Managing COPD isn’t just about breathing better-it’s about keeping your finances from spiraling. If you’re taking roflumilast, you already know it’s not a cheap pill. But what most people don’t talk about is how the cost adds up over time, and how that impacts everything from your monthly budget to your long-term security. This isn’t about scare tactics. It’s about real numbers, real strategies, and real ways to make sure your treatment doesn’t cost you your future.
What roflumilast actually costs
Roflumilast, sold under the brand name Daxas or Daliresp, isn’t a generic drug. In the U.S., a 30-day supply without insurance typically runs between $600 and $900. That’s not a typo. For many people on fixed incomes or without robust coverage, that’s more than their monthly rent or utility bill. Even with Medicare Part D, you might still pay $150-$300 per month depending on your plan’s coverage stage. If you’re taking it daily for years-as most COPD patients do-that’s $1,800 to $3,600 a year, just for this one pill.
Compare that to other COPD medications. Inhalers like Advair or Symbicort might cost $300-$500 a month, but they’re often covered under Tier 2 or 3 with lower copays. Roflumilast? It’s usually Tier 4-specialty tier. That means higher out-of-pocket costs, and often, prior authorization hassles. You’re not just paying for the drug. You’re paying for the paperwork, the appeals, the delays.
Why roflumilast is worth the price-if you qualify
It’s easy to look at the sticker price and feel overwhelmed. But roflumilast isn’t just another COPD med. It’s one of the few oral drugs proven to reduce flare-ups in people with severe COPD linked to chronic bronchitis. A 2023 study in the European Respiratory Journal showed patients on roflumilast had 20% fewer hospital visits over 12 months compared to placebo. Fewer hospital stays mean fewer ambulance rides, ER copays, and lost wages from missed work.
Think of it this way: one ER visit for a COPD exacerbation can cost $8,000-$15,000. Even with insurance, your portion could be $1,000-$3,000. If roflumilast cuts your flare-ups by even half, you’re saving thousands. That’s not just medical-it’s financial.
How to cut the cost without cutting the treatment
You don’t have to choose between breathing and paying bills. Here’s how real people are managing it:
- Ask for manufacturer assistance. AstraZeneca, the maker of roflumilast, offers a patient assistance program called MyAstraZeneca Support. If your income is under $50,000 a year (or $68,000 for a family of four), you may get the drug for free. You don’t need to be uninsured-many with Medicare Part D still qualify.
- Use mail-order pharmacies. Most insurance plans charge less for a 90-day supply than three 30-day fills. You’ll pay one copay instead of three. Some pharmacies even offer free shipping and automatic refills.
- Check state pharmaceutical assistance programs. Many states have programs that help with specialty drug costs. For example, California’s Rx Assist and New York’s EPAP offer direct subsidies. Search your state’s health department website for “pharmaceutical assistance” + your state name.
- Compare prices across pharmacies. Roflumilast prices vary wildly. A CVS might charge $750, while a Walmart or Costco might list it at $480 with a GoodRx coupon. Always check GoodRx, SingleCare, or Blink Health before you pay.
What your insurance doesn’t tell you
Insurance companies don’t always make it easy. Roflumilast often requires prior authorization. That means your doctor has to submit proof you’ve tried other treatments first-like long-acting bronchodilators or inhaled steroids. If they skip this step, your claim gets denied. And if you’re not tracking it, you might get stuck with a $900 bill.
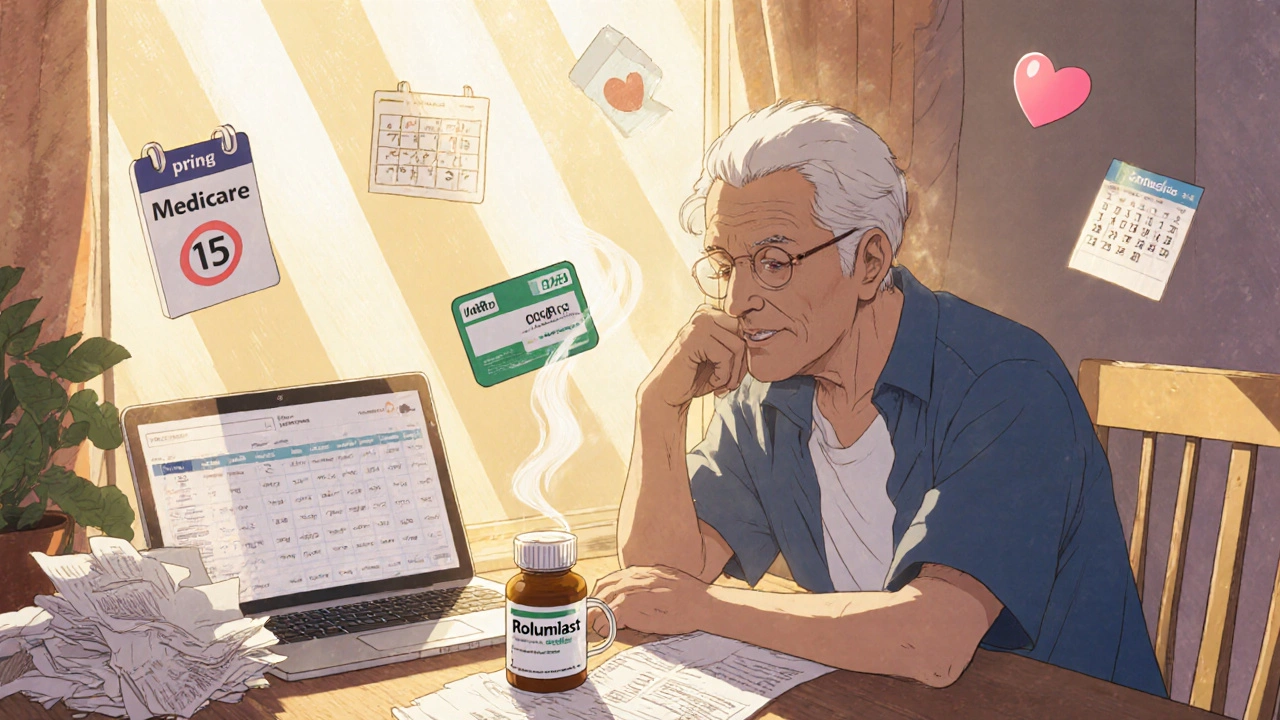
Here’s what to do: Ask your doctor’s office to submit the prior auth request before you fill your first prescription. Then, call your insurer directly and ask for a written confirmation of approval. Keep a copy. If they deny it, you have 60 days to appeal. Don’t wait. Delays mean missed doses, and missed doses mean more flare-ups.
Also, watch for formulary changes. Insurers change which drugs they cover every year. Just because roflumilast was covered last year doesn’t mean it will be this year. Call your plan every January-don’t wait for your refill to be denied.
Long-term planning: COPD and retirement
If you’re 55 or older, you’re probably thinking about retirement. But COPD changes the math. Medication costs don’t stop when you retire-they often increase. Medicare doesn’t cap out-of-pocket drug spending. That means once you hit the donut hole, you’re back to paying full price.
Plan ahead:
- Build a medication budget into your retirement plan. Assume $3,000 a year for roflumilast and other COPD meds.
- Consider a Health Savings Account (HSA) if you’re still working and have a high-deductible plan. Contributions are tax-free, grow tax-free, and can be used for COPD meds later.
- Look into Medicare Supplement (Medigap) plans. They don’t cover drugs directly, but they reduce hospital and ER costs-which matter more when you’re on roflumilast.
And don’t ignore your mental health. The stress of managing chronic illness and high drug costs is linked to depression and anxiety. Talk to your doctor about counseling. Many Medicare plans cover mental health services at low or no cost.
When roflumilast isn’t right for you
Not everyone with COPD needs roflumilast. It’s only approved for severe COPD with chronic bronchitis and a history of flare-ups. If you’re on oxygen, have liver disease, or are underweight, your doctor might skip it. And if your flare-ups are rare, the cost may not make sense.
Ask your pulmonologist: “Based on my flare-up history, is roflumilast likely to prevent hospital visits for me?” If the answer is “maybe,” explore alternatives. Some patients do better with long-term azithromycin (a low-dose antibiotic), which can cost under $20 a month. Others benefit from pulmonary rehab-often covered by insurance and proven to reduce hospitalizations.
What to do next
Take action today:
- Call your pharmacy and ask for the cash price of roflumilast. Compare it to GoodRx.
- Visit MyAstraZeneca Support and check eligibility for free medication.
- Call your insurance provider and ask: “Is roflumilast on my formulary? What’s my copay? Is prior auth required?”
- Set a calendar reminder for January 15 to review your drug coverage again next year.
You’re not just managing a disease. You’re managing your life. And that includes your money. Roflumilast can help you breathe easier-but only if you plan for the cost. Don’t wait for a bill to arrive before you act. Start now. Your lungs-and your bank account-will thank you.
Is roflumilast covered by Medicare?
Yes, roflumilast is covered by most Medicare Part D plans, but it’s usually in the highest cost tier (Tier 4). You’ll likely pay a higher copay-often $150-$300 per month-unless you qualify for extra help or a manufacturer’s discount. Always check your plan’s formulary each year, as coverage can change.
Can I get roflumilast for free?
Yes. AstraZeneca’s patient assistance program provides roflumilast at no cost to eligible U.S. residents with incomes under $50,000 (individual) or $68,000 (family of four). You don’t need to be uninsured. Many people with Medicare Part D still qualify. Apply online at MyAstraZeneca Support.
Are there cheaper alternatives to roflumilast?
For some patients, yes. Low-dose azithromycin (taken 3 times a week) has been shown to reduce COPD flare-ups and costs under $20/month. Pulmonary rehabilitation programs-often covered by insurance-also lower hospitalization rates. But these aren’t direct substitutes. Talk to your doctor about whether your flare-up pattern makes you a candidate for alternatives.
Why does roflumilast cost so much?
Roflumilast is a specialty drug with limited competition. It’s not a generic, and it’s only approved for a specific subset of COPD patients-chronic bronchitis with frequent flare-ups. Because the market is small, manufacturers set higher prices. Unlike inhalers, which have many brands and generics, roflumilast has no close competitors, so pricing power stays with the maker.
What happens if I skip doses to save money?
Skipping doses increases your risk of severe COPD flare-ups, which can lead to emergency room visits, hospital stays, and even long-term lung damage. One ER visit can cost 10 times more than a year’s supply of roflumilast. It’s not a savings strategy-it’s a financial trap. If you can’t afford it, use patient assistance programs instead.

Ankit Yadav
November 6, 2025 AT 02:19Been on roflumilast for 3 years now. My rent is $800, this pill is $700. I chose breathing over a new couch. No regrets. My doctor helped me get it free through AstraZeneca. If you’re struggling, just ask. No shame.
Meghan Rose
November 7, 2025 AT 20:10Okay but like… why is this even a thing? Why can’t we just make it cheaper? Like, it’s not like it’s rocket science. I mean, I’ve seen ads for Viagra and that’s like $5 a pill. This is literally just a chemical in a capsule. Someone’s making bank and we’re paying for it. 🤷♀️
Steve Phillips
November 8, 2025 AT 04:29Oh, so now we’re romanticizing the $900/month pill like it’s some noble sacrifice? Let’s be real - this is pharmaceutical capitalism at its most grotesque. AstraZeneca didn’t invent oxygen. They bought a patent, slapped a brand name on it, and turned a chronic disease into a luxury subscription. And now we’re supposed to be grateful for their ‘patient assistance’ program? Please. It’s a PR stunt with a form you have to fill out three times. I’ve seen people die waiting for approval.
And don’t even get me started on ‘GoodRx’ - it’s just a middleman profiting off your desperation. The real solution? Single-payer. Nationalize the damn drugs. But no, we’d rather have you crying in the pharmacy aisle while you pick between insulin and your kid’s college fund.
Rachel Puno
November 9, 2025 AT 20:07Hey - I’m right there with you. I’ve been there. The fear when the prescription says ‘prior auth pending’? It’s worse than the coughing fits. But you’re not alone. I got mine for $12 a month through my state’s program. Just call your local Area Agency on Aging. They’ll walk you through it. You’ve got this. 💪
Clyde Verdin Jr
November 10, 2025 AT 17:26So… you’re telling me I have to CHOOSE between breathing and not going broke? 😭 I thought COPD was bad enough without having to sell my soul to a corporation to stay alive. This isn’t medicine - it’s a hostage situation. And the hostage-taker has a PhD and a corporate jet. #RoflumilastTax
Key Davis
November 12, 2025 AT 11:03While the financial burden of specialty medications is undeniably significant, I would respectfully suggest that the broader systemic issue lies in the fragmentation of healthcare financing and the absence of universal drug price regulation. The current model incentivizes pharmaceutical innovation at the expense of equitable access. A coordinated policy response - including value-based pricing and international reference pricing - would be more sustainable than individualized patient advocacy.
Cris Ceceris
November 14, 2025 AT 05:12I keep thinking about how weird it is that we treat medicine like a product you buy at a store. Like, if you need a new kidney, you don’t get to pick the brand. But if you need to breathe? You’re stuck comparing CVS vs Walmart prices like it’s a Black Friday sale. It’s not about being ‘smart’ with your money - it’s about being alive. And we’ve made being alive into a negotiation.
Brad Seymour
November 14, 2025 AT 23:54Love this thread. Real talk. I’m from the UK and we get this stuff free through the NHS - no stress, no forms, no GoodRx. Just walk in, get it. I know it’s not the same system, but it makes you wonder why we’re okay with this in the US. We’re the richest country on earth. We can do better.
Malia Blom
November 16, 2025 AT 07:54Okay but what if the real problem isn’t the drug - it’s that we’re all just too lazy to quit smoking? I mean, if you didn’t smoke, you wouldn’t need this pill. So why are we blaming Big Pharma when the root cause is personal choice? Just saying.
Erika Puhan
November 16, 2025 AT 11:34Let’s not romanticize this. Roflumilast is a PDE4 inhibitor - a second-line agent for a subset of patients with FEV1 <50% and chronic bronchitis. Most patients are overprescribed it. The real cost isn’t the pill - it’s the misallocation of healthcare resources due to guideline non-adherence. And yes, your ‘$300 copay’ is a symptom of a broken system - but the solution isn’t charity programs. It’s evidence-based prescribing.
Edward Weaver
November 17, 2025 AT 18:38Why are we even talking about this? In my country, we don’t let foreigners get free meds. If you can’t afford it, move to Canada. Or better yet - don’t get sick. That’s what I say. America’s not a福利国家. You want cheap drugs? Work harder. Pay taxes. Don’t be lazy.
Lexi Brinkley
November 18, 2025 AT 03:05OMG this hit so hard 😭 I cried reading it. I just got my first bill for $892. I had to sell my dog’s special food to pay for it. I miss her. I miss breathing. I miss not crying every time I see a pharmacy. 💔🙏 #RoflumilastStruggles
Kelsey Veg
November 19, 2025 AT 14:42so i got the pill for 480 at costco but then my doc said i need a blood test every month to stay on it. that’s like 150 a pop. so now im paying 630 a month. who even designed this system? 🤦♀️
Steve Phillips
November 21, 2025 AT 11:07And now we’re turning patients into financial engineers. ‘Oh, just apply for assistance, use mail-order, compare coupons.’ Meanwhile, the people who are too tired, too sick, too depressed to fill out forms - they’re the ones who end up in the ER. And guess what? That costs the system more. This isn’t empowerment. It’s exploitation dressed up as ‘resourcefulness’.