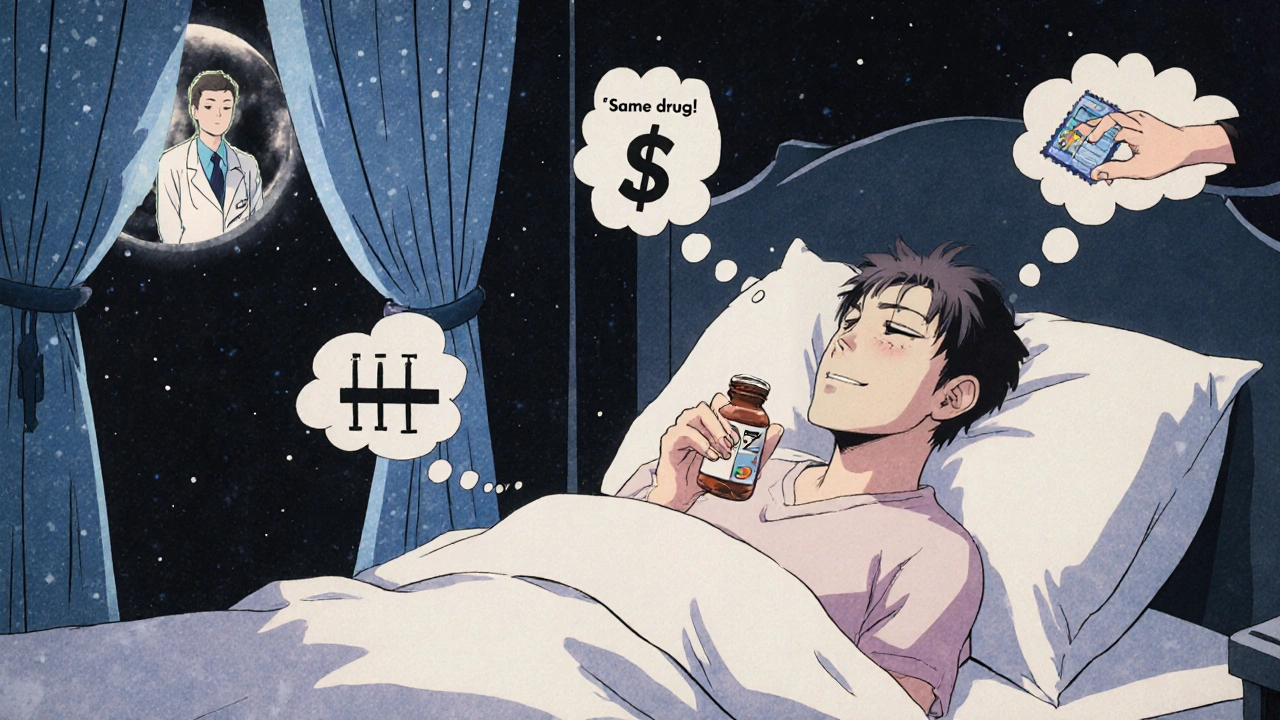
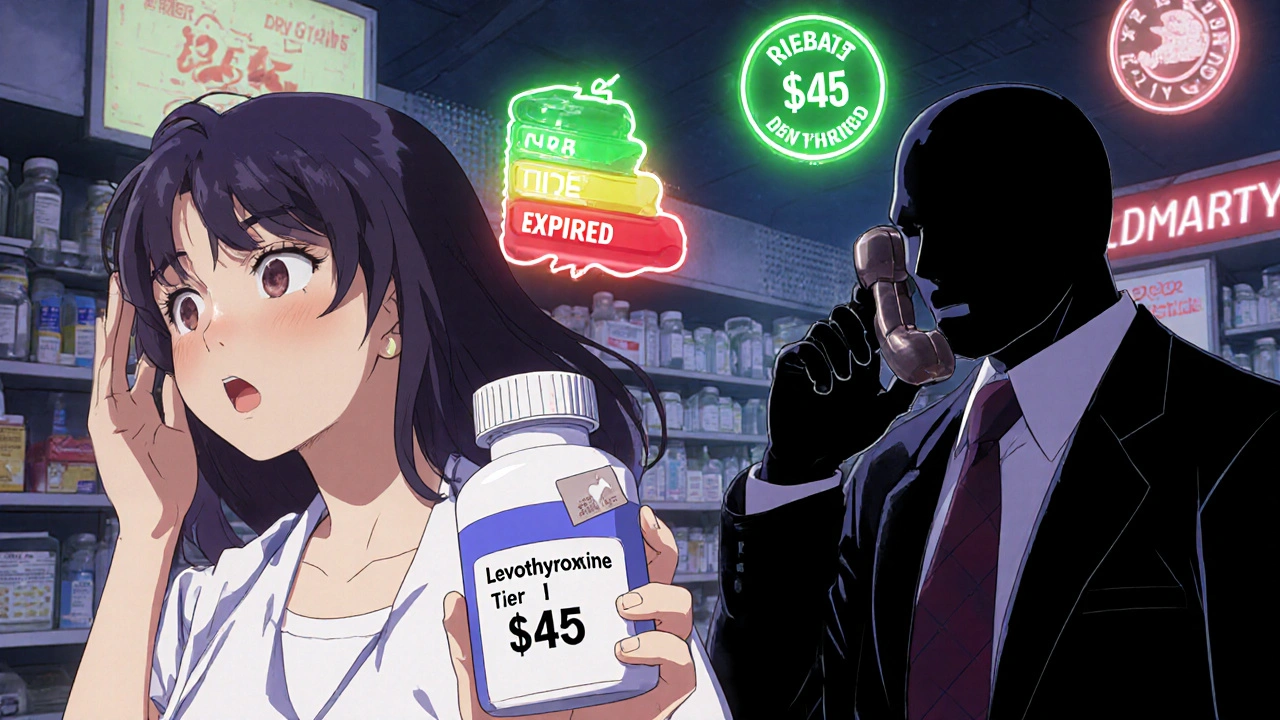
You picked up your prescription for generic levothyroxine-the same drug you’ve taken for years-and the pharmacy charged you $45. Last month, it was $5. You didn’t change anything. Your doctor says all generics are the same. So why the spike?
This isn’t a mistake. It’s the system.
Most health plans in the U.S. use something called tiered copays. Instead of charging the same amount for every drug, they sort medications into levels-tiers-and each tier has its own price tag. Tier 1 is cheap. Tier 5 is expensive. And here’s the twist: not all generic drugs are in Tier 1. Some generics, even if they’re chemically identical to cheaper versions, sit in higher tiers with much steeper copays.
How Tiered Copays Actually Work
Think of your drug plan like a grocery store with price labels that change based on who the supplier is, not what’s inside the box.
Tier 1: Preferred generics. These are the cheapest-usually $0 to $15 for a 30-day supply. Common drugs like lisinopril, metformin, or atorvastatin often land here because the manufacturer gave the pharmacy benefit manager (PBM) a big discount.
Tier 2: Non-preferred generics. Same active ingredient. Same effect. But this version? It’s $15 to $30. Why? Because the company that makes it didn’t offer the PBM a good enough rebate. It’s not about quality. It’s about money.
Tier 3: Preferred brand-name drugs. These cost more-$25 to $50. You might see them if your doctor prescribes a brand version that’s still under patent.
Tier 4 and 5: Specialty drugs. These are for complex conditions like rheumatoid arthritis, multiple sclerosis, or cancer. Even if they’re generic versions of biologics (like adalimumab), they can cost you 20-40% of the total price. A single month’s supply might be $5,000. Your share? $1,000 to $2,000.
According to data from Medicare Part D and employer plans in 2024, nearly all plans use this system. And it’s not going away. The Inflation Reduction Act caps your annual out-of-pocket drug costs at $2,000 starting in 2025-but it doesn’t change how drugs are tiered. You still pay more for some generics.
Why Your Generic Isn’t in Tier 1
Here’s the truth: your generic drug isn’t in Tier 1 because it’s better. It’s in Tier 1 because the manufacturer paid the PBM to put it there.
Pharmacy Benefit Managers-like CVS Caremark, Express Scripts, and OptumRx-negotiate rebates with drugmakers. The bigger the rebate, the lower the tier. If your generic drug’s maker didn’t offer a big enough discount, it gets bumped up. Even if it’s identical to the one in Tier 1.
Studies show that 68% of generic drugs moved to higher tiers in recent years were due to expiring rebate deals-not clinical reasons. A 2023 analysis by BOC Pharmacy Group found that 12-18% of generic medications are classified as specialty drugs (Tiers 4-5) simply because they’re expensive to make, store, or ship-even if they’re not complex biologics.
Patients don’t know this. They assume “generic” means “cheapest.” But that’s not how it works. Two pills with the exact same chemical formula can cost $10 apart because of a contract between two corporations.

The Real Impact on Patients
When a drug moves from Tier 1 to Tier 3, people stop taking it.
A 2005 study found that when diabetes medications shifted from Tier 2 to Tier 3, adherence dropped by 7.3%. That’s not a small number. It means people skipped doses, delayed refills, or went without-because they couldn’t afford it.
And it’s happening right now. In a 2023 survey by the Patient Advocate Foundation, 41% of insured adults said they’d been hit with a higher-than-expected copay for a generic drug. Two-thirds of them couldn’t get a clear answer from their insurer.
Reddit threads are full of stories like this: “My levothyroxine went from $5 to $45. My doctor says it’s the same. Why?”
Pharmacists sometimes swap your prescription automatically for the “preferred” generic. But if you’re used to one brand of generic and your body reacts differently-even slightly-you might feel off. Fatigue. Mood swings. Weight changes. These aren’t always reported. They’re just blamed on “aging” or “stress.”
Specialty generics are even worse. A patient on a generic version of adalimumab (a biologic for autoimmune disease) might pay $1,200 a month. That’s not a copay. That’s coinsurance. And if you miss a payment? Your treatment stops. Your condition flares. Your life gets harder.
What You Can Do About It
You’re not powerless. There are steps you can take.
1. Check your plan’s formulary. Every year in October, Medicare plans update their drug lists. Employer plans often do too. Log in to your insurer’s website. Search for your drug. Look for the tier. If it’s higher than expected, note the name of the specific generic version they’re covering.
2. Ask your pharmacist. They know which generics are in which tier. Ask: “Is there a different generic version of this drug that’s cheaper?” Sometimes, the same drug from a different manufacturer is in Tier 1. Just because it’s labeled “generic” doesn’t mean it’s the same product.
3. Request a therapeutic interchange. Ask your doctor to fill out a form asking your insurer to cover a lower-tier version. This isn’t a hassle. In 2024, 63% of these requests were approved.
4. Use tools like GoodRx or SmithRx. These sites show you cash prices and compare copays across tiers. You might find that paying cash for your generic is cheaper than your copay. That’s not rare.
5. Look into manufacturer assistance programs. Many drugmakers offer coupons or free medication programs for low-income patients. Even for generics. You’d be surprised how many people don’t know this exists.
What’s Changing in 2025 and Beyond
The system isn’t static. UnitedHealthcare started putting high-volume generics like atorvastatin and lisinopril into $0 copay tiers in early 2024. That’s good news-for those drugs. But they moved 87 other generics to higher tiers to balance the cost.
Express Scripts did the same. Rebates are falling. PBMs are scrambling. They’re moving more generics to higher tiers, especially those used less frequently.
Future trends? More biosimilars-generic versions of biologics-will be sorted into tiers. You’ll have multiple versions of the same drug, each with a different price. More confusion. More cost surprises.
Legislation like the Prescription Drug Pricing Reduction Act could force PBMs to justify tier placements with clinical data. But that’s still years away.
For now, the system stays. And it’s designed to make you pay more for some generics-not because they’re worse, but because the company that makes them didn’t pay enough to the middleman.
Bottom Line
Your generic drug isn’t expensive because it’s special. It’s expensive because of a contract you never saw. A deal between a drugmaker and a PBM. A deal that doesn’t care if you can afford it.
But you can fight back. Know your plan. Ask questions. Compare options. Don’t assume “generic” means “cheap.” It doesn’t. And if you’re paying more than you should, you’re not alone. Millions are. But you’re the only one who can fix it-for yourself.

Suzan Wanjiru
November 22, 2025 AT 21:28My levothyroxine went from $8 to $42 last month and I didn’t even know why until I read this. Pharmacists swap generics all the time without telling you. I had to call my doctor three times to get the right one back. It’s ridiculous.
Jennifer Shannon
November 24, 2025 AT 02:30You know what’s wild? We treat medication like it’s a luxury brand-some generics are the ‘limited edition’ version you pay extra for because the company paid the middleman to put it on the shelf next to the ‘premium’ label. Meanwhile, the pills are chemically identical. It’s not healthcare-it’s consumer psychology engineered by insurance middlemen who’ve never held a pill in their hand. I’ve seen people skip doses because they thought their body ‘didn’t respond’ to the new generic-when really, they just got the cheaper version the PBM didn’t pay for. And then they blame themselves. That’s not a system failure. That’s a moral failure disguised as a business model.
Manjistha Roy
November 25, 2025 AT 09:22This is exactly why I always check my plan’s formulary before refilling. I used to assume ‘generic’ meant ‘cheap’ too. Now I know better. I keep a spreadsheet of my meds, their tiers, and the cash price from GoodRx. It’s saved me over $1,200 a year. No one taught us this stuff. We’re just supposed to trust the system. But the system doesn’t care if you’re tired, depressed, or broke. You have to be your own advocate.
Henrik Stacke
November 25, 2025 AT 22:50As someone who’s lived in both the UK and the US, I can tell you this: in Britain, we don’t have tiered copays. The NHS negotiates bulk prices, and everyone gets the same drug at the same cost. It’s not perfect, but at least you don’t have to become a pharmaceutical detective just to afford your thyroid pills. The American system isn’t broken-it was designed this way. And it’s designed to profit from your confusion.
Olanrewaju Jeph
November 26, 2025 AT 05:06My cousin in Lagos takes the same generic levothyroxine as I do, bought from a local pharmacy for $1.20 per month. No tier system. No PBM. No rebate negotiations. Just medicine. I wish we could export that model here. Instead, we’ve built a labyrinth where the only winners are the ones who never have to fill a prescription.
Richard Wöhrl
November 28, 2025 AT 01:20I work in pharmacy benefits and can confirm: 80% of tier changes are driven by rebate contracts, not clinical data. If a manufacturer stops paying the PBM enough, their drug gets moved up-even if it’s the exact same pill. Patients are collateral damage. And yes, some people do react differently to different fillers or binders in generics, but that’s rare. Most of the time, it’s just money.
Kezia Katherine Lewis
November 28, 2025 AT 13:46The terminology is deliberately obfuscating. ‘Preferred’ and ‘non-preferred’ sound like clinical judgments, but they’re purely financial. The term ‘specialty generic’ is especially misleading-it implies complexity where none exists. These are not biologics. They’re not novel. They’re just pills that didn’t pay the right bribe. We need new language. We need transparency. And we need to stop pretending this is about patient outcomes.
Adrian Rios
November 28, 2025 AT 17:16Let me tell you about my friend who stopped taking her generic adalimumab because the copay jumped from $25 to $1,100. She had a flare-up. Lost her job. Got hospitalized. The insurer didn’t care. The PBM didn’t care. The drugmaker didn’t care. The only person who cared was her sister, who paid for her meds out of pocket for six months. That’s not healthcare. That’s a moral crisis wrapped in a spreadsheet.
Pramod Kumar
November 28, 2025 AT 22:34I used to think generics were boring. Now I see them as the quiet revolutionaries of healthcare-identical pills, different prices, and the whole system rigged to make us feel guilty for wanting to afford our own medicine. I’ve started calling my meds by their manufacturer names instead of just ‘generic’-it helps me remember: this isn’t about science. It’s about who paid whom to win a game I didn’t even know I was playing.
Jennifer Skolney
November 29, 2025 AT 15:38I just used GoodRx and found out my $45 levothyroxine is $12 cash. I’m not paying $45. I’m not. I’m done. If I can buy it cheaper without insurance, why does insurance even exist for this? 🤦♀️
JD Mette
December 1, 2025 AT 05:18I’ve had this happen twice. I didn’t say anything because I didn’t know what to say. I just paid. It felt wrong, but I didn’t want to fight it. Reading this makes me feel less alone. Thanks.
Casper van Hoof
December 2, 2025 AT 03:18The tiered copay system is a logical extension of neoliberal healthcare logic: commodification of biological necessity, mediated by opaque third-party entities whose fiduciary duty lies not with the patient, but with the shareholder. The illusion of choice is maintained while the underlying structure remains unaltered. The patient, in this paradigm, becomes a consumer of risk, not a subject of care.
Lisa Lee
December 2, 2025 AT 16:10Why are we even talking about this? In Canada we just get the drug. No tiers. No drama. If you can’t afford it, you get help. Maybe if we stopped letting greedy American corporations run our system we wouldn’t have this mess. Just sayin’.
Bryson Carroll
December 4, 2025 AT 06:43People are so dumb they think a pill is a pill. Newsflash: fillers matter. And if you can’t afford your meds, maybe you shouldn’t be on them. The system isn’t broken. You’re just bad at budgeting.