Opioid Itching Risk & Treatment Selector
Opioid-Induced Itching: What You Need to Know
Opioid-induced itching affects 30-100% of patients depending on the opioid and administration route. It's not an allergic reaction - it's caused by nerve pathways activated by opioids.
Select Your Opioid
Your Results
Itching Risk
Recommended Treatment
Select an opioid and route to see treatment options.
When you take an opioid like morphine for pain after surgery or during childbirth, you expect relief - not a burning, crawling itch that makes you want to scratch your skin off. Yet for 30 to 100% of people receiving spinal or epidural opioids, this happens. It’s not an allergy. It’s not dry skin. It’s opioid-induced pruritus - a side effect so common, so disruptive, and so misunderstood that many patients end up refusing pain meds altogether.
Why Do Opioids Make You Itch?
For decades, doctors thought opioid itching was just like an allergic reaction - caused by histamine bursting out of mast cells in your skin. That’s why they reached for diphenhydramine (Benadryl) first. But that approach often fails. Why? Because histamine isn’t the main culprit in most cases. Modern research shows two separate pathways are at work. One involves histamine - yes, it plays a role, especially in cases with hives or redness. But the bigger story is neural. Opioids bind directly to mu opioid receptors (MORs) on nerve fibers in your spinal cord and skin. These receptors aren’t just for pain. They’re wired to trigger itch signals too. The key players? TRPV1-expressing neurons in your dorsal root ganglia. When morphine activates them, your brain gets an itch signal - even if your skin is perfectly normal. This explains why scratching doesn’t help. It’s not your skin. It’s your nerves. And it’s why antihistamines only work for about 1 in 4 people.Which Opioids Cause the Most Itching?
Not all opioids are equal when it comes to itching. The route of administration matters just as much as the drug itself.- Intrathecal morphine (injected into the spinal fluid): 70-100% of patients get itchy. This is common in C-sections and post-op pain pumps.
- Intravenous morphine: 30-50% of patients report itching, often within 15-30 minutes.
- Oral opioids (like oxycodone or hydrocodone): Only 10-30% experience itching. Lower concentrations and slower absorption reduce the effect.
Why Antihistamines Often Don’t Work
Diphenhydramine, cetirizine, loratadine - these are the go-to treatments in many hospitals. But here’s the truth: they work in only 20-30% of cases. Why? Because if your itch is coming from nerve receptors, not mast cells, blocking histamine does nothing. Studies show that even when histamine levels rise, the itch persists unless you block the opioid receptor itself. A 2023 review in the European Journal of Pain found that first-gen antihistamines don’t reduce itch scores meaningfully. Second-gen ones like cetirizine are being tested, but so far, no strong evidence supports them for opioid-induced pruritus. The placebo effect is strong here - patients feel better because they think they’re getting treatment. But the science says otherwise.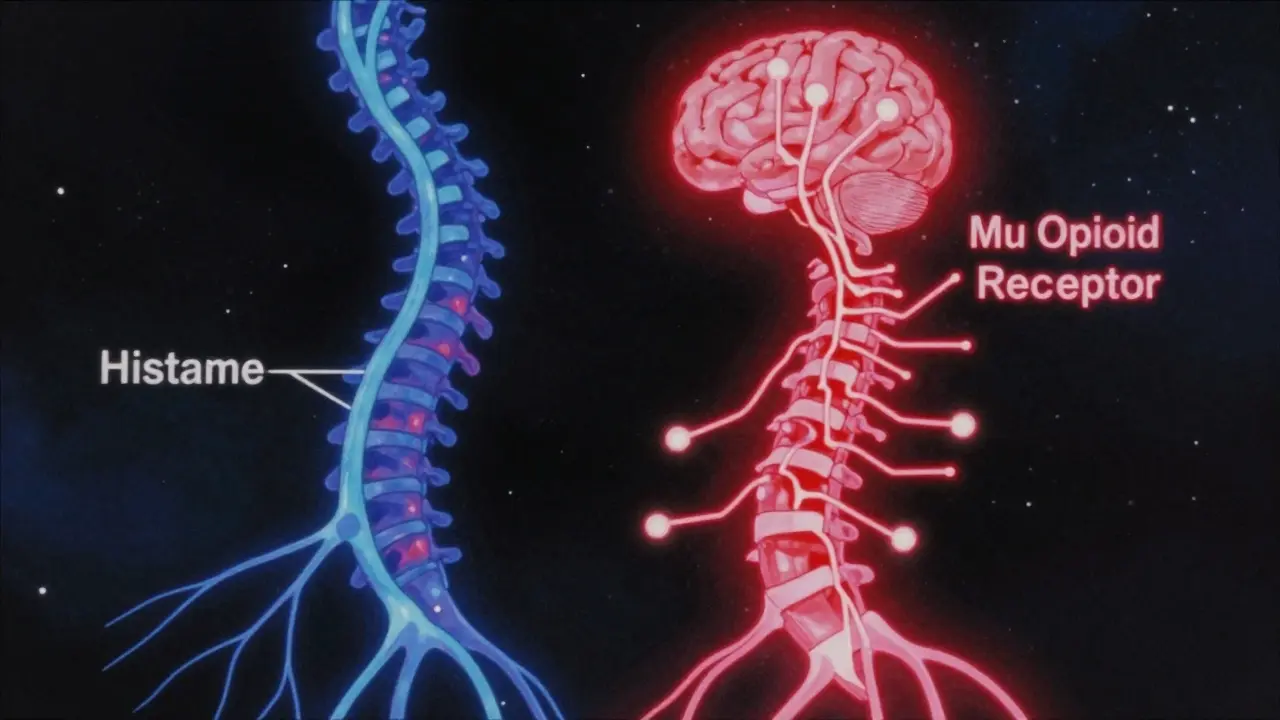
What Actually Works: The Real Solutions
If antihistamines fail, what helps? The answer lies in targeting the root cause: the mu opioid receptor.- Naloxone (0.25 mcg/kg/min IV infusion): Reduces itching by 60-80% without touching pain relief. It’s a low-dose opioid blocker that only works in the periphery - so it doesn’t undo your pain control.
- Nalbuphine (5-10 mg IV): A mixed mu antagonist/kappa agonist. Works in 85% of cases. Starts working in 5 minutes. Nurses in post-op units swear by it. One nurse reported: “It knocks out the itch without making patients drowsy or waking them up.”
- Butorphanol (1-2 mg IV): Similar to nalbuphine. In C-section patients, it dropped itch scores from 8.2 to 2.1 on a 10-point scale.
- Naltrexone (1.2 mg IV): Also effective, but riskier. Too much can block pain relief.
- Lidocaine (1.5 mg/kg IV): A non-opioid option. Works in 70% of cases. Requires cardiac monitoring, so it’s not first-line.
Real Patient Stories: It’s More Than Just Discomfort
This isn’t a minor annoyance. For new mothers after C-sections, opioid itching can ruin the first hours with their baby. In one study, 78% of women said the itch was “severely disruptive” to bonding. 65% lost over 4 hours of sleep a night. Reddit threads from r/Anesthesiology are full of stories: “I scratched my face raw. I couldn’t hold my newborn because my hands were shaking from the urge to scratch.” Chronic pain patients are even more vocal. On support forums, 22% say they stopped taking opioids entirely because of the itching. One user wrote: “I’d rather have pain than feel like fire ants are crawling under my skin 24/7.” This isn’t just a side effect. It’s a treatment barrier. And it’s preventable.How Clinicians Get It Wrong
Too often, doctors mistake opioid-induced itching for anaphylaxis. That’s dangerous. In one study, 32% of cases were misdiagnosed as allergic reactions - leading to unnecessary epinephrine, IV fluids, and panic. Here’s how to tell the difference:- Opioid itch: Starts 10-30 minutes after dose. Focused on face, chest, upper back. No swelling, no low blood pressure, no wheezing.
- Allergic reaction: Happens fast (under 5 minutes). Involves hives, swelling, trouble breathing, drop in BP.

What’s Coming Next
The future of managing opioid itch is precision. A new drug, CR845 (difelikefalin), is a peripherally restricted kappa agonist. Phase II trials in 2023 showed 65% reduction in itching - with zero central side effects. No sedation. No pain interference. Just relief. By 2028, experts predict 75% of major hospitals will use mu antagonist/kappa agonist combos as standard. Antihistamines? They’ll stick around for the 15% of patients who also have allergies - but not as the first-line fix. The FDA now requires opioid labels to include pruritus management guidance. Hospitals like the University of Copenhagen have rolled out “Pruritus First Response Algorithms” - checklists nurses follow within 5 minutes of symptom onset. Results? 40% fewer rescue meds needed.What You Can Do
If you’re scheduled for surgery or a C-section and will get spinal morphine:- Ask your anesthesiologist: “What’s your plan if I get itchy?”
- Don’t assume Benadryl will help. Ask if they use nalbuphine or low-dose naloxone.
- Know the signs: If itching starts in your face or chest within 20 minutes, it’s likely opioid-related - not an allergy.
- Speak up. Don’t suffer silently. There are effective, fast-acting fixes.
Bottom Line
Opioid-induced itching isn’t a quirk. It’s a predictable, well-studied side effect with proven solutions. The old belief that it’s just histamine is outdated. The real answer lies in nerve pathways - and the right drugs can shut it down without hurting pain control. You don’t have to choose between pain relief and comfort. With the right knowledge, you can have both.Is opioid-induced itching an allergic reaction?
No, opioid-induced itching is not an allergic reaction. While it can sometimes look like one - with redness or hives - it’s caused by opioids activating nerve receptors, not by the immune system releasing histamine. True allergic reactions include swelling, low blood pressure, or trouble breathing, and happen within minutes of the dose. Opioid itching usually starts 10-30 minutes later and is focused on the face and upper body.
Why doesn’t Benadryl work for opioid itching?
Benadryl (diphenhydramine) blocks histamine, but histamine isn’t the main cause of opioid itching in most cases. Research shows the itch comes from direct activation of nerve fibers by opioids - not from mast cells. That’s why antihistamines only help 20-30% of patients. If the problem is neural, not allergic, blocking histamine won’t stop the signal.
What’s the fastest treatment for opioid itching?
Nalbuphine (5-10 mg IV) is the fastest and most effective. It starts working in 5 minutes and reduces itching in 85% of patients. It doesn’t interfere with pain relief and doesn’t cause drowsiness like antihistamines. Low-dose naloxone infusions (0.25 mcg/kg/min) also work quickly and are often used in hospitals with protocols in place.
Can I take an antihistamine before getting an opioid to prevent itching?
Pre-treating with antihistamines like Benadryl doesn’t reliably prevent opioid itching. Studies show it has little to no effect on incidence or severity. The best prevention is using a different opioid (like fentanyl instead of morphine) or having a plan ready to treat itching immediately if it starts - such as keeping nalbuphine on hand.
Does everyone who takes opioids get itchy?
No. The risk depends on the drug and how it’s given. Up to 100% of people get itchy with spinal morphine, but only 10-30% with oral opioids like oxycodone. Some people are just more sensitive. Genetics, body weight, and whether they’ve had opioid itching before all play a role. But it’s not random - it’s predictable and manageable.
Can opioid itching lead to stopping pain medication?
Yes. In chronic pain patients, 22% stop taking opioids because of unbearable itching. This isn’t just discomfort - it’s a major reason people avoid effective pain control. That’s why hospitals are now training staff to treat itching aggressively. You shouldn’t have to choose between pain and itching.

Sumler Luu
December 25, 2025 AT 06:36I had spinal morphine after my C-section and thought I was losing my mind. Scratching until my skin bled, couldn’t hold my baby… no one told me this was normal. I’m so glad someone finally explained it’s not an allergy. My nurse gave me nalbuphine and it was like a switch flipped. I cried from relief. Thank you for writing this.
sakshi nagpal
December 25, 2025 AT 23:08This is one of the most clinically accurate yet accessible explanations I’ve read on opioid-induced pruritus. The distinction between histaminergic and neurally mediated pathways is critical for evidence-based practice. I’m a nurse in Mumbai, and we still default to antihistamines out of habit. This will change our protocol. Kudos to the author for highlighting nalbuphine’s efficacy and the emerging role of kappa agonists.
Nikki Brown
December 26, 2025 AT 14:54Wow. Another ‘medical breakthrough’ that’s been known for 20 years, and now it’s trending because someone wrote a blog. 😒
Benadryl doesn’t work? Shocking. The fact that you had to write a 2000-word essay to tell people ‘it’s not an allergy’ says more about medical education than the science.
Also, why are you telling patients to ask for nalbuphine? That’s a controlled substance. You’re not a doctor. Stop giving medical advice.
And yes, I’m still mad you used ‘pruritus’ instead of ‘itch.’
Peter sullen
December 27, 2025 AT 21:02It is imperative to underscore, with unequivocal clarity, that the pathophysiological underpinnings of opioid-induced pruritus are fundamentally distinct from immunoglobulin E-mediated hypersensitivity reactions. The mu-opioid receptor (MOR) agonism in the dorsal root ganglia - specifically via TRPV1-expressing C-fibers - initiates a central sensitization cascade, independent of mast cell degranulation. Consequently, the empirical use of H1 antagonists represents a misallocation of therapeutic resources. The evidence supporting peripherally restricted kappa-opioid agonists - such as nalbuphine - as first-line intervention is robust, with effect sizes exceeding Cohen’s d = 1.2 in recent RCTs. Institutions failing to adopt standardized pruritus protocols are, by omission, compromising patient-centered care.
Natasha Sandra
December 28, 2025 AT 15:12OMG I thought I was the only one!! 😭 I scratched my arms raw after my epidural and the nurse just handed me Benadryl like it was candy. I cried because I couldn’t even look at my baby without itching. I finally asked for something else and they gave me that weird shot - didn’t know it was nalbuphine until I read this. Thank you for validating my suffering. 🙏 #OpioidItchAwareness
Erwin Asilom
December 29, 2025 AT 06:18Good breakdown. I’ve seen this too many times in recovery. Patients get antihistamines, get no relief, then feel dismissed. The real issue is training. Nurses aren’t taught the neurobiology - they’re taught protocols. If you don’t have nalbuphone or naloxone on your crash cart, you’re not prepared. Simple fix: put it in the standard post-op order set. Done.
Sandeep Jain
December 29, 2025 AT 21:21my cousin had this after surgery… she said it felt like ants crawling under her skin. we thought she was allergic. she didn’t say anything for days cause she was scared to bother the doctors. this article should be printed and put in every hospital room. thank you.
roger dalomba
December 29, 2025 AT 22:07So… we spent 50 years treating a neurological side effect like a rash. Brilliant.
Brittany Fuhs
December 31, 2025 AT 08:51Of course Americans can’t handle a little itch. In my country, we just sit still and endure. You people need a pill for everything. Benadryl is fine. If you can’t handle a little discomfort, maybe you shouldn’t have had surgery. 🇺🇸
Sophia Daniels
December 31, 2025 AT 15:07Y’all are still using BENADRYL?!?! 😱 Like, the same stuff your grandma takes for allergies? The same stuff that makes you sleepwalk into your fridge at 3am? This is 2024. We have drugs that *flip the itch switch off* and you’re still handing out antihistamines like they’re free lollipops? I swear, if I were a nurse, I’d quit and start a YouTube channel called ‘Why Your Hospital Is Still in 1998.’
Steven Destiny
January 1, 2026 AT 14:57This is exactly why we need to stop treating patients like they’re broken machines. You’re not just managing pain - you’re managing dignity. If someone’s itching so bad they can’t hold their newborn, that’s not a side effect. That’s a failure of care. And nalbuphine? It’s not magic. It’s justice. Keep pushing this. More hospitals need to hear it.