Corticosteroid Hives: What They Are, Why They Happen, and What to Do
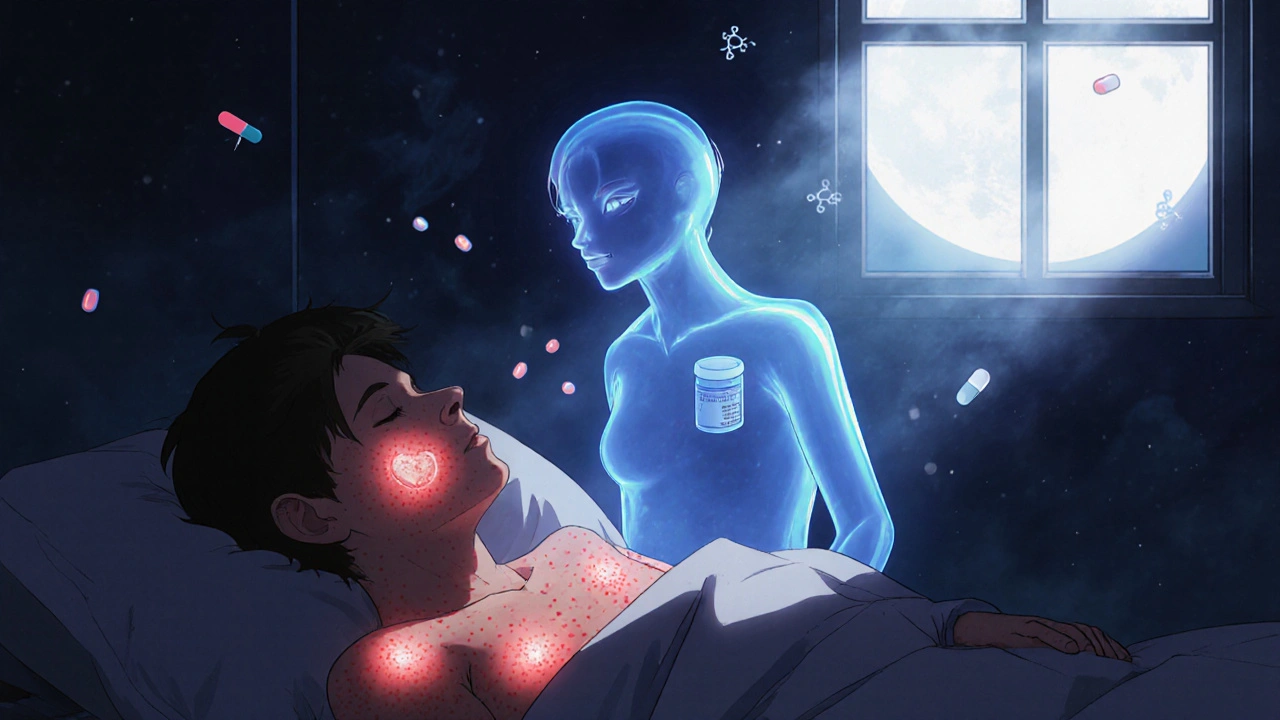
When you take corticosteroid hives, a skin reaction that can occur after using steroid medications like prednisone or hydrocortisone. Also known as steroid-induced hives, it’s not an allergy to the drug itself—it’s often the body’s odd response to sudden changes in immune activity. You might be on corticosteroids to calm down eczema, asthma, or an autoimmune flare-up, but instead of clearing your skin, you break out in itchy red welts. It sounds backwards, but it’s more common than you think.
This isn’t just a rash. corticosteroids, powerful anti-inflammatory drugs used to suppress immune overreactions. Also known as steroids, they work by dialing down your body’s defense system. But when you start, stop, or change the dose, your immune system can misfire. It’s like hitting the brakes too hard on a fast-moving car—you don’t crash, but everything shakes. That shaking can show up as hives: raised, burning, red patches that come and go. It’s not dangerous on its own, but it’s confusing and frustrating when you’re taking the medicine to feel better.
And it’s not just about the drug. allergic reaction, the immune system’s overzealous response to something harmless. Also known as hypersensitivity, it’s what corticosteroids are meant to stop—but sometimes they accidentally trigger it instead. People who’ve had chronic inflammation for months or years are especially prone. Their immune system is already on edge. When steroids suddenly quiet it down, the rebound effect can look like a flare-up. It’s not the medicine causing the allergy—it’s the body trying to find balance again.
What makes this worse? Stopping steroids too fast. Going from 20mg of prednisone to zero in a week? That’s a recipe for rebound hives. Even switching from oral to topical steroids can cause this. And if you’ve been on long-term steroids, your body’s natural cortisol production is suppressed. When you cut back, your system doesn’t know how to respond—so it sends out signals that look like hives.
So what do you do? Don’t panic. Don’t stop the medicine cold. Talk to your doctor. They might slow the taper, switch to a different steroid, or add an antihistamine like cetirizine to help calm the skin. Sometimes, a short burst of another anti-inflammatory helps. The key is recognizing this isn’t a failure of treatment—it’s a known side effect with a known fix.
You’ll find posts here that dig into how steroids interact with other meds, why some people get hives while others don’t, and how to tell if it’s truly steroid-induced or something else. We cover real cases, not just theory. You’ll learn how to track your symptoms, what questions to ask your doctor, and how to avoid common mistakes when coming off steroids. This isn’t about guessing. It’s about knowing what’s happening to your body—and how to fix it without risking more problems.