HCTZ Drug Interaction Checker
Taking any prescription comes with a hidden checklist: what else are you on? For Hydrochlorothiazide is a thiazide diuretic that lowers blood pressure and reduces fluid buildup, that list matters a lot. Missing a risky combo can mean a sudden drop in electrolytes, a spike in blood pressure, or even kidney trouble. Below you’ll find the most common drug families that should stay clear of HCTZ, why the chemistry clashes, and practical steps to keep you safe.
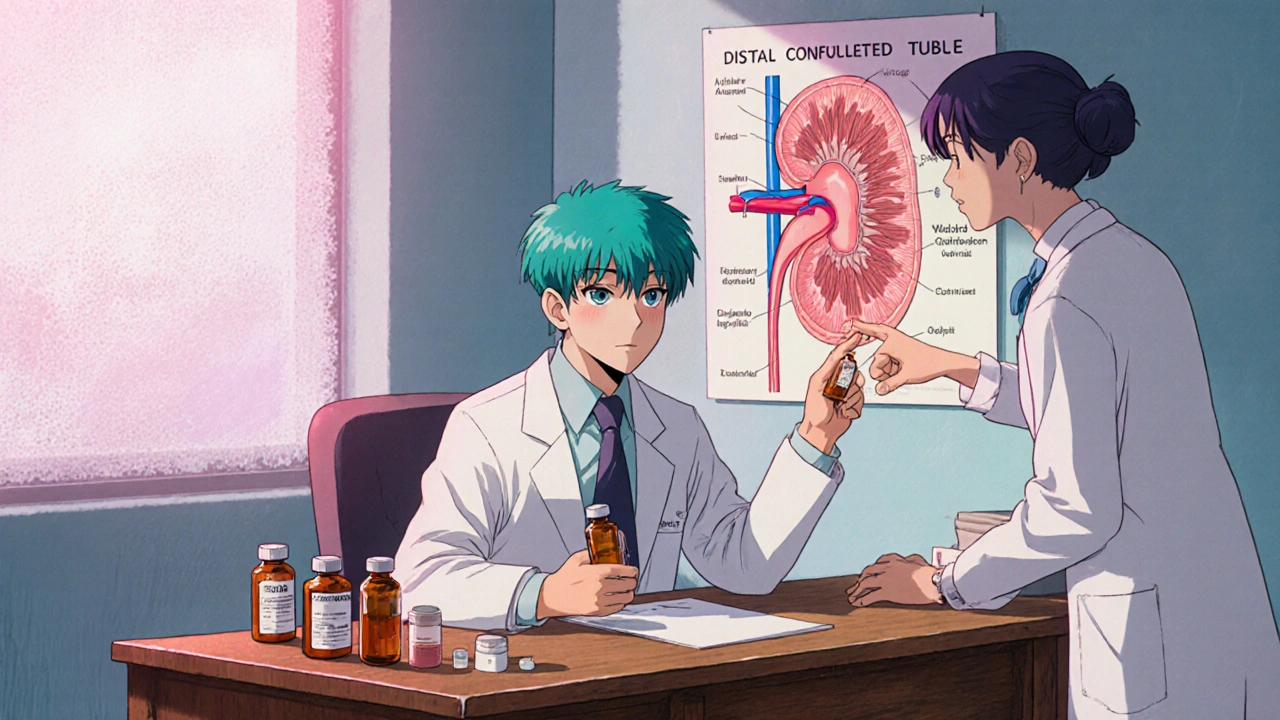
How Hydrochlorothiazide Works
HCTZ acts on the distal convoluted tubule in the kidney, blocking sodium‑chloride reabsorption. Less sodium stays in the bloodstream, water follows, and blood pressure drops. The side effect? The kidneys also lose potassium, magnesium, and calcium along the way, which is why many interactions revolve around electrolyte balance.
Why Interactions Matter
When another drug pushes the same physiological levers-or interferes with HCTZ’s elimination pathway-the result can be a dangerous swing in blood pressure, heart rhythm, or kidney function. Some combos simply blunt HCTZ’s effect, leaving hypertension uncontrolled. Others amplify electrolyte loss, leading to muscle cramps, arrhythmias, or severe dehydration. Knowing the culprits lets clinicians adjust doses or pick safer alternatives before problems surface.
Medication Classes to Avoid or Use With Caution
- Non‑steroidal anti‑inflammatory drugs (NSAIDs) - e.g., ibuprofen, naproxen, diclofenac. NSAIDs reduce kidney prostaglandin production, counteracting the diuretic effect of HCTZ and raising blood pressure.
- Lithium - used for bipolar disorder. Lithium has a narrow therapeutic window that shrinks when HCTZ causes sodium loss, increasing lithium toxicity risk.
- ACE inhibitors and ARBs - e.g., lisinopril, losartan. They boost potassium levels, which can clash with HCTZ‑induced hypokalemia, leading to unpredictable potassium swings.
- Antidiabetic agents (especially sulfonylureas) - e.g., glipizide, glyburide. HCTZ can raise blood glucose, making these drugs less effective and increasing hypoglycemia risk.
- Warfarin - a blood thinner. HCTZ can enhance warfarin’s anticoagulant effect by displacing it from plasma proteins, raising bleeding risk.
- Digoxin - for heart failure or atrial fibrillation. Low potassium from HCTZ heightens digoxin toxicity, which may present as nausea, visual changes, or arrhythmias.
- Allopurinol - for gout. When combined with HCTZ, serum uric acid may rise, worsening gout attacks.
- Cytochrome P450 (CYP) inhibitors - e.g., fluconazole, erythromycin. Though HCTZ isn’t heavily metabolized by CYP enzymes, strong inhibitors can affect its renal clearance in some patients.
Detailed Look at High‑Risk Interactions
NSAIDs + HCTZ
NSAIDs reduce prostaglandin synthesis, narrowing the blood vessels that deliver blood to the kidneys. HCTZ already limits fluid volume; the double hit can cause acute kidney injury (AKI). Watch for rising creatinine, reduced urine output, or sudden swelling.
Lithium + HCTZ
Thiazides increase lithium reabsorption in the proximal tubule, pushing serum levels up 50‑100%. Even a mild tremor may signal toxicity. If a patient needs both, lower lithium dose by 25‑50% and check serum lithium within a week.
ACE Inhibitors/ARBs + HCTZ
These agents raise potassium, while HCTZ pushes it down. The net effect varies per individual; routine electrolyte panels are a must, especially after dose changes.
Warfarin + HCTZ
Protein‑binding displacement can lift the INR by 0.5-1.0 points. A sudden jump heightens bleeding risk, so clinicians often check INR 2-3 days after initiating or adjusting HCTZ.
Digoxin + HCTZ
Low potassium sensitizes heart tissue to digoxin, increasing the chance of ventricular arrhythmias. Keep potassium above 4.0 mmol/L and monitor digoxin levels weekly during the first month of combined therapy.
Practical Strategies to Manage Interactions
- Review the full medication list at every visit-prescriptions, over‑the‑counter drugs, and supplements.
- Order baseline labs: serum electrolytes (K+, Mg2+, Ca2+), creatinine, fasting glucose, and INR if the patient is on warfarin.
- Schedule follow‑up labs 1-2 weeks after starting HCTZ or after any dose change.
- If a high‑risk combo is unavoidable, adjust the dose of the interacting drug and set a tighter monitoring schedule.
- Educate patients to report symptoms such as muscle weakness, irregular heartbeat, excessive bruising, or sudden weight gain.
- Consider potassium‑sparing alternatives (e.g., chlorthalidone with a low‑dose potassium supplement) when hypokalemia is recurrent.
Interaction Severity Table
| Medication Class | Typical Effect | Clinical Significance | Management |
|---|---|---|---|
| NSAIDs | Reduced diuretic efficacy, possible AKI | High | Avoid concurrent use; if needed, monitor creatinine & electrolytes. |
| Lithium | Increased lithium levels → toxicity | High | Reduce lithium dose; check serum lithium 3-5 days after HCTZ start. |
| ACE inhibitors / ARBs | Opposing potassium effects | Medium | Check potassium weekly; adjust doses if needed. |
| Warfarin | Elevated INR, bleeding risk | Medium | Re‑check INR within 48 h of HCTZ initiation. |
| Digoxin | Enhanced toxicity via hypokalemia | Medium | Maintain K+ >4.0 mmol/L; monitor digoxin levels. |
| Antidiabetics (sulfonylureas) | Higher glucose levels | Low‑Medium | Check fasting glucose; adjust antidiabetic dose if needed. |
| Allopurinol | Increased uric acid → gout flare | Low | Monitor uric acid; consider dose reduction. |
Quick Checklist for Patients and Providers
- Ask about any over‑the‑counter NSAID use (including topical creams).
- Review psychiatric meds-particularly lithium.
- Confirm anticoagulant status (warfarin, DOACs) before starting HCTZ.
- Schedule labs within 1-2 weeks of any dose change.
- Educate on signs of low potassium: muscle cramps, irregular heartbeat.
- Keep a medication list handy and update it at every visit.
Frequently Asked Questions
Can I take ibuprofen for a headache while on hydrochlorothiazide?
Occasional low‑dose ibuprofen is usually safe, but it can blunt HCTZ’s blood‑pressure‑lowering effect and strain the kidneys. If you need regular pain relief, talk to your doctor about a safer alternative like acetaminophen.
Why does hydrochlorothiazide raise my blood sugar?
Thiazides cause mild insulin resistance and reduce potassium, which both push glucose higher. Monitoring fasting glucose and adjusting antidiabetic meds can keep levels in check.
Is it safe to combine HCTZ with a potassium supplement?
Yes, many clinicians prescribe a low‑dose potassium chloride tablet to counteract HCTZ‑induced loss, but the dose must be individualized. Too much potassium can cause its own heart rhythm problems.
What should I do if I miss a dose of hydrochlorothiazide?
Take the missed tablet as soon as you remember, unless it’s almost time for the next dose. In that case, skip the missed one and continue with your regular schedule. Doubling up can trigger sudden drops in blood pressure.
Can hydrochlorothiazide cause gout attacks?
Yes. HCTZ reduces uric acid excretion, so serum uric acid may rise, triggering gout in susceptible people. If you have a history of gout, your doctor may choose a different diuretic or prescribe allopurinol.
Understanding hydrochlorothiazide interactions isn’t rocket science, but it does save you from avoidable hospital visits. Keep an up‑to‑date medication list, stay on top of lab checks, and never assume an over‑the‑counter product is automatically safe. Your health-and peace of mind-depends on it.

Harry Bhullar
October 21, 2025 AT 00:13When you start a patient on hydrochlorothiazide it’s worth treating the prescription like a mini‑project with several checkpoints. First, grab a baseline panel that includes potassium, magnesium, calcium, creatinine, fasting glucose and, if the patient is on an anticoagulant, the INR. Next, schedule a follow‑up lab draw in about one to two weeks; this catches the early dip in potassium that can predispose to arrhythmias. If the potassium is low, consider adding a low‑dose potassium chloride tablet or switching to a potassium‑sparing thiazide like chlorthalidone. For patients on lithium, remember that thiazides boost lithium reabsorption, so you’ll need to drop the lithium dose by roughly a quarter and re‑check serum lithium levels within five days. NSAIDs are a classic antagonist: they blunt the diuretic effect and can precipitate acute kidney injury, so advise patients to limit ibuprofen or naproxen usage and monitor serum creatinine if they can’t avoid them. When a patient is on an ACE inhibitor or ARB, watch the potassium trend closely because the drugs push potassium up while HCTZ pulls it down, creating a tug‑of‑war that can swing either way. Warfarin users should have their INR rechecked 48 hours after any dose change in HCTZ because the drug can displace warfarin from plasma proteins, nudging the INR higher. Diabetics on sulfonylureas may see a modest rise in blood glucose; a dose adjustment or an alternative agent can keep glycemic control on track. Gout patients should be warned that HCTZ reduces uric acid excretion, potentially sparking a flare, so prophylactic allopurinol or a different diuretic may be prudent. Lastly, always ask about over‑the‑counter meds and herbal supplements, because something as innocuous as a topical diclofenac gel can still affect renal prostaglandins. By building this systematic approach you’ll reduce the chance of an unexpected emergency visit and keep the therapeutic benefits of hydrochlorothiazide intact.
Dana Yonce
October 25, 2025 AT 15:46Got it! 👍
Kimberly Lloyd
October 30, 2025 AT 05:53It’s easy to feel overwhelmed by all those lab numbers, but think of each test as a little compass pointing toward safety. A calm mind can turn those numbers into actionable steps, like a potassium boost or a gentle switch of pain reliever. Remember, the goal isn’t just to avoid trouble, but to keep living well while on medication.
Chirag Muthoo
November 3, 2025 AT 21:00Indeed, precise monitoring is indispensable; without it, the therapeutic window may be inadvertently breached, compromising patient safety.
Lolita Gaela
November 8, 2025 AT 12:06From a pharmacokinetic perspective, the diuretic’s impact on proximal tubular sodium exchange can potentiate lithium’s bioavailability, necessitating a recalibration of the therapeutic index to mitigate neurotoxicity; similarly, the antagonistic effect of NSAIDs on renal prostaglandin synthesis can attenuate natriuresis, fostering iatrogenic azotemia.
Giusto Madison
November 13, 2025 AT 03:13Listen, if you’re still popping ibuprofen daily while on HCTZ, you’re basically asking for a kidney disaster – cut the NSAIDs or your blood pressure will spike, period.
Ivan Laney
November 17, 2025 AT 18:20Look, the United States prides itself on being a land of freedom, but that freedom comes with responsibility, especially when it concerns your health; you cannot simply ignore drug interactions because you think you’re invincible, and the science is crystal clear – hydrochlorothiazide can derail the delicate electrolyte balance that keeps your heart beating in rhythm, and when you add a careless mix of over‑the‑counter painkillers, lithium, or even certain blood thinners, you are courting a catastrophe that could land you in an emergency room, which, let’s be honest, is not the American Dream you signed up for; therefore, educate yourself, keep a comprehensive medication list, and demand thorough monitoring from your provider, because a well‑informed patient is the best defense against the chaos of adverse drug events.
Sakib Shaikh
November 22, 2025 AT 09:26Yo, HCTZ + ibuprofenn = oops, kidney blowout!!!
Angela Koulouris
November 27, 2025 AT 00:33Think of your body as a garden; HCTZ is the gardener that trims excess water, but you still need to fertilize with potassium and watch out for weeds like NSAIDs that can choke the roots.
erica fenty
December 1, 2025 AT 15:40HCTZ interaction checklist: NSAIDs, lithium, ACE‑I/ARBs, warfarin, digoxin, sulfonylureas, allopurinol – monitor labs, adjust doses, stay safe.
Xavier Lusky
December 6, 2025 AT 06:46Big pharma doesn’t want you to know that combined drugs can be a hidden weapon against your health.
Ashok Kumar
December 10, 2025 AT 21:53Sure, “just take the pills” – because ignoring electrolyte shifts has never caused any real problems, right? (Sarcasm intended.)
Jasmina Redzepovic
December 15, 2025 AT 13:00Patriotic citizens should demand that our healthcare system enforce strict guidelines on hydrochlorothiazide co‑prescriptions to protect national health security.
Esther Olabisi
December 20, 2025 AT 04:06Wow, so many meds to watch – better keep that list handy and maybe add a ✅ emoji for each safe combo! 😅🎉