you’re already on 80mg of morphine and your insurance only covers one brand. Also, ‘start low’? Yeah, right. My doctor gave me a 10mg tablet and said ‘take one every 4 hours.’ No adjustment. No follow-up. Just ‘hope it works.’ Thanks for the textbook advice, but real life doesn’t come with a manual.
Stuart Shield
January 20, 2026 AT 08:40Brilliant breakdown. I’ve been a palliative nurse for 18 years and this is exactly how we train new staff. The ‘30-minute rule’? Absolute gold. And the ginger? I’ve seen patients light up after trying it-especially when they’re too nauseous to swallow pills. One old lady in Glasgow started chewing raw ginger root. Said it tasted like ‘fighting a dragon,’ but she slept through the night for the first time in weeks. Weird? Maybe. Effective? Hell yes.
Leonard Shit
January 20, 2026 AT 15:18Wait so you’re saying I didn’t have to quit my meds because I was ‘too sensitive’? I thought it was me… I thought I was broken. I’ve been on this for 3 weeks. Took prochlorperazine before my dose today… no vomit. Just… quiet. I don’t know what to feel. But I’m not crying anymore. Thank you.
Brian Anaz
January 21, 2026 AT 05:30This is why America’s opioid crisis is so stupid. People don’t know how to use the drugs. It’s not the drugs. It’s the idiots taking them without reading. If you’re vomiting, take the antiemetic. Simple. No drama. No ‘I’m special.’ Just follow the science. Stop being dramatic.