SSRI-NSAID Risk Calculator
Assess Your Risk
Your Risk Assessment
Select your medications and age to see your risk assessment
When you’re taking an SSRI for depression or anxiety and an NSAID for arthritis or back pain, you might think you’re just managing two separate conditions. But what you might not realize is that together, these two common medications can quietly increase your risk of a dangerous internal bleed - one that could land you in the hospital.
Why This Combination Is Riskier Than You Think
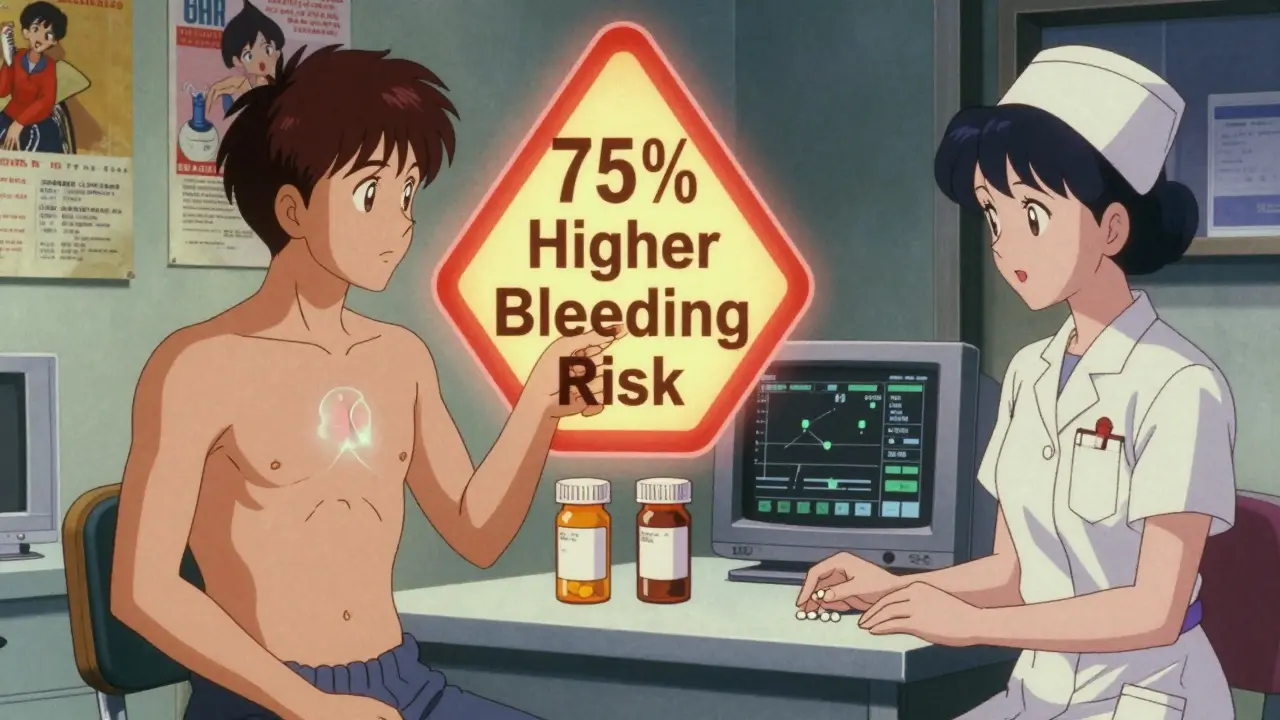
Selective serotonin reuptake inhibitors (SSRIs) like sertraline, fluoxetine, and citalopram are among the most prescribed antidepressants in the UK and US. Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, naproxen, and diclofenac are the go-to for everything from headaches to chronic joint pain. Both are safe on their own for most people. But when taken together, their effects on your stomach lining and blood clotting don’t just add up - they multiply.SSRIs reduce the amount of serotonin available to your platelets. Serotonin helps platelets stick together when you bleed. Without enough of it, your blood doesn’t clot as quickly. NSAIDs, meanwhile, attack the protective mucus layer in your stomach by blocking COX-1 enzymes. This leaves your stomach lining exposed to acid and prone to ulcers. When you combine them, you get a double hit: slower clotting and a weaker barrier. The result? A 75% higher risk of upper gastrointestinal bleeding compared to using either drug alone.
This isn’t theoretical. A major 2023 analysis of over 10 studies confirmed this exact risk increase. Even more concerning: the risk jumps even higher in people over 65, those with a history of ulcers, or anyone also taking low-dose aspirin. In fact, this combination is now considered one of the most dangerous drug interactions in primary care - not because it’s rare, but because it’s so common and often overlooked.
Not All SSRIs or NSAIDs Are Equal
You might assume all SSRIs carry the same bleeding risk. They mostly do - but there are subtle differences. Studies suggest escitalopram may be slightly less likely to interfere with platelets than fluvoxamine or paroxetine, though the difference is small enough that switching shouldn’t be done lightly without medical advice.With NSAIDs, the variation is much clearer. Non-selective NSAIDs like naproxen and diclofenac are the worst offenders. They block both COX-1 and COX-2 enzymes, wiping out the stomach’s natural defenses. Ibuprofen is a bit gentler on the gut, especially at low doses (like 200mg taken occasionally). But even ibuprofen isn’t risk-free when paired with an SSRI.
Celecoxib, a COX-2 selective NSAID, is the safest option in this class. It spares COX-1, so it doesn’t strip away your stomach’s protective lining nearly as much. Studies show it increases GI bleeding risk by only about 16% - close to baseline. That’s why doctors often recommend celecoxib for patients who need long-term pain relief and are already on an SSRI.
Who’s Most at Risk - And Why Most Don’t Know
Age is the biggest factor. If you’re over 65, your stomach lining naturally thins, your kidneys clear drugs slower, and your body’s ability to repair tissue declines. Add an SSRI and NSAID, and your bleeding risk can be three to five times higher than a younger person’s.History of ulcers? That’s another red flag. Even if you haven’t had one in years, the scar tissue in your stomach remains vulnerable. And if you’re also on blood thinners like warfarin or apixaban, the risk skyrockets further.
Here’s the problem: most people aren’t warned. A 2022 survey found that nearly 7 out of 10 patients prescribed both an SSRI and an NSAID were never told about the bleeding risk. Doctors often assume patients know, or they assume the patient’s pain is too severe to avoid NSAIDs. But patients rarely bring it up. They don’t connect their black, tarry stools or sudden dizziness to their meds.
Online forums are full of stories like this: someone on sertraline takes ibuprofen for a bad back, starts passing dark stools, waits a few days thinking it’s ‘just indigestion,’ then ends up in A&E with a bleeding ulcer. These aren’t rare cases. They’re predictable.
What You Can Do - Practical Steps to Reduce Risk
If you’re on both an SSRI and an NSAID, here’s what you should do - no waiting, no guesswork.- Ask if you really need the NSAID. Can acetaminophen (paracetamol) do the job? It doesn’t affect platelets or the stomach lining. For many types of pain - headaches, muscle aches, mild arthritis - it’s just as effective without the bleeding risk.
- If you must use an NSAID, choose celecoxib. It’s more expensive, but it’s the safest option in this class. If cost is an issue, stick to low-dose ibuprofen (no more than 1200mg per day) and only use it for short periods.
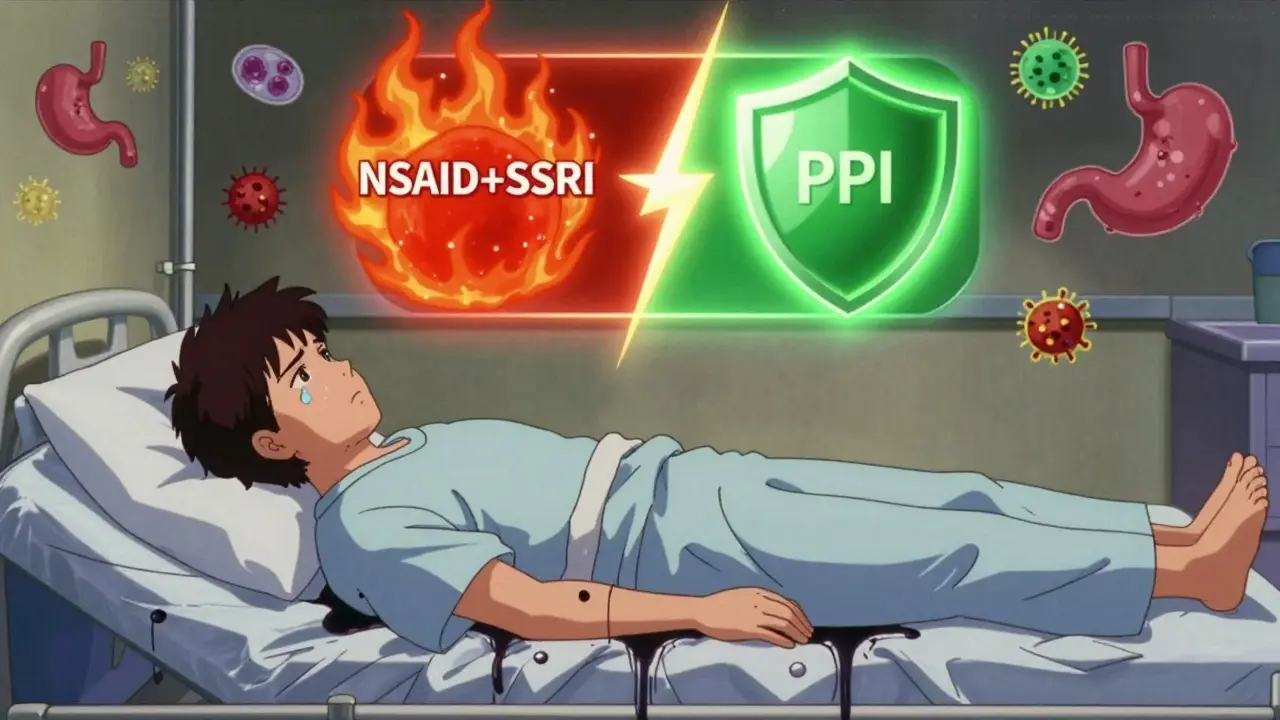
- Ask for a proton pump inhibitor (PPI). Omeprazole 20mg daily is the standard recommendation. It reduces stomach acid enough to let your lining heal and protects against ulcers. Studies show PPIs cut the excess bleeding risk from SSRI-NSAID combos by about 70%. That’s not a small win - it’s the difference between moderate risk and near-normal risk.
- Get tested for H. pylori. This bacteria causes most peptic ulcers. If you have it, treating it before starting long-term NSAID therapy can cut your bleeding risk in half. Your GP can order a simple breath or stool test.
- Watch for warning signs. Black, sticky stools (like tar), vomiting blood or material that looks like coffee grounds, sudden dizziness, or unexplained fatigue could mean internal bleeding. Don’t wait. Go to urgent care or call 111 immediately.
What Your Doctor Should Be Doing
Doctors aren’t ignoring this - but many are overwhelmed. In 2021, only 22% of GPs consistently prescribed PPIs to patients on both SSRIs and NSAIDs. Electronic health record systems in places like Cleveland Clinic now flag this interaction automatically. When a doctor tries to prescribe ibuprofen to someone on sertraline, a pop-up says: “High risk of GI bleeding. Consider PPI co-therapy or alternative pain relief.” Since implementing this in 2020, that hospital saw a 42% drop in related hospital admissions.The American College of Gastroenterology now recommends routine PPI use for anyone on this combo - especially if they’re over 60, have a history of ulcers, or take other blood-thinning meds. Yet in the UK, many GPs still don’t have these alerts. You may need to bring it up yourself.
The Bigger Picture: Why This Keeps Happening
It’s not just about ignorance. SSRIs and NSAIDs are everywhere. In the US alone, over 34 million people take antidepressants - most of them SSRIs. Nearly 17 million take NSAIDs daily for chronic pain. That’s tens of millions of people potentially exposed to this interaction. The annual cost of treating the resulting bleeds in the US is over $1.2 billion. In the UK, the NHS spends millions more on emergency admissions, endoscopies, and blood transfusions for these preventable cases.Regulators have acted. The FDA added a warning to SSRI labels in 2019. The EMA followed in 2020. But warnings on a drug leaflet aren’t enough. Patients rarely read them. Pharmacists don’t always flag it. And doctors, under time pressure, often default to the easiest solution: prescribing what’s familiar.
The future is changing. Companies are testing pills that combine NSAIDs with built-in PPIs - like a single capsule of ibuprofen and omeprazole. Early results look promising. Meanwhile, AI tools are being trained to predict individual bleeding risk based on age, genetics, and medical history. One model from 2023 correctly predicted risk in 86% of cases using just EHR data.
But for now, the solution is simple: if you’re on both, talk to your doctor. Ask if you can switch to acetaminophen. Ask if you need a PPI. Ask if you should be tested for H. pylori. Don’t assume it’s fine because you’ve been taking them for months. Bleeding doesn’t always come with warning. Sometimes, it just happens.
What If You’re Already Bleeding?
If you notice black, tarry stools, vomit blood, or feel faint and weak - don’t wait. Call 111 or go to A&E. These are signs of active bleeding. You’ll need urgent endoscopy, possibly blood transfusions, and immediate stopping of both medications. Delaying care can be life-threatening.Even if you’re not bleeding, if you’ve been on this combo for more than three months without a PPI, it’s time to have a conversation. Your stomach doesn’t show pain until it’s too late. Prevention isn’t optional - it’s essential.
Can I take ibuprofen with sertraline?
You can, but it’s not safe without protection. Taking ibuprofen with sertraline increases your risk of stomach bleeding by 75%. If you need to take them together, you should also take a proton pump inhibitor like omeprazole 20mg daily. Consider switching to acetaminophen for pain relief instead, or ask your doctor about celecoxib, which carries a much lower bleeding risk.
Do all SSRIs cause bleeding?
Most SSRIs - including fluoxetine, sertraline, citalopram, and escitalopram - carry a similar risk because they all affect platelet serotonin. Some studies suggest escitalopram may be slightly less likely to interfere with clotting, but the difference is small. Don’t switch SSRIs just to reduce bleeding risk unless your doctor recommends it for other reasons.
What’s the safest NSAID to take with an SSRI?
Celecoxib is the safest NSAID option when combined with an SSRI. It doesn’t block the COX-1 enzyme that protects your stomach lining, so it causes far less bleeding risk than naproxen, diclofenac, or even ibuprofen. If celecoxib isn’t affordable, use the lowest effective dose of ibuprofen for the shortest time possible - and always take a PPI.
Should I stop my SSRI if I need an NSAID?
No - don’t stop your SSRI without talking to your doctor. Stopping suddenly can cause withdrawal symptoms and worsen depression or anxiety. Instead, focus on safer pain relief options and add a PPI. If your pain is severe and NSAIDs are unavoidable, your doctor can help you manage the risk without stopping your antidepressant.
How long should I take a PPI with SSRIs and NSAIDs?
If you’re on both medications long-term - say, for chronic pain and depression - you should take a PPI daily as long as you’re using the NSAID. If you’re only taking the NSAID occasionally, take the PPI on days you use it. Never stop a PPI suddenly if you’ve been on it for more than a few weeks - talk to your doctor about tapering.
Can I use natural remedies instead of NSAIDs?
Some natural options like turmeric, ginger, or omega-3s may help with mild inflammation, but they’re not strong enough for moderate to severe pain. They also aren’t proven to replace NSAIDs in conditions like rheumatoid arthritis. Don’t rely on them alone. If you’re trying to avoid NSAIDs, talk to your doctor about alternatives like physical therapy, acetaminophen, or non-SSRI antidepressants like bupropion that don’t affect platelets.
Next Steps: What to Do Today
If you’re on an SSRI and an NSAID right now:- Check your medicine list - do you have both?
- Look for signs of bleeding: black stools, vomiting dark material, dizziness.
- Call your GP or pharmacist and ask: “Do I need a PPI with these meds?”
- Ask if acetaminophen or celecoxib could replace your current NSAID.
- Request an H. pylori test if you’ve had stomach issues before.
Don’t wait for symptoms. This risk builds silently. A simple conversation with your doctor today could prevent a hospital visit tomorrow.


ellen adamina
January 16, 2026 AT 08:18Diane Hendriks
January 17, 2026 AT 21:29Gloria Montero Puertas
January 19, 2026 AT 01:02Tom Doan
January 20, 2026 AT 04:03Sohan Jindal
January 20, 2026 AT 13:10Frank Geurts
January 21, 2026 AT 05:02Annie Choi
January 22, 2026 AT 04:30Arjun Seth
January 22, 2026 AT 18:22Mike Berrange
January 24, 2026 AT 17:59Amy Vickberg
January 25, 2026 AT 19:35Ayush Pareek
January 27, 2026 AT 19:00Nishant Garg
January 27, 2026 AT 20:42Nicholas Urmaza
January 27, 2026 AT 20:55Nilesh Khedekar
January 28, 2026 AT 22:38