Sleep Quality: How Medications, Lifestyle, and Health Conditions Affect Your Rest
When you struggle with sleep quality, how well and how deeply you rest through the night. Also known as sleep efficiency, it’s not just about how many hours you spend in bed—it’s about whether your body and brain actually recover. If you wake up tired even after eight hours, something’s off. And it’s rarely just stress.
Many common medications quietly wreck sleep quality. Antidepressants like Venlafaxine, diabetes drugs like Metformin, even nasal sprays used for congestion can disrupt your natural sleep cycle. Some pills make you drowsy during the day but keep you awake at night. Others suppress deep sleep or cause restless legs. And if you’re taking multiple meds, interactions can make it worse. It’s not always the pill’s main job—it’s a side effect you didn’t see coming.
Then there’s the hidden link between sleep quality, the depth and restoration of your nightly rest. Also known as sleep efficiency, it’s not just about how many hours you spend in bed—it’s about whether your body and brain actually recover. Many common medications quietly wreck sleep quality. Antidepressants like Venlafaxine, diabetes drugs like Metformin, even nasal sprays used for congestion can disrupt your natural sleep cycle. Some pills make you drowsy during the day but keep you awake at night. Others suppress deep sleep or cause restless legs. And if you’re taking multiple meds, interactions can make it worse. It’s not always the pill’s main job—it’s a side effect you didn’t see coming.
Then there’s the hidden link between appetite changes, how drugs alter hunger signals and food cravings. Also known as medication-induced appetite shifts, it’s a common but overlooked driver of poor sleep. If your meds make you hungrier at night, you’re more likely to snack, spike blood sugar, or feel uncomfortable lying down. Same if you lose your appetite and wake up hungry. Blood sugar swings, acid reflux from late eating, or even anxiety from hunger—all these mess with sleep. And it’s not just food. Alcohol might help you fall asleep, but it kills REM sleep. That’s why you wake up feeling like you didn’t rest at all.
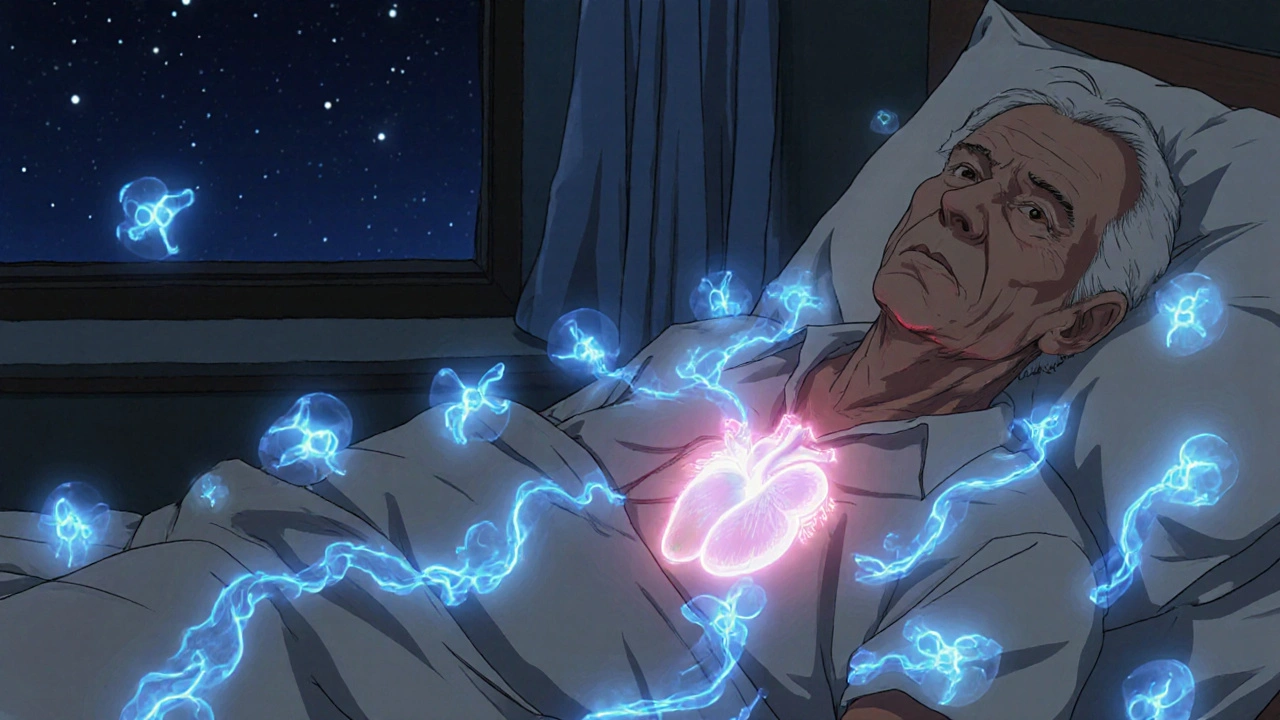
Chronic conditions like COPD, Parkinson’s, and even psoriasis don’t just hurt during the day—they make nights worse. Roflumilast helps COPD flare-ups, but the coughing and breathing trouble? That’s a sleep killer. Skin chafe from psoriasis flares can keep you tossing and turning. And if you’re dealing with tinnitus, the ringing in your ears doesn’t stop when the lights go out. These aren’t just annoyances—they’re sleep disruptors with real medical roots.
What’s missing from most sleep advice? The connection between what you take and how you rest. You won’t fix poor sleep quality by just avoiding screens or drinking chamomile tea if your medication is the real culprit. The posts below dig into exactly that: which drugs mess with sleep, how to spot the signs, and what to do next—without quitting your treatment. You’ll find real talk on rebound congestion from nasal sprays, why antidepressants like Venlafaxine can cause insomnia, how diabetes meds affect your nighttime rhythm, and what to ask your doctor when your sleep won’t improve. No fluff. No guesswork. Just clear links between your pills and your nights.