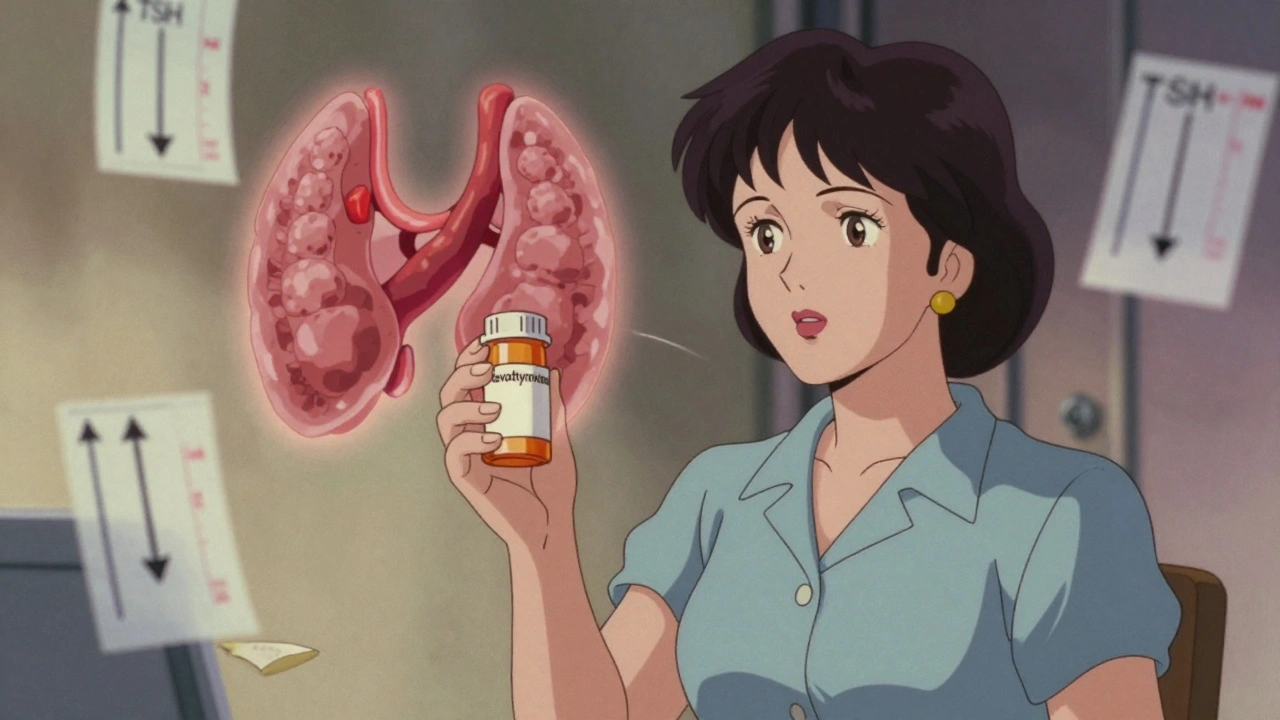
Levothyroxine is one of the most common prescription drugs in the UK, with over 260 million packs dispensed between 2016 and 2020. For millions of people with hypothyroidism, it’s the difference between constant fatigue and feeling like themselves again. But here’s the thing: levothyroxine isn’t just a pill you take and forget. If it’s not monitored properly, it can cause serious problems - from heart palpitations to bone loss, or worse, a return of symptoms you thought were gone.
Why Levothyroxine Works - and Why It Can Go Wrong
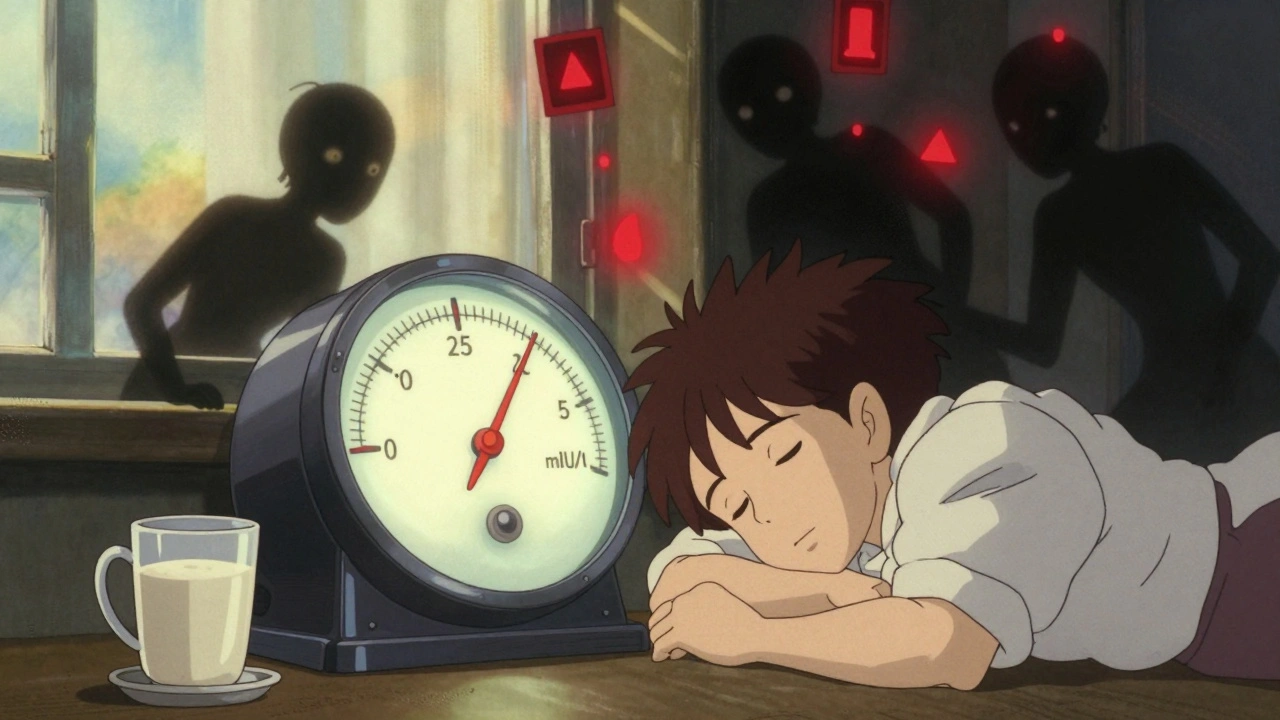
Levothyroxine is a synthetic version of T4, the main hormone your thyroid makes. When your thyroid doesn’t produce enough, this pill replaces it. Simple, right? Not quite. The body needs just the right amount. Too little, and you’re back to feeling sluggish, gaining weight, and struggling to stay warm. Too much, and you might get heart racing, anxiety, insomnia, or even muscle wasting.
The narrow window between effective and dangerous is why this medication demands precision. Unlike antibiotics or painkillers, you can’t just take it when you feel off. Levothyroxine affects your entire metabolism. A tiny change in dose - even 12.5 micrograms - can throw your system out of balance.
How Often Should You Get Tested?
Many people think once they’re on levothyroxine, they’re set for life. That’s a dangerous assumption. Guidelines from the Specialist Pharmacy Service (SPS) and the American Thyroid Association are clear: you need regular blood tests.
- After starting or changing your dose: wait 6 weeks, then get a TSH test.
- Until your levels stabilize: test every 3 months.
- Once stable: test at least once a year - but every 6 to 12 months is better.
- During pregnancy: test every 4 weeks, especially in the first half.
Yet, NHS data from 2022 shows only 58% of primary care practices follow this schedule. Over a third of patients go more than 18 months without a single TSH check - even when they’re still tired, gaining weight, or feeling anxious. That’s not just negligence. It’s a risk.
The Brand Switch Problem
Here’s something most patients don’t know: not all levothyroxine is the same.
Generic versions are cheaper and widely used. But they’re made by different manufacturers. Even though they’re supposed to be identical, small differences in fillers, coatings, or absorption rates can change how your body responds. The UK’s Medicines and Healthcare products Regulatory Agency (MHRA) received 335 reports of problems between 2015 and 2019 linked to switching brands. Symptoms? Fatigue (78%), headaches (65%), palpitations (39%), and unexplained weight gain (33%).
On patient forums like Thyroid UK, 68% of 1,245 respondents said they felt worse after a pharmacy switched their brand without telling them. One woman in Birmingham told her GP she’d been “back to square one” after her prescription changed from a branded version to a generic. Her TSH jumped from 2.1 to 8.9 - a clear sign she was under-medicated. She didn’t know to ask for a test until she was nearly fainting at work.
If you’ve ever felt off after a refill, even if the dose says the same, ask your doctor to specify the brand on your prescription. It’s your right.

When to Worry About Interactions
Levothyroxine doesn’t play well with a lot of common supplements and meds.
- Calcium supplements, iron pills, and antacids - take them at least 4 hours apart.
- Cholesterol drugs like cholestyramine can block absorption.
- Amiodarone and lithium can interfere with thyroid function.
- Even coffee, soy milk, and high-fiber meals can reduce how much you absorb.
Take your levothyroxine on an empty stomach, 30 to 60 minutes before breakfast. No coffee. No food. No supplements. Just water. That’s the rule. Skip it once, and your body doesn’t get the full dose. Do it every day, and you’re setting yourself up for failure.
Who Needs Special Care?
Not everyone gets the same dose or monitoring. Certain groups need extra attention:
- Pregnant women - thyroid needs rise by 30-50% during pregnancy.
- People over 65 - higher TSH targets (up to 7.5) are often safer to avoid heart strain.
- Those with heart disease - starting low and going slow prevents arrhythmias.
- Patients on amiodarone or lithium - these drugs can cause thyroid dysfunction on their own.
- Children and teens - growth and development depend on precise dosing.
If you fall into any of these groups, your doctor should be checking you more often. If they’re not, ask why. You’re not being difficult - you’re being smart.
What If You Still Feel Bad Even With Normal TSH?
Some people do everything right: they take their pill on time, they get tested, their TSH is in range - but they still feel exhausted, depressed, or foggy. This is more common than you think.
Research from the Mayo Clinic and the Endocrine Society suggests that 10-15% of patients may benefit from adding liothyronine (T3) to their regimen, even if TSH looks fine. It’s not standard yet, but it’s being studied. If you’re in this boat, don’t accept “your numbers are normal” as the end of the conversation. Ask about thyroid-related quality of life tools like ThyPRO or ThySRQ. These questionnaires measure how you actually feel - not just what your blood says.
Dr. Rebecca Bahn, former president of the American Thyroid Association, says 15-20% of patients need a dose adjustment every year. Why? Aging, weight changes, new meds, or even seasonal shifts in metabolism. Your body isn’t static. Your dose shouldn’t be either.
What You Can Do Right Now
You don’t need to wait for your next appointment to take control.
- Check your last TSH result. If it’s over a year old, call your GP and request a test.
- Look at your prescription. Is it named (e.g., “Levothyroxine Teva”)? If it just says “levothyroxine,” ask if you can stay on the same brand.
- Keep a simple log: time you take your pill, what you ate or drank around it, and how you feel each day.
- If you’ve switched brands and felt worse, tell your doctor - and ask for a TSH test immediately.
- Never skip a dose because you’re “feeling fine.” Thyroid hormone needs are constant.
Levothyroxine works - but only if you treat it like the serious, precision medicine it is. It’s not a vitamin. It’s not optional. It’s your body’s thermostat. Get it right, and you’ll feel better than you have in years. Get it wrong, and you’re playing Russian roulette with your health.
What Happens If You Don’t Monitor?
Untreated or poorly managed hypothyroidism leads to long-term damage. High cholesterol. Heart disease. Infertility. Depression that doesn’t lift. Osteoporosis in older adults.
And over-treatment? That’s just as dangerous. Too much levothyroxine can cause atrial fibrillation, bone thinning, and muscle loss. In older people, it’s linked to higher death rates. The MHRA reports show that many adverse events weren’t from the drug itself - they were from poor monitoring. People didn’t know their dose was too high. Or they didn’t realize a pharmacy switch had changed their absorption.
This isn’t hypothetical. It’s happening in GP surgeries across the UK right now.
Can I switch levothyroxine brands without telling my doctor?
No. Even though the dose is the same, different brands can affect how your body absorbs the hormone. If you switch and feel worse - tired, anxious, or gaining weight - get a TSH test. Ask your doctor to specify your brand on the prescription to avoid future changes.
How long does it take for levothyroxine to work?
You may notice small improvements in energy within 2-3 weeks, but full symptom relief usually takes 3 to 6 months. That’s because your body needs time to rebalance its metabolism. Don’t rush to change your dose - wait for blood tests before adjusting.
Is it safe to take levothyroxine for life?
Yes - if it’s monitored properly. Millions of people take it for decades without issues. The risk comes from inconsistent dosing, poor testing, or ignoring interactions. As long as your TSH is checked regularly and your dose is adjusted as needed, lifelong use is safe and effective.
Can coffee or calcium interfere with levothyroxine?
Yes. Coffee, calcium supplements, iron pills, and antacids can block absorption. Take your pill with water, 30 to 60 minutes before breakfast. Wait at least 4 hours before taking any of these other items.
What’s the ideal TSH level for someone on levothyroxine?
There’s no single number. For most adults, the target is 0.5 to 4.5 mIU/L. But for older adults (over 65), a level up to 7.5 may be safer. Pregnant women need tighter control - usually under 2.5. Your doctor should tailor your target based on your age, heart health, and symptoms - not just a lab range.
Should I get Free T4 tested too?
TSH is usually enough. But if your symptoms don’t match your TSH - for example, you feel hyperthyroid but your TSH is normal - ask for Free T4. It can help spot absorption issues or rare conditions like thyroid hormone resistance.
Can I stop levothyroxine if I feel better?
No. Hypothyroidism is usually a lifelong condition. Stopping the medication will bring your symptoms back - often worse than before. Your thyroid won’t suddenly start working again. Always consult your doctor before making any changes.
Final Thought: Your Body Knows When Something’s Off
Levothyroxine is powerful. It can give you your life back. But it’s not magic. It’s medicine. And like all medicine, it needs respect. If you’re tired, bloated, or anxious - and your doctor says “your numbers are fine” - push back. Ask for a test. Ask about your brand. Ask if your dose still fits your life.
Because the truth is, you know your body better than any lab result. Trust that. But back it up with data. That’s how you stay safe - and truly well.

alaa ismail
December 3, 2025 AT 15:29Been on levothyroxine for 8 years. The brand switch thing hit me hard last year - switched from Tirosint to a generic and suddenly I was crashing by 3pm. Took me 3 months to get my doc to listen. TSH went from 2.3 to 7.1. Now I demand the brand on my script. No more guessing games.
Also, coffee? Yeah, I used to take it with my pill. Big mistake. Now I wait 90 minutes. Life changed.
Stop treating this like a vitamin. It’s a precision tool.
Allan maniero
December 5, 2025 AT 12:58It’s wild how something so essential gets treated like an afterthought in the NHS. I work in primary care and I’ve seen it firsthand - patients come in with TSH levels off the charts, and the last test was two years ago. Why? Because the system’s stretched thin, GPs are overloaded, and thyroid monitoring doesn’t feel urgent until someone’s in cardiac distress.
And the brand switching? That’s a silent epidemic. I’ve had patients cry because they lost their rhythm - their sleep, their focus, their ability to work - all because a pharmacist thought ‘same dose = same effect.’ It’s not science. It’s luck.
There’s a reason the MHRA got 335 reports. This isn’t about being difficult. It’s about being alive. We need mandatory brand tracking on prescriptions. No exceptions. Not for cost. Not for convenience. For safety.
Sheryl Lynn
December 6, 2025 AT 07:11Oh honey. Let me tell you about the time I took a generic levothyroxine and turned into a human anxiety grenade. I was vibrating. My heart sounded like a jackhammer. I thought I was having a panic attack - turns out, my body was screaming for its old brand. The fillers in those generics? They’re not inert. They’re little saboteurs.
And don’t even get me started on the ‘TSH is fine’ mantra. That’s like saying your car’s engine light is off so you don’t need to check the oil. My symptoms were screaming, but the lab? Silent. I demanded Free T4. Got it. Turns out my T4 was in the bottom 5%.
Thyroid isn’t a checkbox. It’s a symphony. And if your doctor’s not tuning it? Fire them.
Eddy Kimani
December 7, 2025 AT 13:16From a clinical pharmacology standpoint, the bioavailability variance between levothyroxine formulations is well-documented. The FDA and EMA both recognize that even within 10% bioequivalence thresholds, inter-patient variability can lead to clinically significant differences in serum T4/T3 levels due to gastric pH, motility, and enteric coating variations.
Moreover, the 2017 JAMA study on brand-switching in hypothyroid patients showed a 22% incidence of TSH fluctuation >1.5 mIU/L post-switch - well above the 0.5 threshold considered clinically relevant. The MHRA data aligns. This isn’t anecdotal. It’s pharmacokinetic.
Also, coffee reduces absorption by up to 36% per 2021 Clinical Endocrinology meta-analysis. Timing matters. Dose timing isn’t a suggestion. It’s a pharmacological imperative.
Chelsea Moore
December 7, 2025 AT 16:38John Biesecker
December 8, 2025 AT 11:45Man, I used to be the guy who took levothyroxine with his morning coffee and cereal. Thought I was being efficient. Turned out I was just being dumb 😅
Got a new prescription last year - switched to Tirosint because my old one kept making me feel like a zombie. Within 3 weeks? Energy like I was 25 again. My wife said I stopped sighing all day.
Also, TSH isn’t everything. I had mine ‘in range’ for a year and still felt like I was dragging through mud. Asked for Free T4 - turns out I was low. Now I take T3 too. Life’s different.
Don’t just trust the numbers. Trust your body. And if your doc won’t listen? Find a new one. You deserve to feel human again. 🙏
Genesis Rubi
December 9, 2025 AT 14:44UK’s system is broken. Americans don’t get this - you get a pill, you get no follow-up, you get a pharmacy that switches your meds without asking. Meanwhile, in the US, we have specialists who check your TSH every 3 months, and if you’re on a generic? They’ll literally call the pharmacy and demand the brand.
Why are we letting other countries treat our hormones like they’re generic soda? This isn’t ‘healthcare.’ It’s negligence dressed up as policy.
And don’t even get me started on people who say ‘it’s just a pill.’ If you’ve never had your body shut down from a thyroid crash, you don’t get to talk.
John Morrow
December 10, 2025 AT 16:20Let’s deconstruct the myth of ‘normal TSH.’ The reference range of 0.5–4.5 mIU/L is statistically derived from a population that includes undiagnosed hypothyroid patients - meaning the ‘normal’ range is contaminated by pathology.
Studies from the Endocrine Society suggest an optimal TSH for symptomatic patients is 1.0–2.0 mIU/L, especially in those under 65. Yet, most GPs treat 4.0 as the ceiling. That’s not medicine. That’s complacency.
Additionally, the brand-switching issue is exacerbated by the absence of unique product identifiers in the NHS supply chain. Without barcoding or serialization, traceability is impossible. The MHRA reports are the tip of the iceberg.
And yes - coffee. The polyphenols in roasted coffee inhibit intestinal thyroxine transporters. 30 minutes isn’t enough. 60 is the minimum. I’ve published on this.
Saurabh Tiwari
December 10, 2025 AT 21:03From India here - we don’t have brand control here at all. Pharmacies switch everything. I had the same problem as others - felt awful after switch. Took me 6 months to convince my doctor to test me. Now I pay extra for the brand I know works.
Also, coffee? Yeah, I used to drink it right after pill. Now I wait 2 hours. No more brain fog.
My mom’s on it too. She’s 72. Her TSH is 5.8. Doctor says it’s fine for age. I’m not convinced. But I don’t push. Just monitor.
Thanks for the post. Helps people like me feel less alone.
Victoria Graci
December 12, 2025 AT 10:47There’s a quiet tragedy here: thyroid patients are told their symptoms are ‘in their head’ because their labs are ‘normal.’ But the body doesn’t lie. It whispers. And if you’re not listening, it screams.
I had a TSH of 2.8 - ‘perfect’ - but I couldn’t get out of bed. My Free T4 was low-normal, Free T3 was borderline. I asked for a thyroid antibody panel. Hashimoto’s. That’s why my dose kept needing adjustment.
And the brand? I switched from Euthyrox to a generic after my insurance changed. Within a week, my hands shook. I cried in the grocery store because I couldn’t lift my bag.
Don’t wait for a crisis. Ask for the full panel. Ask for the brand. Ask for your life back. It’s not selfish. It’s survival.
Saravanan Sathyanandha
December 13, 2025 AT 17:55As someone from India who has studied endocrinology in the UK, I see how this issue transcends borders. In both systems, the patient is left to navigate a labyrinth of bureaucracy and indifference.
But here’s the hope: patient advocacy is growing. In Delhi, thyroid support groups now demand brand consistency from pharmacies. In London, patients are pushing for electronic prescribing flags for levothyroxine.
And yes - coffee, calcium, soy - they’re all saboteurs. I teach my patients to treat this pill like a sacred ritual: water, fasting, silence. No distractions.
Thyroid health is not a footnote. It’s the foundation. Treat it like one, and you rebuild your life.
ruiqing Jane
December 14, 2025 AT 07:24My sister went from needing 100mcg to 150mcg after a brand switch and no testing. She ended up in the ER with atrial fibrillation. Her doctor blamed stress.
Don’t let this happen to you. If your doctor won’t test you, go to a walk-in clinic. Get your own bloodwork. Pay out of pocket if you have to. Your life is worth more than a £20 test.
And if you’re pregnant? Don’t wait. Test every 4 weeks. Your baby’s brain is developing right now. This isn’t optional.
Stop waiting for permission. You’re your own best advocate.
Fern Marder
December 14, 2025 AT 18:30I’ve been on levothyroxine for 15 years. I’ve had 3 different brands. I’ve had TSH levels from 0.8 to 9.2. I’ve been told I’m ‘fine’ and I’ve been told I’m ‘too sensitive.’
Here’s what I know: if you feel like crap, you’re not imagining it. The lab doesn’t own your soul.
My rule? If I feel off, I test. No matter what. I’ve saved myself from depression, weight gain, and heart issues by trusting my gut over a spreadsheet.
And yes - I still take my pill with water. No coffee. No toast. No excuses. 🙌
alaa ismail
December 15, 2025 AT 05:34Just read the comment about T3 addition. I’ve been on T4-only for 8 years. Started adding 5mcg T3 last month. I didn’t think I’d feel different. But now? I wake up without an alarm. My brain doesn’t feel like cotton. I’m crying happy tears.
Don’t let anyone tell you ‘T3 isn’t proven.’ I’m living proof. Ask your endo. It’s not experimental. It’s essential for some of us.