Urticaria Treatment: What Works, What to Avoid, and How to Find Relief
When your skin breaks out in itchy, raised red welts—urticaria, a common skin condition also known as hives. Also known as hives, it can show up out of nowhere and turn your day upside down. It’s not just a rash. It’s your body’s reaction to something—food, stress, medicine, heat, or even nothing obvious at all. For some, it lasts hours. For others, it sticks around for weeks, months, or longer. That’s when it becomes chronic urticaria, a form of hives that lasts six weeks or more without a clear trigger. The good news? Most cases are manageable. The bad news? Many people waste time on remedies that don’t work while ignoring what actually does.
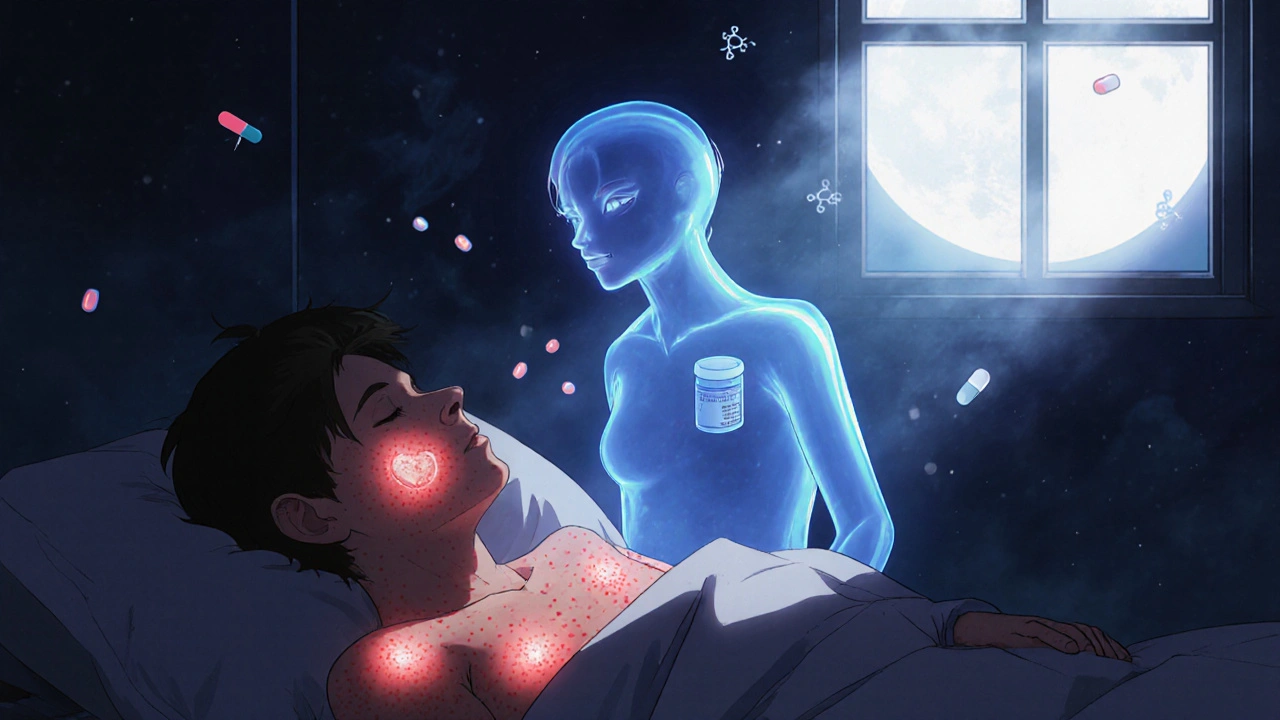
First, understand what’s happening. Your body releases histamine, a chemical that causes swelling and itching. That’s why antihistamines, the first-line treatment for urticaria, block histamine to reduce itching and swelling. Drugs like cetirizine, loratadine, or fexofenadine are often the first thing doctors recommend. They’re usually safe, non-drowsy, and work for most people. But if they don’t cut it, higher doses or second-line options like omalizumab (an injectable biologic) may be needed. Don’t skip the doctor just because it’s "just hives." If you’re on daily antihistamines for more than a few weeks, you need to know why it’s happening. Is it an allergy? An autoimmune issue? A reaction to a medication you’ve been taking? allergic reaction, a common cause of acute urticaria, but not the only one. Triggers like NSAIDs, antibiotics, or even aspirin can cause hives without a true allergy. And stress? It doesn’t cause hives, but it can make them worse—big time.
What you should avoid is just as important as what you try. Hot showers, tight clothes, alcohol, and spicy food can all make hives flare. So can scratching. It sounds obvious, but people do it—and then wonder why it gets worse. Skip the old home remedies like baking soda pastes or ice packs unless they’re part of a doctor-approved plan. They might give quick relief, but they don’t fix the root issue. And never stop or change your meds without talking to your provider. Some people try to "tough it out" or switch to random supplements they found online. That’s risky. Urticaria treatment isn’t one-size-fits-all. What works for your friend might do nothing for you—or even make things worse.
This collection of posts doesn’t just list drugs or quick fixes. It shows you real-world choices people have made, what worked, what didn’t, and why. You’ll see comparisons between common antihistamines, stories about managing chronic hives, and warnings about hidden triggers hiding in everyday products. No theory. No fluff. Just what you need to know to take control—before the next flare-up hits.