Why Sleep Medications Aren’t Always the Answer
Over 4% of U.S. adults use prescription sleep medications each month, but many don’t know the hidden risks. These drugs might help you fall asleep tonight, but they come with serious dangers like dependence, next-day drowsiness, and even dangerous sleepwalking. The sleep medications pharmaceutical agents designed to treat insomnia through central nervous system depression you take today could make your sleep worse long-term. Experts now say non-drug treatments work better and safer for most people. Let’s break down what you need to know.
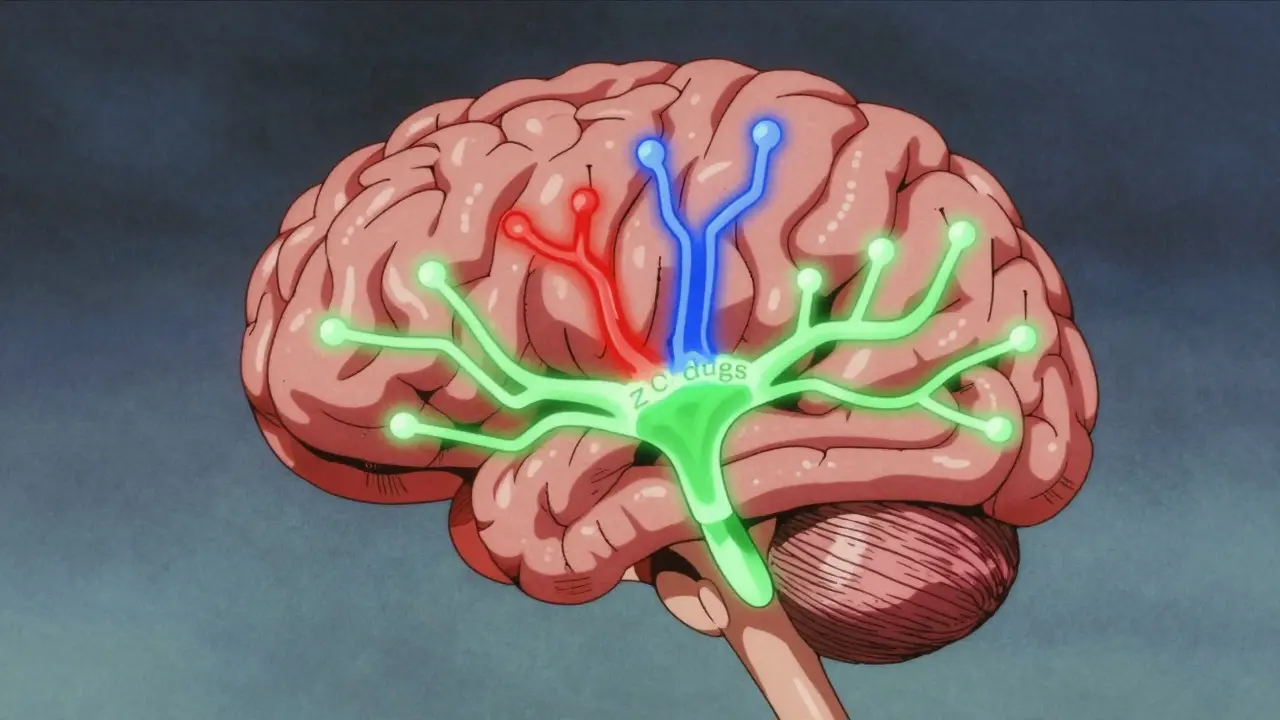
How Sleep Medications Actually Work
These drugs slow down brain activity to help you sleep. There are three main types:
- Benzodiazepines (like Xanax or Valium) - originally for anxiety, but used off-label for sleep. They boost a brain chemical called GABA, which calms nerve activity. However, they carry high dependence risk.
- Z-drugs (Ambien, Lunesta, Sonata) - developed as “safer” alternatives to benzodiazepines. They target specific GABA receptors but still cause next-day impairment.
- OTC sleep aids (like Benadryl or Unisom) - antihistamines that cause drowsiness. These can lead to confusion, dry mouth, and even dementia risk with long-term use.
Each type has trade-offs. Benzodiazepines work faster but cause more dependence. Z-drugs are slightly better for staying asleep but still pose serious risks. OTC options seem harmless, but they’re not safe for regular use.
Hidden Dangers of Sleep Medications
Many people think sleep meds are harmless short-term fixes. But research shows serious risks:
- Next-day impairment affects 25% of users. The FDA warned in 2019 that zolpidem (Ambien) can leave you with “hangover” effects equal to a 0.05-0.08% blood alcohol level - enough to make driving dangerous.
- Parasomnias like sleepwalking or sleep-driving happen in 0.5% of Z-drug users. The FDA added a black-box warning for this in 2019.
- Dependence can develop in as little as 2-5 weeks. Benzodiazepines have a 33% dependence rate after 6 weeks, while Z-drugs still carry 5-10% risk.
- Older adults face a 50-60% higher fall risk from these drugs. The American Geriatrics Society strongly advises against them for seniors.
These aren’t rare side effects. In a 2022 Sleep Medicine survey, 27% of users reported next-day impairment affecting work performance. If you’re taking sleep meds, you’re likely risking more than just sleep quality.
How Dependence Develops (And How to Avoid It)
Dependence isn’t just about addiction. It’s when your body adapts to the drug. When you stop, your brain struggles to regulate sleep naturally. Symptoms include:
- Rebound insomnia - sleeping worse than before starting meds
- Anxiety, tremors, or panic when you skip a dose
- Needing higher doses for the same effect
Dr. Nitun Kapoor, a sleep specialist, explains: “When patients stop after regular use, their sleep often worsens temporarily. This makes them feel like they need the medication to function.” That’s why stopping abruptly is dangerous. If you’ve been using sleep meds for over a month, work with your doctor to taper off slowly (usually 25% reduction every two weeks). A 2021 JAMA study found 40% of patients need extra support to quit safely.
Effective Alternatives to Sleep Medications
The Cognitive Behavioral Therapy for Insomnia (CBT-I) a structured program that teaches sleep habits and cognitive strategies to improve sleep quality is the gold standard for long-term treatment. Unlike pills, it addresses the root causes of insomnia without side effects. Here’s what works:
- CBT-I therapy - 70-80% of people see lasting improvement. It involves sleep scheduling, relaxation techniques, and changing negative thoughts about sleep.
- Digital CBT-I apps - The FDA-approved Somryst app (launched 2020) has 60% remission rates in clinical trials. It’s prescription-only but more accessible than in-person therapy.
- Lifestyle changes - Cutting caffeine after 2 PM, keeping bedrooms cool and dark, and avoiding screens before bed. These simple steps improve sleep for 65% of people.
- Melatonin supplements - Best for circadian rhythm issues (like jet lag). They have no dependence risk but don’t work for most chronic insomnia cases.
WebMD data shows 78% of users who tried CBT-I reported better long-term results than medication alone. The catch? It takes 4-6 weeks of consistent effort. But unlike pills, the benefits last forever.
When Sleep Medications Might Be Necessary
Doctors only recommend sleep meds for short-term use (2-5 weeks) when:
- You’re going through a major life stressor (grief, job loss, surgery recovery)
- Other treatments haven’t worked after 4+ weeks
- You have severe insomnia with no other options
Even then, follow these rules:
- Start with the lowest dose possible (e.g., 5mg zolpidem for women, 2.5mg for seniors)
- Avoid alcohol completely - it triples overdose risk
- Take meds only when you can sleep 7-8 hours (no driving or working after)
- Never refill without consulting your doctor
Most healthcare systems now require proof of CBT-I referral before prescribing sleep meds beyond 30 days. This isn’t bureaucracy - it’s science. The American Academy of Sleep Medicine states CBT-I is always the first choice because it works better long-term with no risks.
Frequently Asked Questions
Can sleep medications cause addiction?
Yes, especially benzodiazepines. Dependence can develop in as little as 2-5 weeks of regular use. Withdrawal symptoms include anxiety, insomnia, and tremors. Always taper off under medical supervision. Z-drugs have lower dependence risk (5-10%) but still require caution.
What’s the safest alternative to sleep meds?
Cognitive Behavioral Therapy for Insomnia (CBT-I) is the safest long-term solution. It has no side effects and works better than medication over time. For quick help, melatonin supplements may assist with sleep timing but don’t address underlying causes. Digital CBT-I apps like Somryst are FDA-approved and effective for most people.
Do OTC sleep aids like Benadryl work?
They’re not safe for regular use. Diphenhydramine (Benadryl) has anticholinergic effects that increase dementia risk by 54% with long-term use. It also causes next-day grogginess and dry mouth. These OTC options are meant for occasional use only - never as a nightly sleep aid.
Why do doctors recommend CBT-I first?
Because it works better long-term. CBT-I has 70-80% effectiveness rates without the risks of medication. It teaches skills that last forever, while pills only help while you’re taking them. The American Academy of Sleep Medicine calls CBT-I the “first-line treatment” for insomnia due to strong evidence.
Can I stop sleep meds cold turkey?
Never. Stopping abruptly can cause severe rebound insomnia, anxiety, or seizures. Work with your doctor to create a tapering plan (usually reducing by 25% every two weeks). A 2021 JAMA study found 40% of patients need extra support to quit safely.


Mark Harris
February 7, 2026 AT 00:45Switched to CBT-I after months of struggling with Ambien. No more next-day grogginess! My productivity's through the roof. Seriously, if you're on meds, talk to your doc about alternatives. It's worth the effort.
Savannah Edwards
February 8, 2026 AT 08:49I've been dealing with insomnia for years and tried everything. The part about benzodiazepines causing dependence in just 2-5 weeks really hit home. I was on Xanax for sleep and didn't realize how quickly it happened. Now I'm doing CBT-I through a digital app, and while it takes time, it's worth it. No more scary side effects like sleepwalking. Seriously, if you're on meds, talk to your doc about alternatives. Your body will thank you.
For example, the FDA warning on zolpidem says it can leave you with hangover effects equal to a 0.05-0.08% blood alcohol level. That's enough to make driving dangerous. I didn't know that until I read this post. I used to take Ambien every night without thinking twice. Now I'm working with a therapist to adjust my sleep habits. It's been tough, but I'm seeing real progress. The key is consistency. CBT-I isn't a quick fix, but it's sustainable. Unlike pills that only work while you're taking them, CBT-I gives you skills for life. I've also started cutting out caffeine after 2 PM and keeping my room cool. Small changes add up. It's not easy, but it's worth it. I'm finally getting restful sleep without any side effects.
Mayank Dobhal
February 9, 2026 AT 13:51Same here. Ambien was a nightmare. Switched to CBT-I and life's better. No more sleepwalking incidents. Just do it.
Marcus Jackson
February 10, 2026 AT 18:21Actually, the FDA warning on Ambien is correct. 0.05-0.08% blood alcohol equivalent. That's like having a drink before driving. Most people don't realize how dangerous that is. You should always check with a doctor before taking sleep meds.
Natasha Bhala
February 12, 2026 AT 10:44totally agree. i used to think sleep meds were harmless but after reading this switched to CBT-I. my doctor helped me taper off safely. now i sleep better naturally. its all about the right steps!
Gouris Patnaik
February 13, 2026 AT 23:10CBT-I is great, but you need to do it right. In India, they have better sleep practices without meds. Western medicine is too reliant on pills. You should try yoga and meditation instead.
Jesse Lord
February 15, 2026 AT 06:14Many people don't know about the 50-60% higher fall risk for seniors. My grandma was on sleep meds and almost fell. Now she's doing CBT-I and doing great. It's scary how common these risks are.
AMIT JINDAL
February 17, 2026 AT 05:51Ah, yes! The American Geriatrics Society says it all. But you know what? In India, we don't have these issues because we don't take pills. We use herbal remedies. 😎 Also, the FDA warning is just a way to push CBT-I. Big Pharma is scared.
Catherine Wybourne
February 18, 2026 AT 06:56Sleep meds might seem like a quick fix, but they're like using a bandaid on a broken leg. CBT-I takes work, but it's the real solution. I've seen so many people improve without drugs. It's not just about sleeping-it's about waking up to a better life. 🌟
For instance, the FDA's warning about zolpidem causing hangover effects equivalent to a 0.05-0.08% blood alcohol level is eye-opening. I never realized how dangerous that could be until I read this. And the part about dependence developing in just 2-5 weeks? Scary stuff. I was on Ambien for months before I found out. Switching to CBT-I was tough at first, but now I sleep better naturally. No more grogginess, no more risks. It's all about learning healthy habits. Things like keeping a consistent sleep schedule, avoiding screens before bed, and creating a relaxing bedtime routine. These small changes have made a huge difference. The science is clear: CBT-I works better long-term with no side effects. Why take the risk when there's a safer, more effective option?
Ashley Hutchins
February 19, 2026 AT 17:44totally agree. but you have to be disciplined. i tried CBT-I and it worked great. but some people just want the easy way out. pills are bad news. always choose natural solutions.
Lakisha Sarbah
February 20, 2026 AT 11:42discipline is key, but it's also about support. i needed help from a therapist to stick with CBT-I. it's not just willpower. everyone's different, so find what works for you.
Ariel Edmisten
February 21, 2026 AT 20:33CBT-I > meds. Period.
Niel Amstrong Stein
February 23, 2026 AT 11:27Exactly! 💯 CBT-I is the way to go. No more weird dreams or grogginess. Just better sleep naturally. 🌙
Paula Sa
February 25, 2026 AT 02:57Sleep is so important, yet we often treat it with quick fixes. This post really highlights the risks and alternatives. It's time we prioritize natural solutions over pills. The science is clear-CBT-I is the future.