Why Your Pain Reliever Might Be Worse Than You Think
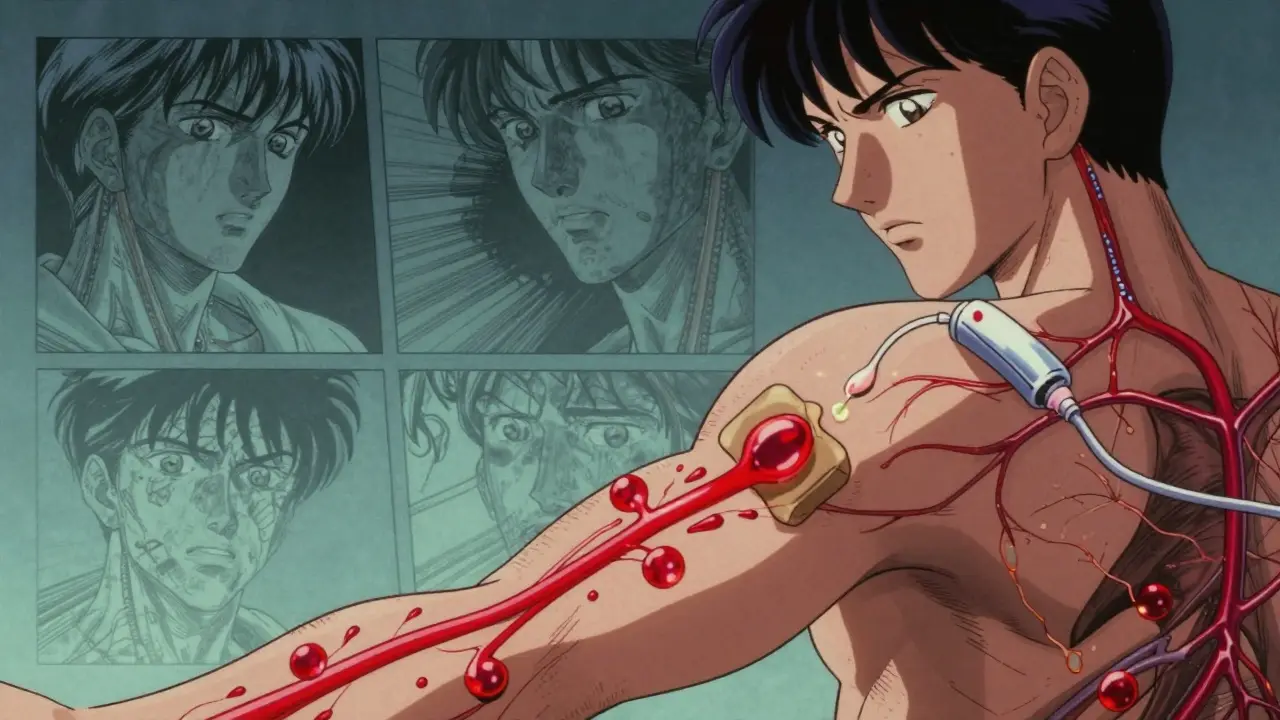
If you’ve ever taken an oral NSAID like ibuprofen or naproxen for back pain or arthritis, you’ve probably heard the warnings: stomach upset, ulcers, even internal bleeding. But what if you could get the same pain relief without risking your gut? That’s the promise of topical medications - creams, gels, and patches applied directly to the skin. The real difference isn’t just convenience. It’s systemic absorption - and that changes everything about safety.
Oral meds go down your throat, get absorbed in your intestines, then travel straight to your liver, where a big chunk gets destroyed before it even reaches your bloodstream. This is called first-pass metabolism. On average, 58.7% of oral drugs lose potency this way. For some, like morphine, it’s as high as 95%. What’s left enters your blood, circulates everywhere - your kidneys, your brain, your stomach lining - and that’s where the trouble starts.
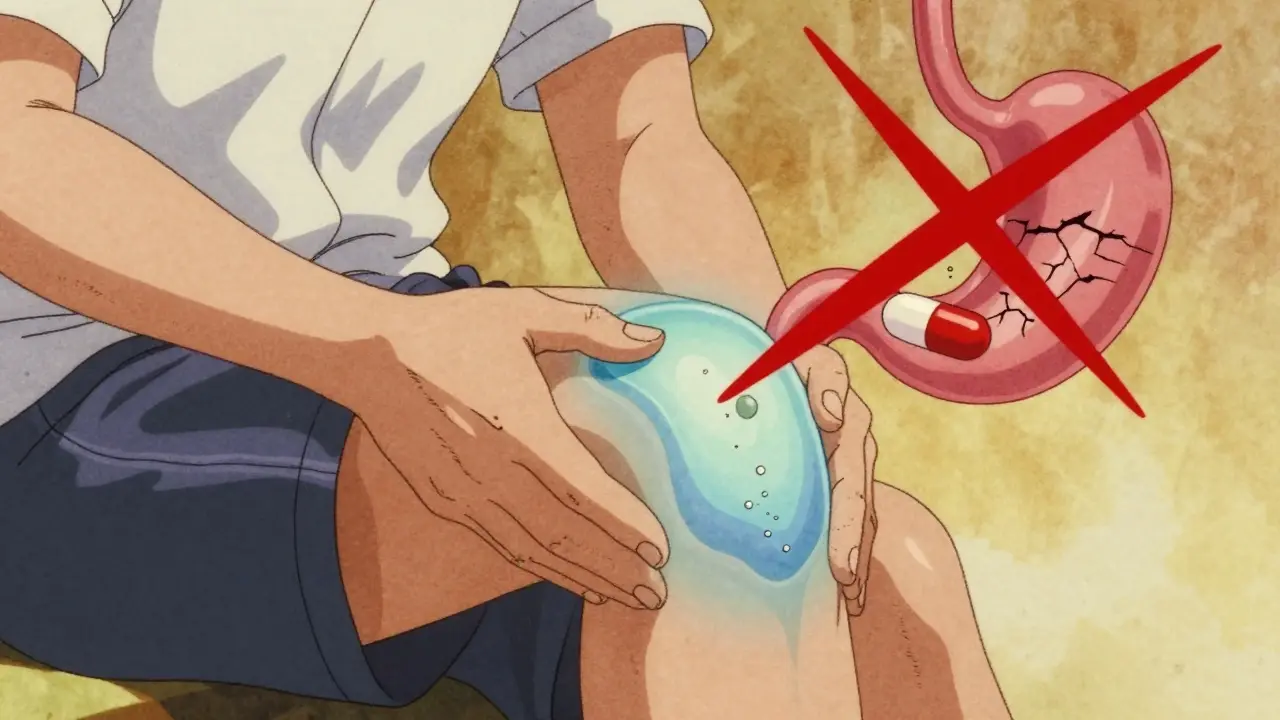
Topical meds? They’re designed to stay put. Applied to your knee, your shoulder, your lower back - they’re meant to work right where you hurt. Less than 5% of the drug typically enters your bloodstream. That’s why the FDA and the American College of Rheumatology now recommend topical NSAIDs as first-line treatment for localized pain. It’s not just safer. For many people, it’s just as effective.
How Much of the Drug Actually Gets Into Your Blood?
It’s easy to assume that if you rub something on your skin, it’s not doing anything inside your body. But that’s a dangerous myth.
Standard topical creams and gels - like Voltaren Gel or generic diclofenac - absorb through the top layers of skin. Studies show only 1% to 5% of the dose makes it into your bloodstream. Compare that to oral diclofenac, where 80-90% of the pill gets absorbed. That’s a 20-fold difference in systemic exposure.
But here’s the twist: transdermal patches are a different beast. These aren’t your average pain cream. They use chemicals to force drugs through the skin barrier. Fentanyl patches, for example, deliver 92% of the drug into your blood over three days. That’s why they’re used for chronic pain - and why they come with serious warnings. The difference between a topical gel and a transdermal patch is like comparing a drip to a hose.
Even with regular topical gels, absorption isn’t the same for everyone. Skin thickness, temperature, and even how much you apply matter. If you use too much - say, a whole tube on your back - or if your skin is cracked or inflamed, you can get systemic levels high enough to cause side effects. There are documented cases where patients using topical diclofenac on large areas ended up with plasma concentrations that matched those from oral doses. It’s not common, but it’s real.
Why Topical NSAIDs Are Safer - And When They’re Not
The safety gap between topical and oral NSAIDs is massive.
Oral NSAIDs cause about 15% of users to develop stomach problems - nausea, heartburn, ulcers. One in 10,000 people taking them will have a serious gastrointestinal bleed. That’s why older adults are told to avoid them. The American Geriatrics Society’s Beers Criteria says: skip oral NSAIDs for seniors. Use topical instead. Why? Because topical NSAIDs cut the risk of GI bleeding by 82%.
But topical isn’t perfect. About 10-15% of users get a skin reaction - redness, itching, rash. That’s the trade-off. It’s uncomfortable, but it’s not life-threatening. The FDA’s adverse event database shows 1.2 reports per 10,000 prescriptions for topical NSAIDs versus 14.7 for oral. That’s a 92% drop in serious incidents.
And here’s something most people don’t realize: topical NSAIDs can still reach your joints. Studies show muscle tissue under the application site gets drug concentrations equal to oral doses. Synovial fluid - the fluid inside your joints - gets some too, though the amount varies. That’s why they work for osteoarthritis. You’re not just numbing the surface. You’re treating the source.
But if your pain is in your hip or spine, or if it’s widespread, topical won’t cut it. Only 12% of the 200 most common prescription drugs can even be made into topical form. Why? Because molecules larger than 500 Daltons can’t pass through skin. That rules out most antibiotics, antidepressants, and heart meds. Topical is local. Oral is systemic. You pick based on where the problem lives.
Real People, Real Results: What Patients Say
Surveys tell us what studies can’t - how people actually feel.
In a 2023 survey of 2,417 people with osteoarthritis, 68% said topical NSAIDs gave them good to excellent pain relief. That’s slightly less than the 72% who said oral worked well. But here’s the kicker: 89% of those using topical meds preferred them. Why? Because 89% said they had fewer stomach problems. Only 42% of oral users said the same.
Reddit threads from the r/ChronicPain community are full of similar stories. One user wrote: “I used to take 800 mg of ibuprofen three times a day. My stomach was in constant pain. Switched to Voltaren gel - no more acid reflux, no more bloating. I just hate how sticky it is.” Another said: “It takes forever to work when it’s cold. I have to warm the gel in my hands first.”
And then there’s adherence. A 2023 study of 1,842 Medicare patients found that 37% more people stuck with topical meds than oral ones. Why? Because swallowing pills is hard if you’re elderly, have trouble swallowing, or just forget. A cream you rub on? You’re more likely to remember.
But here’s the flip side: 63% of people who stopped using topical meds said it just didn’t help enough. For severe pain - like a flare-up of rheumatoid arthritis or a herniated disc - topical alone isn’t enough. It’s a tool, not a cure-all.
How to Use Topical Meds Right - And Avoid Common Mistakes
Topical meds aren’t magic. If you use them wrong, they won’t work - or worse, they might hurt you.
The standard dose? A 4- to 6-inch ribbon of gel, applied to the painful area 3 to 4 times a day. That’s it. Most people under-dose. A 2023 survey of pharmacists found 41% of topical failures were due to using too little.
Also, don’t apply it to broken skin. Don’t cover it with a bandage unless the label says to. Heat helps absorption - so if you’re applying it in winter, warm the tube in your hands first. Skin works best above 89.6°F (32°C). Cold skin = slower absorption.
And wash your hands after applying - unless you’re treating your hands. Otherwise, you might accidentally rub the drug into your eyes or mouth. That’s how some people end up with stomach upset from a “topical” product.
Oral meds have their own pitfalls. Taking them with food can delay absorption by hours. Levothyroxine, for example, loses up to half its potency if taken with breakfast. And if you’re over 65? Avoid long-term oral NSAIDs entirely. The risk of kidney damage and heart events goes up fast.
What’s Next? The Future of Pain Relief
The market is shifting. The global topical drug market hit $52.3 billion in 2023 and is growing at 7.2% a year - faster than oral meds. Why? Because hospitals and insurers are seeing the savings. In 2023, 18,432 people were hospitalized for oral NSAID-related GI bleeding. Only 127 were for topical. That’s a 99% difference.
Insurance companies are catching on. Medicare Part D covers 82% of topical NSAID prescriptions, compared to 67% for oral. Out-of-pocket cost? Just $12.40 for topical versus $9.80 for generic oral. The price difference is tiny. The safety difference? Huge.
New tech is coming. Microneedle patches - tiny needles you stick on your skin - are in late-stage trials. They can deliver drugs that used to require pills. Imagine a patch for osteoporosis meds, or even insulin, without needles. Early results show 45% bioavailability - way higher than creams, but still safer than swallowing a pill.
By 2030, experts predict 35% of new pain drugs will be topical or transdermal. That’s up from 22% today. The American Pain Society says topical meds will become first-line treatment for 70% of localized pain conditions in the next decade.
But here’s the catch: 18-22% of people just don’t absorb enough through their skin. For them, topical won’t work. That’s why doctors still need to assess each patient - skin type, pain location, age, other meds - before deciding.
Bottom Line: Choose Based on Where the Pain Is
Oral meds are great when you need the drug to go everywhere - for full-body inflammation, infections, or chronic conditions like migraines or high blood pressure. But if your pain is in one spot - your knee, your elbow, your lower back - topical is the smarter choice.
It’s not about being “natural” or “milder.” It’s about precision. You’re not flooding your body with chemicals. You’re targeting the problem. That’s why doctors are changing their advice. That’s why insurance is covering it more. And that’s why, for millions of people, the next pain reliever they reach for won’t be a pill - it’ll be a tube of gel.
Just remember: apply the right amount, on the right skin, at the right time. And if it doesn’t help after a week? Talk to your doctor. Topical isn’t a magic fix - but for many, it’s the safest place to start.
Are topical pain creams as effective as oral NSAIDs?
For localized pain - like osteoarthritis in the knee or elbow - topical NSAIDs are just as effective as oral versions for most people. Clinical studies show pain relief rates between 18% and 92%, depending on the formulation and individual skin absorption. However, for widespread pain, deep joint pain, or systemic inflammation, oral meds are still more reliable. Topical doesn’t work well if the pain isn’t close to the skin surface.
Can topical NSAIDs cause stomach problems?
Rarely - and only if misused. Standard topical NSAIDs absorb less than 5% into the bloodstream, so they rarely cause stomach issues. But if you apply too much, use it on broken skin, or cover it with a tight bandage, systemic levels can rise enough to trigger nausea or ulcers. Cases of GI bleeding from topical use are extremely rare - about 1 in 100,000 users - compared to 1 in 10,000 for oral NSAIDs.
Why do some topical creams work faster than others?
It’s all about formulation. Gels with penetration enhancers - like Diclonate P - can deliver drug 3 times deeper than older versions. Liposomal creams trap the drug in tiny fat bubbles that fuse with skin cells, releasing it slowly. Hydrogels work fast but don’t penetrate deeply. The key isn’t just the drug - it’s how it’s packaged. Always check if the product is FDA-approved for systemic delivery; many OTC creams are just moisturizers with a little painkiller.
Is it safe to use topical NSAIDs every day?
Yes - for most people, daily use is safe if you follow the label. Topical NSAIDs are approved for up to 21 days of continuous use. Long-term use beyond that hasn’t been studied extensively, but data from users over 12 months show low rates of side effects. The real risk isn’t daily use - it’s using too much, applying to large areas, or combining with oral NSAIDs. Never use more than the recommended amount, even if pain persists.
Can children use topical NSAIDs?
Some topical NSAIDs are approved for kids 12 and older, but only for short-term use. Children have thinner skin and higher absorption rates, so they’re more sensitive to systemic effects. Always check the label. For younger kids, acetaminophen or ibuprofen in liquid form are safer choices. Never use adult-strength topical products on children unless directed by a doctor.
Do topical meds work better in warm weather?
Yes. Skin absorbs drugs more efficiently at temperatures above 89.6°F (32°C). In cold weather, blood flow to the skin drops, slowing absorption. That’s why some users report slower relief in winter. Warming the gel in your hands before application, or using a warm towel on the area, can help. Avoid heating pads directly on the cream - that can cause burns or increase absorption too much.
Why are topical NSAIDs more expensive than oral ones?
They’re not - at least not always. Generic oral NSAIDs like ibuprofen cost under $5 for 100 pills. But many topical NSAIDs are still brand-name, and their delivery systems (gels, patches, enhancers) cost more to produce. However, Medicare and private insurers often cover topical NSAIDs at similar or lower out-of-pocket costs than oral versions because they reduce hospitalizations. The $12.40 average cost for topical vs. $9.80 for oral is close, and the long-term savings in avoided GI complications make topical more cost-effective overall.
Can I use topical and oral NSAIDs together?
No - unless your doctor specifically says so. Combining them doubles your NSAID exposure and raises your risk of kidney damage, high blood pressure, and stomach bleeding. Even if the topical seems “weak,” it still adds to your total dose. If you’re taking oral NSAIDs and your pain isn’t controlled, talk to your doctor about switching - not stacking.

Herman Rousseau
December 22, 2025 AT 23:25Still hate how it smells though.
Nader Bsyouni
December 24, 2025 AT 22:10you think you're being smart but you're just paying more for less efficacy
the body is a system you can't cheat it with creams
Jeremy Hendriks
December 25, 2025 AT 22:21Ajay Brahmandam
December 27, 2025 AT 08:11jenny guachamboza
December 29, 2025 AT 03:23Aliyu Sani
December 29, 2025 AT 21:40Jim Brown
December 31, 2025 AT 20:22Vikrant Sura
January 2, 2026 AT 11:08Tarun Sharma
January 3, 2026 AT 08:33Kiranjit Kaur
January 4, 2026 AT 10:19Also, if you're cold, warm the tube in your pocket first. Game changer.
Gabriella da Silva Mendes
January 4, 2026 AT 10:53Johnnie R. Bailey
January 5, 2026 AT 00:28Sai Keerthan Reddy Proddatoori
January 6, 2026 AT 19:47