Steroid for Hives: What Works, What to Avoid, and Real Results
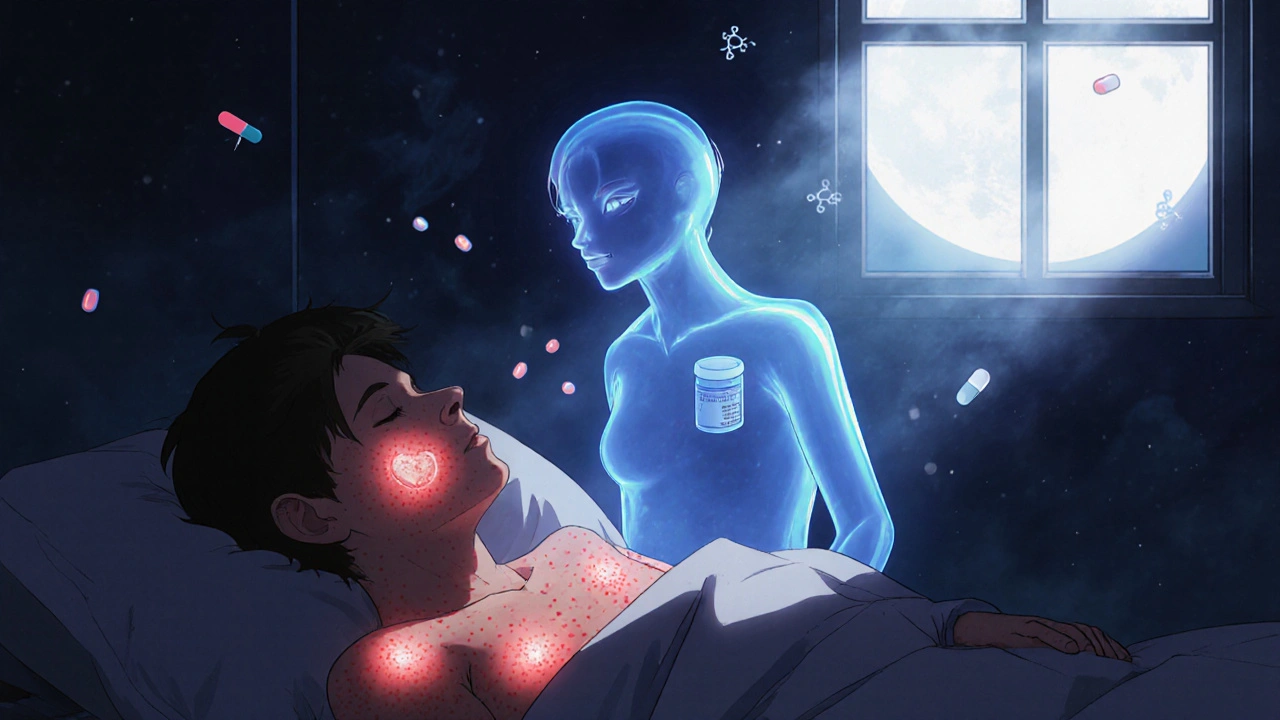
When hives show up suddenly—itchy, red, raised patches on your skin—it’s easy to reach for something strong. A steroid for hives, a type of anti-inflammatory medication that reduces immune system overreaction. Also known as corticosteroids, it works by calming the body’s overactive response to allergens, irritants, or even stress. But here’s the truth: steroids aren’t always the best first move. Most cases of hives get better with simple antihistamines like cetirizine or loratadine. Steroids are usually saved for when those don’t cut it—or when hives are severe, widespread, or last longer than six weeks.
Not all hives are the same. Acute hives, which last less than six weeks, often come from food, insect bites, or infections. Chronic hives, lasting months or years, are trickier. They’re rarely caused by allergies and more often linked to autoimmune issues. That’s where a short course of oral steroids like prednisone might be prescribed. But here’s what no one tells you: steroids don’t fix the root cause. They just mute the symptoms. And using them too often or for too long can lead to weight gain, mood swings, high blood pressure, or even bone thinning. That’s why doctors don’t hand them out like candy.
What you really need to know is this: corticosteroids, prescription drugs that suppress inflammation and immune activity. Also known as systemic steroids, they’re powerful but not magic. Topical steroid creams? Usually useless for hives—they’re designed for localized skin conditions like eczema, not raised, spreading welts. Injections? Rarely used unless it’s an emergency. Pills are the go-to when steroids are needed at all. And even then, they’re often paired with antihistamines to cover more bases.
There’s also a big gap in what people expect versus what actually helps. Many think steroids are the go-to fix for hives because they work fast. But fast doesn’t mean safe long-term. The real winners for most people are non-drowsy antihistamines, avoiding known triggers like heat, tight clothes, or certain foods, and keeping stress low. Some studies show that up to 40% of chronic hives cases improve with just lifestyle tweaks and consistent antihistamine use—no steroids needed.
If you’ve been told you need a steroid for hives, ask why. Is it because the antihistamines didn’t work? Or because your doctor assumes it’s the next step? Don’t assume stronger means better. Sometimes, the best treatment is the one you don’t have to take at all.
Below, you’ll find real-world comparisons and insights from people who’ve dealt with hives, steroids, and everything in between. You’ll see what works, what doesn’t, and how to make smarter choices without guessing.