Primary Sclerosing Cholangitis, or PSC, isn’t something most people have heard of - until they’re diagnosed. It’s a rare, slow-burning disease that attacks the bile ducts inside and outside the liver. Over time, these ducts become scarred, narrowed, and blocked. Bile can’t flow properly. The liver gets damaged. And eventually, without a transplant, it can fail. There’s no cure. No magic pill. But understanding PSC - how it works, what it does to your body, and how to manage it - can make a huge difference in how you live with it.
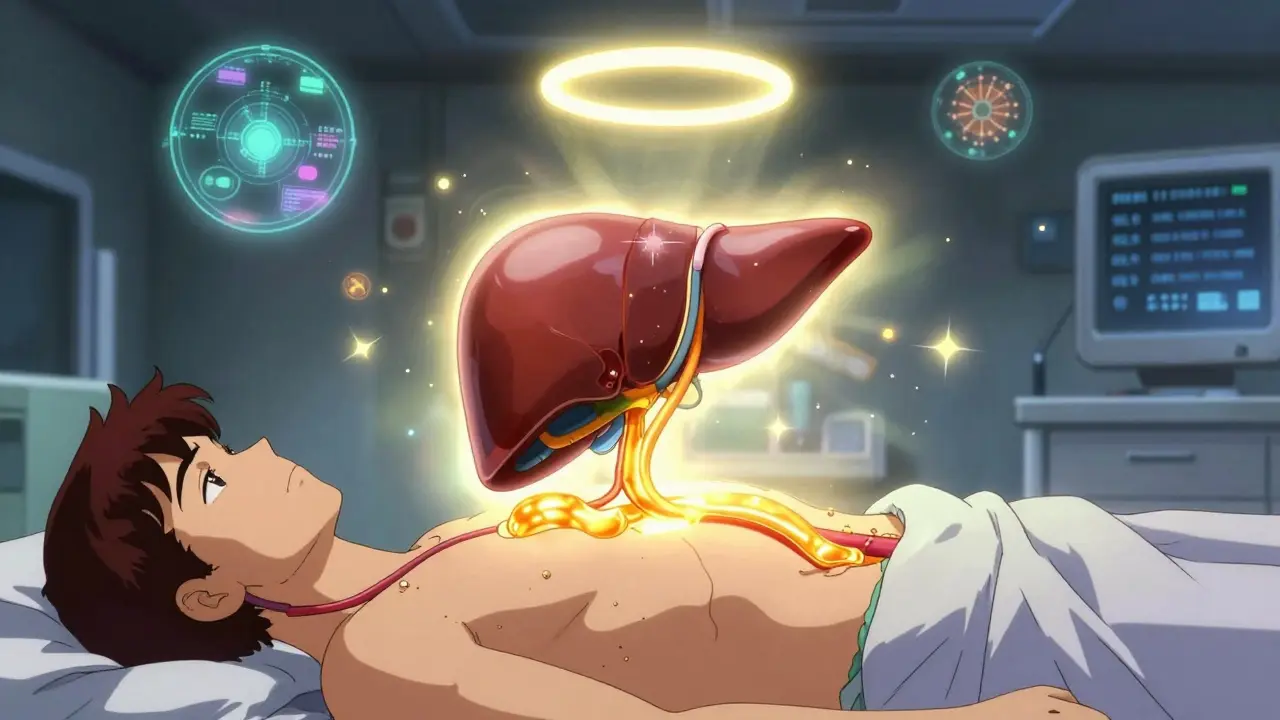
What Exactly Happens in Your Liver With PSC?
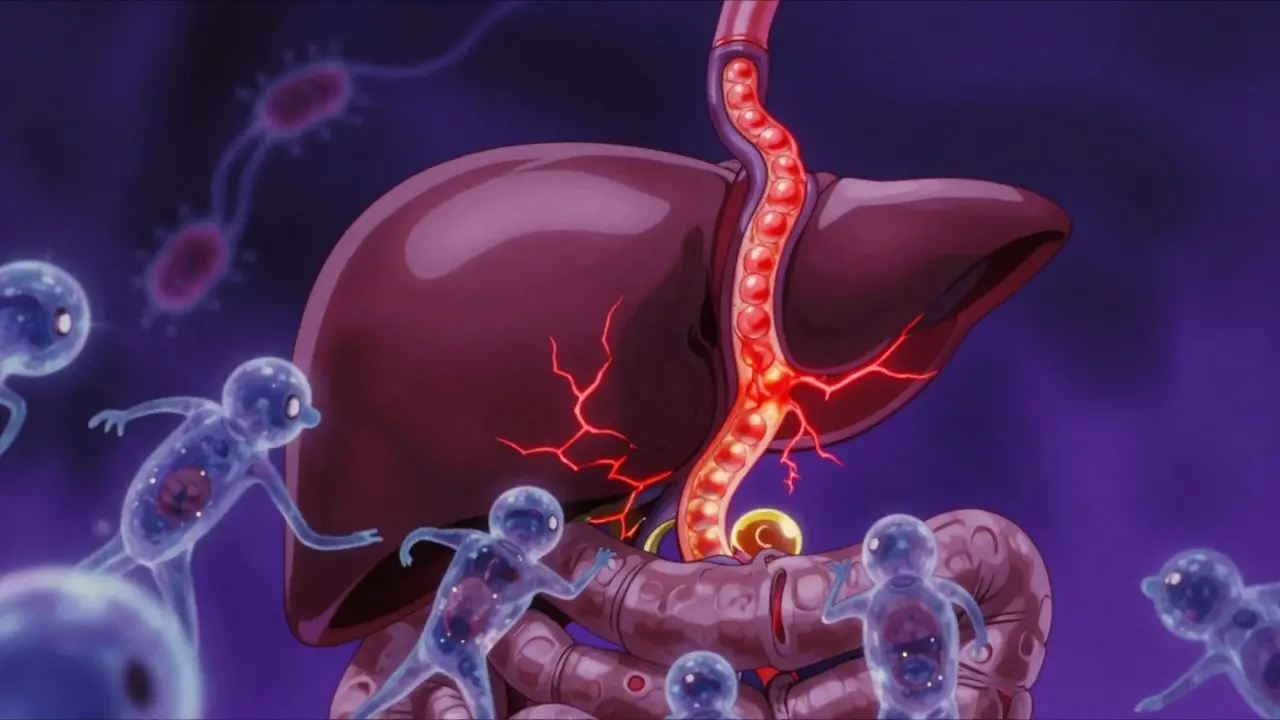
Your liver makes bile, a fluid that helps digest fats. Bile travels through tiny tubes called bile ducts to your small intestine. In PSC, your immune system mistakenly attacks those ducts. It’s not clear why, but genetics and gut bacteria seem to play a big role. The result? Chronic inflammation. Fibrosis. Scarring. The ducts get thinner, tighter, and eventually clogged.
On an MRCP scan - a special MRI of the bile ducts - you’ll see what doctors call a "beaded" pattern. That’s not a typo. It looks like a string of uneven beads because some parts of the duct are narrowed, others are normal. Normal bile ducts are 3 to 8 millimeters wide. In PSC, strictures often shrink to under 1.5 millimeters. That’s like trying to push water through a straw that’s been crushed halfway.
This isn’t a quick process. It takes 12 to 15 years on average for PSC to progress from early inflammation to cirrhosis. But symptoms can show up much earlier - or not at all. That’s why many people are diagnosed accidentally, during tests for something else.
Who Gets PSC - And Why?
PSC mostly hits men between 30 and 50. The ratio is about two men for every one woman. It’s rare globally - about 1 in 100,000 people - but more common in Northern Europe. In Sweden, it’s 6.3 per 100,000. Most cases are in people of European descent. But it’s being found more often in Asian populations, often in a milder form called small-duct PSC.
Genetics matter. If you have the HLA-B*08:01 gene variant, your risk jumps. Odds ratio? 2.15. That’s not a small bump. And almost 80% of people with PSC also have inflammatory bowel disease - mostly ulcerative colitis. The gut and liver are connected. When the gut lining is inflamed, bacteria and toxins leak into the bloodstream and reach the liver. That’s the "gut-liver axis" - and it’s central to how PSC develops.
Unlike Primary Biliary Cholangitis (PBC), which targets small bile ducts and shows up with a clear antibody (AMA), PSC is messier. Only 20 to 50% of patients test positive for p-ANCA. There’s no single blood test to confirm it. Diagnosis relies on imaging and ruling out other causes.
Symptoms Are Silent - Until They’re Not
Many people with PSC feel fine for years. No pain. No jaundice. No symptoms at all. That’s why it’s often found by accident - maybe during a routine blood test showing high liver enzymes.
When symptoms do appear, they’re frustrating and often misunderstood:
- Extreme itching (pruritus): This isn’t just dry skin. People describe it as if the itch comes from inside their bones. It gets worse at night and can make sleep impossible.
- Chronic fatigue: Not just tired. Exhausted. Even after a full night’s rest. One survey found 92% of patients report this as their worst symptom.
- Abdominal discomfort: Dull pain or pressure in the upper right side, where the liver sits.
- Jaundice: Yellowing of skin and eyes - a sign bile is backing up.
- Cholangitis: A dangerous infection of the bile ducts. Fever over 38.5°C, chills, and sharp pain mean you need antibiotics - and fast.
On average, people wait 2 to 5 years to get a diagnosis. That delay isn’t because doctors are careless. It’s because PSC is rare, symptoms are vague, and tests aren’t always obvious. Many end up seeing multiple specialists before someone connects the dots.

There’s No Drug That Cures PSC - And That’s the Hard Truth
For decades, doctors prescribed ursodeoxycholic acid (UDCA) - a bile acid - hoping it would help. It lowered liver enzymes. It looked promising. But large studies showed it didn’t improve survival. Worse, high doses (28-30 mg/kg/day) might actually increase risk of complications. The European Association for the Study of the Liver (EASL) now says: Don’t use UDCA routinely.
There are no FDA-approved drugs to stop PSC progression. That’s why so many patients feel hopeless. A 2023 survey found 74% of people feel frustrated because "doctors have nothing to offer."
But that doesn’t mean nothing can be done. Treatment is about managing symptoms and preventing complications.
How to Manage Symptoms - Even When There’s No Cure
Pruritus is the toughest symptom to control. First-line options include:
- Rifampicin: An antibiotic that helps 50-60% of patients. Dose: 150-300 mg daily.
- Naltrexone: A low-dose opioid blocker (50 mg daily) that helps when itching is tied to bile acids triggering brain receptors.
- Colesevelam: A bile acid binder (1.89-3.78 g daily) that traps bile in the gut so it’s excreted instead of recycled.
For fatigue? There’s no magic fix. But good sleep hygiene, light exercise, and ruling out vitamin deficiencies help. Many patients with PSC are low in fat-soluble vitamins - A, D, E, K - because bile isn’t moving properly to absorb them. Quarterly blood tests are essential. Supplementation isn’t optional. It’s part of survival.
Because PSC is linked to ulcerative colitis, colon cancer risk is high - 10-15% over a lifetime. Colonoscopies every 1-2 years are mandatory. Surveillance isn’t optional. It’s life-saving.
When the Liver Fails - Transplant Is the Only Option
Eventually, for many, the liver stops working. Cirrhosis sets in. Fluid builds up. Bleeding risks rise. That’s when liver transplant becomes the only real solution.
It’s not a cure for PSC - the disease can come back in the new liver, though it’s rare. But transplant gives you a new life. Five-year survival after transplant? Over 80%. That’s better than many cancers.
But transplants are limited. You need to be healthy enough to survive surgery. You need to be on a list. And you need to wait. The median time from diagnosis to transplant is about 10 years. That’s why research is so urgent.
What’s Coming Next? Hope on the Horizon
There are now over a dozen drugs in clinical trials targeting PSC. The most promising ones work on the FXR and PPAR pathways - systems that regulate bile flow and inflammation.
- Obeticholic acid (OCA): Showed 32% drop in liver enzymes in Phase 3 trials. But the FDA paused approval due to safety concerns.
- Cilofexor: A non-steroidal FXR agonist. European regulators gave it orphan drug status after Phase 2 showed 41% reduction in ALP levels.
- NorUDCA: A modified bile acid. Early results suggest it may reduce bile duct damage without the risks of regular UDCA.
The PSC Partners Seeking a Cure registry has over 3,100 patients across 12 countries. Real-world data from this group is helping researchers design better trials faster.
Dr. Andrew Manns from Hannover Medical School predicts: "Within five years, we’ll have at least two disease-modifying therapies." That’s not hype. That’s based on the pipeline.
Living With PSC - The Daily Reality
Living with PSC means constant vigilance. Quarterly blood tests. Annual MRCP scans. Vitamin checks. Colonoscopies. Medications that don’t always work. Fatigue that doesn’t go away. It’s exhausting - physically and emotionally.
But patients who get care at specialized PSC centers report far better outcomes. One 2022 survey found 85% of patients at designated centers had better symptom control than those treated in general hepatology clinics. Access to these centers isn’t equal. In rural Europe, only 35% of patients live within 100 miles of one. In the U.S., it’s 72%.
Support groups matter. Reddit’s r/liverdisease and HealthUnlocked’s PSC community are lifelines. People share what works - and what doesn’t. One user wrote: "The itching is unbearable - it’s not just skin deep but feels like it’s coming from my bones." That’s the kind of truth you won’t find in a textbook.
Understanding PSC isn’t about memorizing facts. It’s about knowing your body, asking the right questions, and finding a team that listens. You’re not just a patient. You’re someone fighting a slow disease - and you’re not alone.
What to Do If You’ve Just Been Diagnosed
- Find a hepatologist who specializes in PSC. General liver doctors often don’t have the experience.
- Get a baseline MRCP and liver function panel. Repeat annually.
- Test for vitamin A, D, E, K - and start supplements if needed.
- Get a colonoscopy if you have IBD - and schedule follow-ups every 1-2 years.
- Join a patient registry like PSC Partners. Your data helps future patients.
- Track your symptoms. Fatigue? Itching? Pain? Keep a log. It helps your doctor adjust care.
- Don’t ignore mental health. Anxiety and depression are common. Therapy isn’t a luxury - it’s part of treatment.
PSC is not a death sentence. It’s a challenge. But with the right care, people live full, meaningful lives - even while waiting for the next breakthrough.

Brooks Beveridge
December 17, 2025 AT 10:49Man, this post hit different. I’ve been living with PSC for 7 years now, and the fatigue? It’s not just being tired-it’s like your bones are made of wet cement and someone forgot to turn off the gravity.
But you’re right-there’s hope. I started taking low-dose naltrexone last year, and the itching? Cut it in half. Not magic, but enough to sleep through the night. Keep going, everyone.
And hey-if you’re reading this and feeling alone? You’re not. We’re out here.
Anu radha
December 17, 2025 AT 12:32I am so sorry you all go through this. My brother has it. He don’t talk much about it. But I see him tired all the time. I wish doctors had better medicine. I pray for you.
Josh Potter
December 18, 2025 AT 04:40Bro, I read this whole thing on my lunch break and now I’m crying in the parking lot. Not because I have it-thank god-but because I know someone who does. And I never realized how much they were hiding.
Just wanna say: you’re not a burden. You’re a goddamn warrior. And if you’re reading this and you’re tired? Take a nap. You’ve earned it.
Nishant Desae
December 19, 2025 AT 17:51As someone who’s been following PSC research since 2018, I’ve seen the slow crawl of progress-and honestly, it’s heartbreaking. But the fact that we now have over a dozen drugs in trials? That’s a miracle compared to 10 years ago.
And let’s not forget the patient registries-PSC Partners, the one mentioned here-those are the real heroes. They’re not just collecting data; they’re building a community that doctors finally listen to.
One thing I wish more people knew: small-duct PSC isn’t ‘mild.’ It’s just slower. And it still carries the same cancer risk. Don’t let anyone tell you otherwise.
Also, vitamin D isn’t optional. If your levels are below 50 ng/mL, you’re playing Russian roulette with your bones and your immune system. Get tested. Supplement. Do it now.
And for those feeling hopeless? I get it. I’ve been there. But the tide is turning. I’ve seen patients go from transplant lists to hiking trails in under two years. It’s not fast-but it’s happening.
Jane Wei
December 20, 2025 AT 02:22My mom was diagnosed last year. She’s 62. She’s still gardening. Still makes her famous apple pie. She says, ‘If I can’t cure it, I’ll outlive it.’
She’s right. This disease doesn’t get to write the ending.
Steven Lavoie
December 20, 2025 AT 09:48One thing missing from this post is the global inequity in care. In the U.S., 72% of patients are near a specialized center. In India, it’s less than 5%.
And yet, the same genetic markers, the same gut-liver axis, the same beaded ducts-they’re universal.
We need global research funding, not just Western trials. PSC doesn’t care about borders. Why do our solutions?
Philippa Skiadopoulou
December 22, 2025 AT 07:02Corrected reference: The EASL 2023 guidelines explicitly advise against UDCA doses exceeding 15–20 mg/kg/day, not routine use altogether. High-dose UDCA remains contraindicated, but low-dose may still be considered in select cases pending further evidence.
Additionally, the 85% symptom control statistic cited refers to tertiary care centers with multidisciplinary teams, not merely ‘designated centers.’ Precision matters.
Victoria Rogers
December 22, 2025 AT 14:22Okay but let’s be real-how many of these ‘breakthrough’ drugs are just Big Pharma repackaging old junk? Obeticholic acid got paused because it made people itch MORE. And now they’re calling it ‘promising’? Please.
And don’t even get me started on ‘support groups.’ Reddit isn’t a clinical trial. I’ve seen people stop their meds because some guy in Ohio said ‘turmeric helped him.’
Stop romanticizing suffering. We need real science, not feel-good stories.
Evelyn Vélez Mejía
December 22, 2025 AT 16:00There is a quiet, unspoken grief in chronic illness that no one talks about-the grief for the body you thought you’d inherit. The one that didn’t betray you. The one that didn’t turn your own immune system into a traitor.
And yet-we persist. We track our vitals. We schedule our colonoscopies. We swallow pills that do nothing but make us nauseous. We show up. Not because we’re brave. But because we have no other choice.
That is not weakness. That is the most profound form of courage I’ve ever witnessed.
And to the doctors reading this: stop calling it ‘manageable.’ It’s not. It’s a marathon with no finish line. But we run anyway.
So thank you. To every one of you. You are not a statistic. You are a story. And your story still matters.
Kent Peterson
December 24, 2025 AT 13:55Wow. Another ‘PSC awareness’ post from the woke medical industrial complex. Let me guess-next they’ll say ‘liver transplants are a human right’ and ‘vitamin D is a form of resistance’?
Real talk: If you’re waiting for a cure, you’re wasting time. The system doesn’t care. Pharma doesn’t care. Your ‘community’ doesn’t care. They just want your data, your story, your pain points.
And don’t get me started on ‘gut-liver axis’-it’s just a fancy way of saying ‘we don’t know what’s going on.’
Here’s the truth: You’re gonna die. The sooner you accept that, the sooner you stop letting them monetize your suffering.