Spiritual Practice Impact Calculator
Enter your details and click "Assess Impact" to see how your spiritual practices may interact with your treatment.
Key Takeaways
- Spiritual practices can complement clinical treatment for schizophrenia, but they are not a substitute for medication.
- Evidence shows mindfulness, prayer, and faith‑based counseling can reduce stress and improve quality of life.
- Professional guidance is crucial to avoid false beliefs that could worsen psychotic symptoms.
- Integrating spirituality should respect personal beliefs and cultural background.
- Resources such as peer‑support groups and WHO guidelines help navigate the intersection of mental health and faith.
When someone hears the word Schizophrenia is a chronic brain disorder characterized by hallucinations, delusions, and disorganized thinking, the first thought is usually medication. Yet many people wonder if faith, prayer, or meditation could play a role in managing the condition. This article pulls together research, clinical insight, and real‑world stories to answer that question. You’ll learn how spiritual practices interact with symptoms, where the science stands, and practical steps for safely blending belief with treatment.
schizophrenia affects roughly 20 million people worldwide, according to the World Health Organization (WHO). While antipsychotic medication remains the cornerstone of care, a growing body of research highlights the benefits of addressing the whole person-including their spiritual dimension.
Understanding Schizophrenia and Its Core Challenges
To see how spirituality fits in, start with the basics. Schizophrenia typically emerges in early adulthood and involves three symptom clusters:
- Positive symptoms - hallucinations and delusions that add experiences.
- Negative symptoms - flat affect, social withdrawal, and reduced motivation.
- Cognitive symptoms - trouble with memory, attention, and executive function.
These symptoms can disrupt daily life, relationships, and self‑identity. The diagnostic criteria are set out in the DSM‑5 is the American Psychiatric Association’s standard manual for mental health diagnoses, which requires at least two of the above symptoms for a six‑month period.
Neurobiology research links schizophrenia to dopamine dysregulation, glutamate signaling, and structural brain changes. However, none of these findings explain why two people with similar clinical profiles can have vastly different life outcomes. That’s where personal meaning, social support, and spirituality step in.
What Does Spirituality Mean in a Mental‑Health Context?
Spirituality is a broad term that refers to a person's search for meaning, purpose, and connection beyond the material world. It can manifest as organized religion, personal meditation practice, or a sense of awe in nature. Importantly, spirituality is distinct from religiosity (formal affiliation), though the two often overlap.
In clinical settings, professionals use the term "spiritual well‑being" to capture how a person’s beliefs influence coping, hope, and resilience. For someone with schizophrenia, spirituality can provide:
- A framework for interpreting bizarre experiences (e.g., viewing a hallucination as a spiritual message).
- A source of community support via churches, mosques, or meditation groups.
- Mind‑body techniques that reduce stress hormones.
But spirituality can also backfire if delusional content becomes intertwined with religious ideas, a phenomenon known as "religious psychosis".
Evidence Linking Spiritual Practices to Better Outcomes
Researchers have examined several spiritual‑related interventions:
| Practice | Core Element | Evidence Strength | Typical Use |
|---|---|---|---|
| Mindfulness‑Based Cognitive Therapy | Non‑judgmental present‑moment awareness | Moderate (several RCTs) | Reduces negative symptoms, improves insight |
| Prayer or Faith‑Based Counseling | Structured religious dialogue | Low‑to‑moderate (observational studies) | Boosts hope, lowers perceived stigma |
| Yoga and Breath Work | Physical postures + controlled breathing | Emerging (pilot trials) | Alleviates anxiety, improves sleep |
| Spiritual Peer‑Support Groups | Shared experiences within a faith community | Low (qualitative reports) | Enhances social connection |
The World Health Organization is a United Nations agency that provides global health guidelines cites psychosocial interventions-including spiritual care-as adjuncts to medication in its Mental Health Action Plan 2024‑2030. A 2022 meta‑analysis of mindfulness‑based programs showed a 15% reduction in negative symptom scores compared with treatment‑as‑usual.
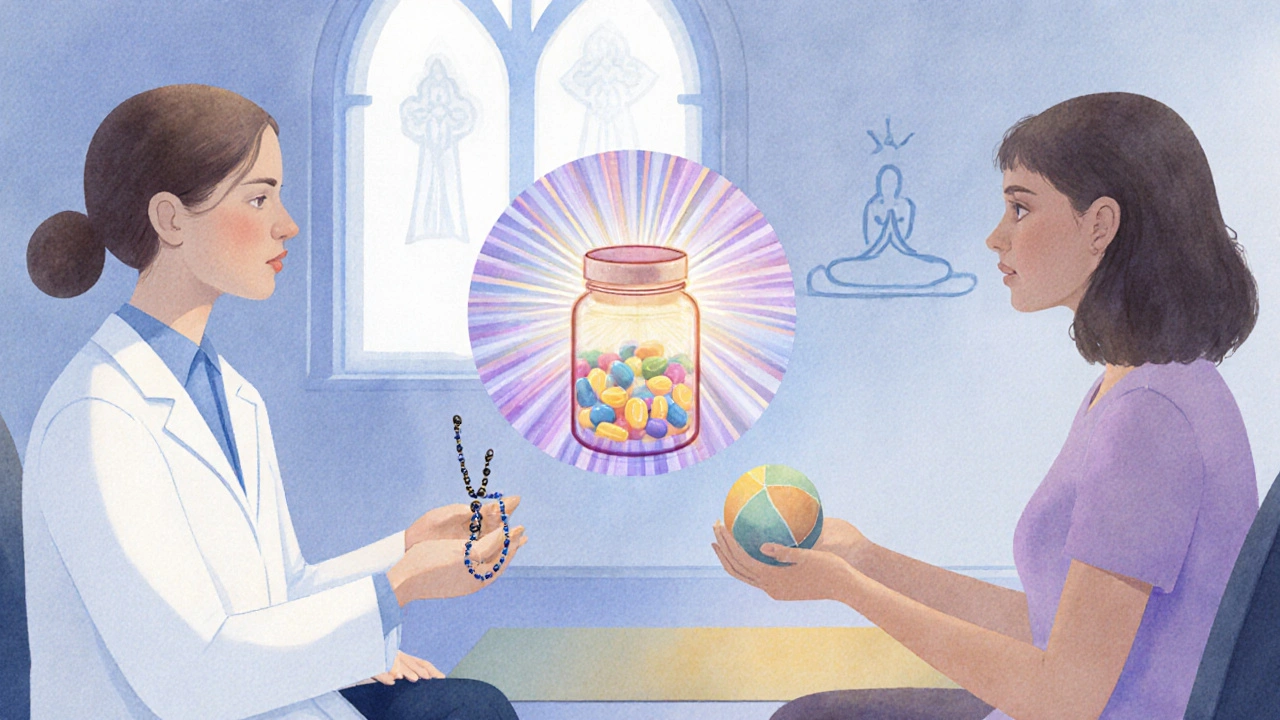
When Spirituality Helps-and When It Might Harm
Positive outcomes generally arise when the spiritual practice:
- Encourages grounding techniques (e.g., breath focus) that counteract agitation.
- Provides a supportive community that promotes medication adherence.
- Offers meaning that reduces internalized stigma.
Potential pitfalls include:
- Interpreting hallucinations as divine commands, leading to risky behavior.
- Rejecting medication in favor of “faith healing,” which can precipitate relapse.
- Excluding mental‑health professionals from the care team, creating a siloed approach.
Clinicians often use the Recovery Model is an approach that focuses on personal growth, hope, and functional improvement rather than symptom elimination to balance spiritual needs with medical safety. The model stresses collaborative planning, where patients, families, and providers discuss spiritual preferences openly.
Practical Steps to Integrate Spirituality Safely
If you or a loved one with schizophrenia wants to explore spirituality, consider these steps:
- Talk to the treatment team. Mention any religious or spiritual practices you value. A psychiatrist or therapist can help assess whether a practice might interfere with medication or exacerbate symptoms.
- Choose evidence‑backed techniques. Mindfulness, yoga, and guided meditation have the strongest research support. Start with short, structured sessions-5-10 minutes a day.
- Find a supportive community. Look for faith‑based groups that welcome mental‑health discussions. Many churches and mosques now have mental‑health ministries that collaborate with clinicians.
- Set clear boundaries. If a spiritual leader suggests stopping medication, seek a second opinion from a mental‑health professional.
- Track outcomes. Keep a simple log of mood, sleep, and symptom changes when you introduce a new practice. Share this with your clinician.
These steps help keep the spiritual journey constructive rather than destabilizing.
Real‑World Stories: How People Combine Faith and Treatment
John, a 28‑year‑old from Manchester, was diagnosed with schizophrenia at 22. He struggled with medication side effects and felt disconnected from his Anglican faith. After his therapist suggested mindfulness, John joined a church‑run meditation circle. Over six months, his anxiety dropped, and he reported feeling "more at peace" during psychotic episodes. He continued his antipsychotic regimen, noting that the spiritual practice made medication more tolerable.
Maria, a 35‑year‑old mother of two, relies on daily prayer and a supportive mosque community. She works with a psychiatrist who integrates her prayer schedule into treatment planning, ensuring she takes medication before early‑morning prayers. The routine reduces missed doses and provides a sense of purpose that counters depressive symptoms.
These narratives illustrate the spectrum: some people use spirituality as a coping tool alongside medication, while others may experience conflict that requires careful clinical navigation.
Resources for Patients, Families, and Clinicians
- WHO Mental Health Action Plan 2024‑2030 - outlines psychosocial care standards, including spiritual support.
- National Alliance on Mental Illness (NAMI) - offers peer‑support groups that respect diverse faith backgrounds.
- Mindfulness‑Based Cognitive Therapy (MBCT) manuals - practical guides for clinicians and patients.
- Faith‑Based Mental Health Directories - searchable listings of chaplains, counselors, and religious organizations trained in mental‑health collaboration.
Engaging with these resources can demystify the process and provide concrete tools for integrating spirituality safely.
Key Takeaways for Different Audiences
For patients: Spirituality can enhance coping and hope, but never replace prescribed medication without professional guidance.
For families: Respecting a loved one’s beliefs while encouraging open dialogue with clinicians fosters a supportive environment.
For clinicians: Inquire about spiritual preferences early, recommend evidence‑based practices, and coordinate care with faith leaders when appropriate.

Frequently Asked Questions
Can prayer cure schizophrenia?
Prayer alone cannot cure schizophrenia. The condition requires antipsychotic medication and psychosocial support. Prayer may add comfort and reduce stress, but it should complement-not replace-standard treatment.
Is mindfulness safe for someone experiencing hallucinations?
For most patients, mindfulness is safe and can improve insight. However, if a person finds guided meditation triggers vivid internal imagery, a therapist should adapt the practice-perhaps focusing on breath awareness rather than visualization.
What should I do if my therapist says my religious beliefs are worsening my symptoms?
Ask for clarification and request a collaborative plan. You might benefit from a chaplain‑clinician partnership that respects both medical and spiritual viewpoints.
Are there any medications that interfere with meditation or prayer?
Most antipsychotics do not directly affect meditation. Sedating medications can make staying alert during practice harder, so timing doses around meditation sessions can help.
How can families support a loved one’s spiritual journey?
Listen without judgment, attend faith‑based events if invited, and encourage open conversations with healthcare providers about spiritual preferences.


Victoria Unikel
October 4, 2025 AT 13:43i guess faith can be a nice add‑on but meds still the main thing.
Lindsey Crowe
October 13, 2025 AT 19:56oh great, because chanting cures dopamine imbalance.
Rama Hoetzlein
October 23, 2025 AT 02:10Look, the whole "spirituality heals all" narrative is a dangerous myth that pretends the mind is some mystical garden where prayers replace neurochemistry.
First, schizophrenia is a biologically rooted disorder; dopamine dysregulation doesn’t magically dissolve when you say a mantra.
Second, the literature shows only modest effect sizes for mindfulness‑based interventions and those are adjuncts, not replacements.
Third, when patients start believing their hallucinations are "divine messages," they risk reinforcing delusional systems.
Fourth, the clinical community has documented cases where faith‑based groups pressured patients to skip medication, leading to relapse.
Fifth, you cannot ignore the social determinants – poverty, stigma, isolation – that spirituality alone cannot resolve.
Sixth, you must ask: who profits from the spiritual‑only agenda? Charities, churches, and some alternative practitioners often receive donations from vulnerable patients.
Seventh, the WHO does endorse psychosocial care, but it explicitly states it must be integrated with pharmacotherapy.
Eighth, mindfulness can improve stress response, but only when guided by trained clinicians who monitor psychotic symptoms.
Ninth, yoga’s breath work may lower cortisol, yet many studies lack proper control groups and are underpowered.
Tenth, peer‑support groups that focus solely on faith can become echo chambers, magnifying false beliefs.
Eleventh, the ethical line is crossed when clinicians allow religious doctrine to dictate treatment plans.
Twelfth, any spiritual practice that triggers intense inner imagery can exacerbate hallucinations if not properly adapted.
Thirteenth, the patient’s autonomy must be respected, but not at the expense of evidence‑based care.
Fourteenth, collaboration with chaplains is valuable only when it supplements, not supplants, medication adherence.
Fifteenth, the bottom line: spirituality can be a supportive tool, but it is not a cure, and treating it as such is both naïve and dangerous 😊.
Lorena Garcia
November 1, 2025 AT 07:23i was wondering how someone could actually fit a weekly prayer group into a medication schedule without missing doses, any tips would be cool.
Dietra Jones
November 10, 2025 AT 13:36Just a quick note – the article typo’s “psychotic” as “pshychotic” a few times. Also, “medication adherence” should be hyphenated consistently.
Victoria Guldenstern
November 19, 2025 AT 19:50so you claim mindfulness is the silver bullet but ignore the half‑baked studies that lack proper blinding and control groups – classic cherry‑picking of data without any real nuance.
Bill Bolmeier
November 29, 2025 AT 02:03Hey folks, I’ve seen several patients thrive when they blend a daily 10‑minute breathing exercise with their meds – the stress drop is real and it often translates into better sleep.
It’s not magic, but the added routine creates a sense of agency that counters the helplessness many feel.
If you’re skeptical, try logging mood for a couple of weeks while you add a short meditation; the data usually speaks for itself.
Remember, support from family or a faith community can reinforce that habit and keep medication adherence on track.
Stay hopeful, keep experimenting safely, and always keep the psychiatrist in the loop.
Darius Reed
December 8, 2025 AT 08:16Imagine a world where the choir sings a lullaby while the neuro‑chemist adjusts the dose – that’s the kind of creative synergy we need, folks.
Karen Richardson
December 17, 2025 AT 14:30For clarity, the phrase should be "spiritual practices can complement clinical treatment," not "spiritual practice impact calculator" which reads oddly; also, "mindfulness‑based" requires a hyphen.
AnGeL Zamorano Orozco
December 26, 2025 AT 20:43Okay, let me dramatize this: picture a patient standing on the edge of a cliff of psychosis, clutching a rosary while the doctor hands over a pill bottle – the tension is palpable, the stakes are life‑or‑death, and yet you suggest a "nice little meditation" will save the day. It’s theatrical, it’s absurd, and it’s a disaster waiting to happen if we let mysticism replace medicine!
Cynthia Petersen
January 5, 2026 AT 02:56so you think sarcasm is the highest form of critique? maybe, but at least it points out that the article could’ve been shorter and less preachy.
Marcia Hayes
January 14, 2026 AT 09:10Just a friendly reminder: even a short daily prayer can be a powerful anchor, but never skip your meds for it – balance is key.