Every time you pick up a prescription, the label on that bottle or box isn’t just a sticker-it’s your first line of defense against a medication error. You might think, “It’s from my regular pharmacy, so it’s fine.” But mistakes happen. A wrong name. A misprinted number. A prescription meant for someone else. And if you don’t check, you could end up taking the wrong drug, at the wrong dose, or worse.
The FDA says 1.3 million injuries and over 7,000 deaths each year in the U.S. come from medication errors. About 12% of those are tied to incorrect prescriber or pharmacy info on the label. That’s not a small risk. It’s something you can stop-right now-by spending just 60 seconds checking what’s printed on your label.
What to Look for on Your Prescription Label
Your medication label isn’t just a reminder of what to take. It’s a legal document. By law, it must include specific details to keep you safe. Here’s what you need to find, every single time:
- Prescriber’s full name - Not “Dr. J.” or “PCP.” It should be the full legal name of the person who wrote the prescription. If you saw Dr. Lisa Chen for your high blood pressure, but the label says Dr. Robert Kim, that’s a red flag.
- National Provider Identifier (NPI) number - A 10-digit number assigned to every licensed healthcare provider in the U.S. It’s unique to them. You won’t need to memorize it, but if you’re unsure, call the pharmacy and ask them to confirm the NPI matches your prescriber’s.
- Prescription number - Usually starts with “Rx” or “#.” This is the key to refills. If the number doesn’t match what your pharmacy gave you last time, don’t take the pills.
- Pharmacy name and address - Should be the full legal name, not just “CVS.” If you ordered from a mail-order pharmacy, it might say “Express Scripts Pharmacy” or “Walgreens Mail Service.” If you picked it up locally, it should say the name of your neighborhood pharmacy.
- Pharmacy phone number - This is the number to call with questions. Don’t rely on the prescriber’s office. The pharmacy’s number is your direct line to a pharmacist who knows your meds.
- Pharmacist’s name (in 42 states) - Not required everywhere, but if it’s there, it’s a good sign. It means someone took responsibility for filling your prescription.
These aren’t suggestions. They’re requirements under 21 CFR 1306.22 and state pharmacy board rules. If any of these are missing, the pharmacy is out of compliance. And you should walk away until it’s fixed.
When to Verify: Three Critical Moments
Don’t wait until you’re standing at your kitchen counter with the bottle in hand. Verify at three points:
- When you first receive the medication - Check it right there at the pharmacy counter. Don’t just grab it and leave. Ask the pharmacist: “Can you confirm this is for me and matches what my doctor ordered?”
- Before you take the first dose - Even if it looked right at the pharmacy, check again at home. You might have missed something in the rush. Compare the label to your doctor’s note or your own records.
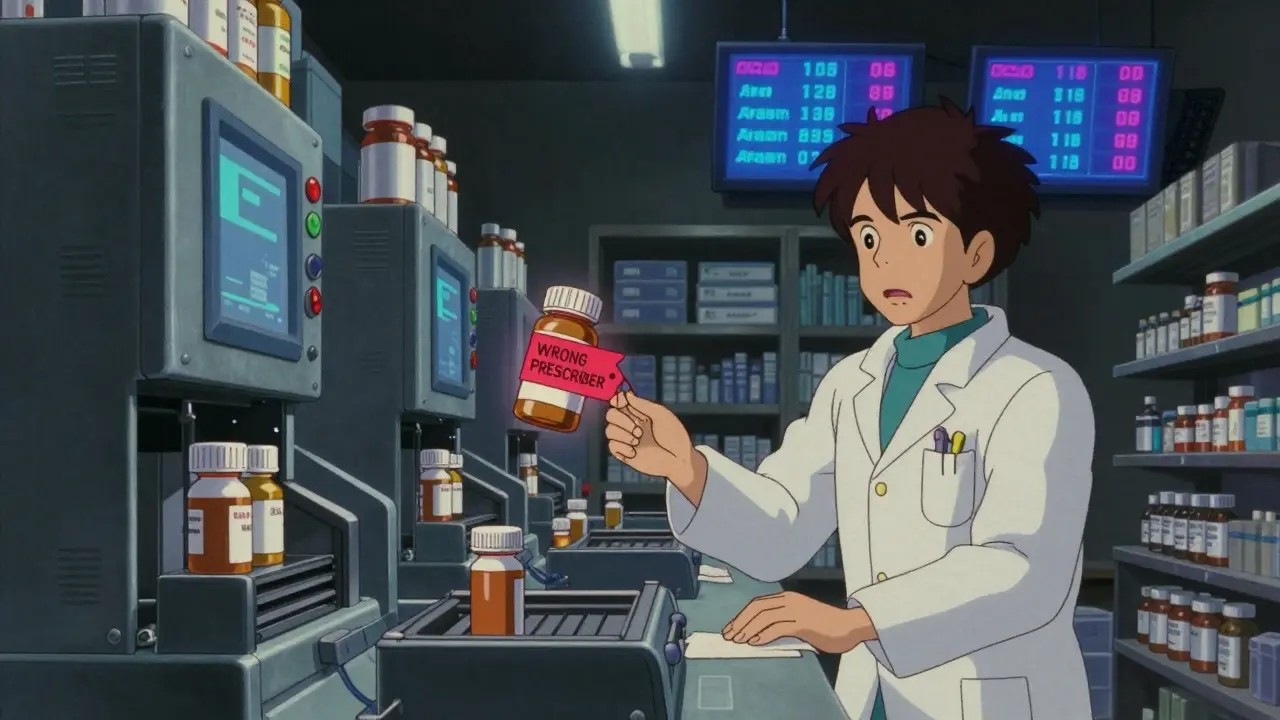
- Every time you refill - Prescriptions get mixed up during refill processing. One patient on Reddit found a Schedule II opioid labeled with their dentist’s name instead of their cardiologist. That’s not a typo. That’s a dangerous error.
A 2023 study in the Journal of the American Pharmacists Association found that physical label verification has a 2.1% error rate. Mobile apps? 7.2%. Why? Because apps can auto-fill wrong data. Labels don’t lie. They’re printed, not programmed.

Common Mistakes and How to Catch Them
Most errors aren’t random. They follow patterns. Here’s what usually goes wrong-and how to spot it:
- Misspelled prescriber names - 42% of reported errors. “Dr. Smith” becomes “Dr. Smyth.” Sounds harmless, but if the real Dr. Smith never treated you, this could mean someone else’s prescription got mixed in.
- Wrong specialty - 28% of errors. A dentist prescribing a heart medication? A psychiatrist prescribing a controlled painkiller? That’s a mismatch. Prescribers can only legally write certain types of prescriptions based on their license.
- Electronic prescription glitches - 18% of failures come from E-prescribing systems auto-filling the wrong provider. Happens often when doctors share offices or use templates.
- Mail-order pharmacy mix-ups - These pharmacies handle 23% more errors than local ones. Why? Higher volume, less face-to-face interaction. If you get a label from a mail-order pharmacy and it looks off, call them immediately.
One real case from the ISMP Medication Safety Alert in January 2024: A patient noticed the prescriber name didn’t match their cardiologist. They called the pharmacy. Turns out, the pharmacy had filled a different patient’s prescription for the same drug. That patient was on blood thinners. The wrong person could’ve had a stroke.
What to Do If Something’s Wrong
If you spot a mistake, don’t guess. Don’t assume it’s “probably fine.”
- Call the pharmacy - Use the number on the label. Ask: “I’m checking my prescription. The prescriber name says [name], but I was treated by [correct name]. Can you confirm this is correct?”
- Ask for the pharmacist to spell the name - If the name looks unfamiliar, ask them to say it out loud. “Is that S-M-I-T-H or S-M-Y-T-H?”
- Don’t take the medication - Until you get confirmation from the pharmacy, leave it sealed.
- Ask for a printed copy of the original prescription - Pharmacies are required to keep this on file. You have the right to see it.
- Report it - If the pharmacy doesn’t fix it, or if you suspect a pattern, report it to the FDA’s MedWatch program. You can do it online. It helps protect others.
Patients who verify their labels report 27% fewer medication errors and 31% higher adherence to their treatment plans. That’s not magic. It’s awareness.
Tools to Help You Verify
You don’t need to remember everything. Here’s how to make verification easier:
- Keep a personal medication record - Write down: drug name, dose, prescriber, pharmacy, and date. Update it every time you get a new script. Most major pharmacies (CVS, Walgreens, etc.) offer free digital versions in their apps.
- Use a magnifying glass - If the print is too small (a problem for 37% of people over 65), ask the pharmacy for a larger-print label. Most will print it for free.
- Ask for help - If a name is hard to read, ask the pharmacist to read it aloud. Don’t feel awkward. They’ve seen this before.
- Use QR codes (new in 2024) - Some pharmacies are testing QR codes on labels that link to a digital page with verified prescriber info. Early results show a 19% improvement in accuracy. Ask your pharmacy if they offer it.
The FDA’s 2024 strategic plan wants 75% of U.S. adults to verify their labels by 2027. Right now, only 62% do. That gap? It’s fixable. With your attention.
Why This Matters More Than You Think
Some people say, “I trust my doctor. I trust my pharmacy.” But trust isn’t a safety system. Systems fail. People make mistakes. Even the best pharmacies have errors. The 2023 NABP audit showed community pharmacies have a 98.7% accuracy rate. That sounds great-until you realize that means 1 in 75 prescriptions still has an issue.
And here’s the hard truth: 14% of labels that look perfect still contain clinically dangerous errors-like wrong dosage, wrong drug, or wrong instructions-that patients can’t spot on their own. That’s why verification isn’t the end of the process. It’s the beginning. Always follow up with your doctor or pharmacist if something feels off, even if the label looks right.
Medication safety isn’t about being paranoid. It’s about being informed. You’re not just a patient. You’re the last checkpoint in a long chain of care. Your eyes on that label could save your life.
What if the prescriber name on my label doesn’t match my doctor?
Don’t take the medication. Call the pharmacy using the number on the label. Ask them to confirm the prescription was meant for you and matches your doctor’s name. If they can’t verify it, ask for a copy of the original electronic or paper prescription. If the pharmacy refuses to fix it, contact your doctor’s office and report the issue to the FDA’s MedWatch program.
Is it safe to rely on my pharmacy’s app instead of checking the physical label?
No. A 2023 study found that mobile app verification has a 7.2% error rate, compared to just 2.1% for physical label checks. Apps can auto-fill wrong information, especially with electronic prescriptions. The physical label is printed directly from the pharmacy’s system and is the most reliable source. Use the app as a supplement, never a replacement.
Can a pharmacy legally fill a prescription without the prescriber’s NPI number?
No. Under federal law (21 CFR 1306.22), all controlled substance prescriptions must include the prescriber’s full name and NPI number. For non-controlled prescriptions, most states require the same. If the NPI is missing, the pharmacy is violating regulations. You have the right to ask for a corrected label or to take the prescription to another pharmacy.
Why do mail-order pharmacies have more errors than local ones?
Mail-order pharmacies process far more prescriptions daily and often use automated systems with less direct pharmacist oversight. A 2022 CMS analysis found they have a 23% higher error rate than community pharmacies. They also rarely offer face-to-face verification. Always double-check your label when you receive mail-order meds.
What should I do if I’ve already taken the wrong medication?
Stop taking it immediately. Call your pharmacist or doctor. If you’re experiencing symptoms like dizziness, nausea, rapid heartbeat, or confusion, call 911 or go to the nearest emergency room. Even if you feel fine, report the incident to the pharmacy and the FDA’s MedWatch program. Document the label details and keep the bottle as evidence.


Stephen Tulloch
January 17, 2026 AT 00:42Melodie Lesesne
January 17, 2026 AT 02:32Corey Sawchuk
January 18, 2026 AT 18:20Joie Cregin
January 19, 2026 AT 02:11Allen Davidson
January 19, 2026 AT 02:31john Mccoskey
January 20, 2026 AT 09:41Ryan Hutchison
January 20, 2026 AT 22:35Samyak Shertok
January 22, 2026 AT 14:01Rob Deneke
January 24, 2026 AT 03:59evelyn wellding
January 25, 2026 AT 23:17Chelsea Harton
January 27, 2026 AT 19:06vivek kumar
January 28, 2026 AT 22:22Nick Cole
January 29, 2026 AT 16:27Cheryl Griffith
January 30, 2026 AT 09:33Isabella Reid
February 1, 2026 AT 07:35