Quick Takeaways
- Venlafaxine is an SNRI commonly prescribed for depression and anxiety.
- Long‑term therapy can sustain mood stability but raises risks of cardiovascular strain, weight changes, and withdrawal symptoms.
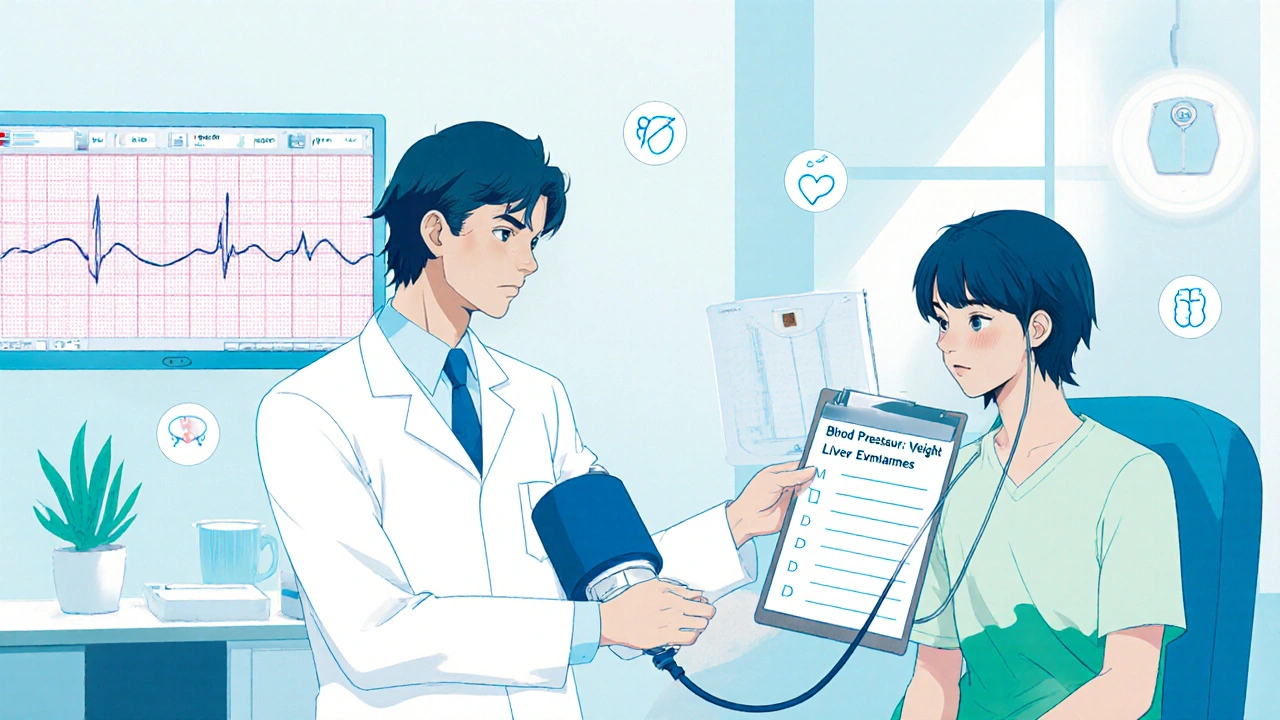
- Regular monitoring of blood pressure, heart rate, and liver enzymes helps catch problems early.
- Switching to an SSRI may be advisable if side effects become intolerable.
- Never stop the medication abruptly; taper slowly under medical supervision.
What Is Venlafaxine?
Venlafaxine is a serotonin‑norepinephrine reuptake inhibitor (SNRI) that boosts the levels of both serotonin and norepinephrine in the brain. It was first approved by the FDA in 1993 and quickly became a go‑to option for major depressive disorder (MDD) and generalized anxiety disorder (GAD).
By blocking the re‑uptake of two key neurotransmitters, Venlafaxine helps improve mood, energy, and anxiety control. The drug comes in immediate‑release tablets, extended‑release capsules, and a generic version that many insurers cover.
Why Consider Long‑Term Use?
Clinical guidelines suggest maintaining an antidepressant for at least six months after a patient achieves remission. For chronic conditions like recurrent depression or persistent anxiety, many clinicians keep patients on Venlafaxine for years. Long‑term therapy aims to:
- Prevent relapse or new episodes.
- Stabilise mood fluctuations that could impair work or relationships.
- Allow the brain to adapt to a steady neurotransmitter environment.
However, the decision to stay on the medication indefinitely hinges on weighing these benefits against possible downsides.
Potential Benefits of Staying on Venlafaxine
When the drug works well and side effects stay mild, the advantages can be substantial.
- Consistent symptom relief: Patients often report fewer depressive spikes and less anxiety during stressful life events.
- Improved functional outcomes: Better concentration, sleep, and social engagement.
- Reduced healthcare utilization: Fewer emergency visits and hospitalisations related to mental‑health crises.
- Flexibility of dosing: Lower doses (37.5‑75 mg) may suffice for anxiety, while higher doses (150‑225 mg) target severe depression.
Risks and Downsides of Long‑Term Venlafaxine
Extended exposure brings a handful of safety signals that clinicians keep an eye on.
Cardiovascular Concerns
Cardiovascular risk includes elevated blood pressure and heart‑rate variability. Studies show that doses above 150 mg can raise systolic pressure by 3‑5 mmHg on average. For patients with hypertension, regular BP checks are essential.
Weight and Metabolic Changes
Weight gain of 2‑5 kg over a year is reported in up to 15 % of long‑term users, while another 10 % experience modest weight loss. Metabolic panels should be reviewed annually.
Sexual Dysfunction
Sexual dysfunction covers reduced libido, delayed orgasm, and erectile difficulties. The incidence rises with higher doses and can hurt relationship satisfaction.
Withdrawal and Discontinuation Syndrome
Withdrawal syndrome may include dizziness, flu‑like symptoms, irritability, and electric‑shock sensations if the medication is stopped too quickly. Even tapering over two‑four weeks might not prevent mild symptoms in sensitive individuals.
Drug Interactions and Metabolism
Venlafaxine is metabolised primarily by the liver enzyme CYP2D6. Concomitant use of strong CYP2D6 inhibitors (e.g., fluoxetine, paroxetine) can increase plasma levels, raising the chance of side effects.
Other Possible Issues
- Sleep disturbances, especially at doses above 150 mg.
- Potential increase in suicidal thoughts during the first few weeks of treatment, a warning that applies to most antidepressants.
- Rare but serious conditions such as serotonin syndrome when combined with other serotonergic drugs.
How to Monitor and Manage Long‑Term Use
Effective monitoring turns many of these risks into manageable items.
- Blood pressure: Check at baseline, then every 2‑4 weeks for the first 3 months, and every 6‑12 months thereafter.
- Weight and BMI: Record at each visit; advise on diet and exercise if upward trend appears.
- Heart rate & ECG: Consider an ECG for patients with a history of arrhythmia or when doses exceed 225 mg.
- Liver function tests: Annual panels are standard, more often if liver disease is present.
- Side‑effect questionnaire: Use tools like the UKU Side Effect Rating Scale to capture subtle changes.
If any parameter crosses a safety threshold, clinicians may lower the dose, switch to an SSRI, or add adjunctive therapy (e.g., low‑dose aripiprazole for residual depression).
Venlafaxine Versus Other Antidepressants for Long‑Term Therapy
| Feature | Venlafaxine (SNRI) | Sertraline (SSRI) | Escitalopram (SSRI) |
|---|---|---|---|
| Primary neurotransmitters affected | Serotonin & norepinephrine | Serotonin only | Serotonin only |
| Typical dose for depression | 150‑225 mg/day | 50‑200 mg/day | 10‑20 mg/day |
| BP impact (high doses) | +3‑5 mmHg systolic | None | None |
| Weight change (12 mo) | ±2‑5 kg (mixed) | ±1‑3 kg (gain fav.) | ±1‑2 kg (gain fav.) |
| Sexual dysfunction incidence | 15‑20 % | 10‑15 % | 8‑12 % |
| Withdrawal severity (if stopped abruptly) | Moderate‑severe | Mild‑moderate | Mild‑moderate |
| Common drug interactions | CYP2D6 inhibitors | CYP3A4 inhibitors | CYP2C19 inhibitors |
The table shows that Venlafaxine offers broader neurotransmitter coverage, which can translate into stronger antidepressant effects for some patients. The trade‑off is higher blood‑pressure impact and a tougher withdrawal profile. SSRIs like sertraline and escitalopram are gentler on the cardio system and easier to stop but sometimes fall short in severe depressive episodes.
Real‑World Perspective: Patient Stories
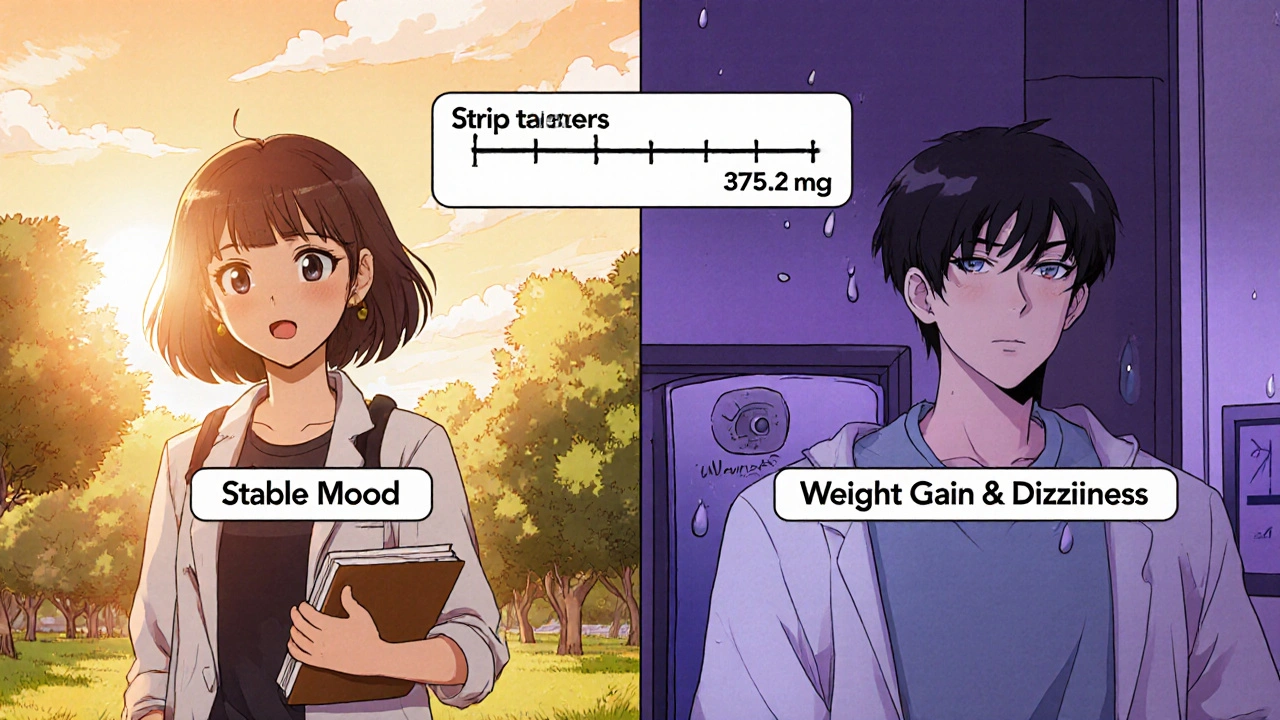
Emma, a 34‑year‑old graphic designer from Melbourne, began Venlafaxine 150 mg after two failed SSRI trials. After six months, her depressive scores dropped from 28 to 9 on the PHQ‑9. She continued the medication for three years, reporting stable mood and only mild dry mouth. Annual BP checks stayed under 130/80 mmHg, so her doctor kept the dose steady.
John, 58, started Venlafaxine for GAD. After 18 months he noticed persistent dizziness and a 6 kg weight gain. His physician tapered him to sertraline, which resolved the dizziness and halted weight gain, though his anxiety required a modest dose increase.
These anecdotes underline that individual response varies; regular check‑ups let patients and clinicians fine‑tune therapy.
Frequently Asked Questions
Can I take Venlovaxine forever?
There’s no hard deadline, but doctors usually reassess the need every 12‑18 months. If you’ve been stable for years and side effects are minimal, continuing may be reasonable.
What blood‑pressure level should worry me?
A consistent reading above 140/90 mmHg warrants a dose review or a switch to a medication with less impact on BP.
How do I taper Venlafaxine safely?
Typical tapers reduce the dose by 37.5 mg every 1‑2 weeks for extended‑release capsules. Your prescriber may stretch the schedule if you experience withdrawal symptoms.
Is Venlafaxine safe during pregnancy?
Data are mixed. Some studies link early‑trimester exposure to a slight increase in cardiac defects. Discuss risks vs. benefits with your obstetrician before deciding.
Will Venlafaxine affect my cholesterol?
No direct effect, but weight changes can indirectly alter lipid panels. Annual lipid screening is a good habit regardless of medication.
Bottom Line
Venlafaxine can be a powerful ally for people battling chronic depression or anxiety, especially when other drugs fall short. The upside-steady mood control-must be balanced against possible cardiovascular, metabolic, and withdrawal issues. Ongoing monitoring, dose adjustments, and open dialogue with a prescriber are the keys to staying on the drug safely for the long haul.


Shannon Stoneburgh
October 24, 2025 AT 20:04The article overstates the benefits and downplays the risks.
Nathan Comstock
October 26, 2025 AT 21:04Listen, anyone who thinks Venlafaxine is a miracle cure clearly hasn't read the fine print – it's a powerful drug with real side‑effects, and you can't just ignore blood‑pressure spikes, weight gain, or the nasty withdrawal storms that hit when you quit too fast. If you want a quick fix, you’ve got the wrong guide; you need discipline, regular check‑ups, and a doc who actually cares about the numbers, not just the mood scores.
Corrine Johnson
October 28, 2025 AT 23:04Ah, the paradox of modern psychopharmacology, wherein the pursuit of stability collides with the specter of physiological compromise, and thus we find ourselves navigating a labyrinth of dosage titrations, blood‑pressure monitoring, and the ever‑present dread of an electric‑shock withdrawal; indeed, the very mechanisms that lift us from the abyss of depression also tether us to a cascade of metabolic and cardiovascular considerations, demanding a balance as delicate as a tightrope walk across a canyon of uncertainty.
Jennifer Stubbs
October 31, 2025 AT 01:04From a clinical standpoint, the data on long‑term Venlafaxine use shows a clear trade‑off: you get solid mood control for many patients, but you also have to keep an eye on blood pressure, weight, and the withdrawal profile. The key is regular monitoring – labs, vitals, and honest symptom check‑lists – so you can catch any drift early. If side‑effects become burdensome, a dose tweak or a switch to an SSRI is a reasonable next step.
Tamara Tioran-Harrison
November 2, 2025 AT 03:04Well, isn’t that just splendid? One would assume that a "helpful" analysis would also advise the reader to actually schedule those BP checks, rather than merely gloss over them. Your summary feels rather like a polite pamphlet with the vigor of a bureaucratic memo – quite the masterpiece of understatement, I must say. :)
Abby W
November 4, 2025 AT 05:04Hey, no offense, but you kinda missed the point about the real‑world hassle of getting those appointments 🤷♀️. I’ve been on Venlafaxine for years and the clinic’s calendar is a nightmare – you end up juggling work, kids, and the occasional panic attack while waiting for a slot. Anyone else feel like the system sets us up to fail? 🙈
Veronica Appleton
November 6, 2025 AT 07:04If you’re thinking about staying on Venlafaxine long‑term, the best approach is a partnership with your prescriber: schedule regular BP checks, keep a simple log of weight changes, and discuss any new symptoms right away. Most people find that a steady dose works well when side‑effects stay mild, and taper plans can be customized to avoid withdrawal headaches.
ram kumar
November 8, 2025 AT 09:04Ah, the naïve optimism of “just keep a log” – as if a spreadsheet can replace nuanced clinical judgment. One must acknowledge that the very act of chronic dosing invites a cascade of metabolic and cardiovascular shifts, rendering any simplistic self‑monitoring woefully inadequate. Yet, of course, this is the kind of shallow advice that populates every wellness blog.
Deborah Galloway
November 10, 2025 AT 11:04I hear you, and it can definitely feel overwhelming when you’re juggling medication, appointments, and daily life. First, remember that you’re not alone – many people on Venlafaxine share similar concerns, and talking to a supportive community can make a big difference. Second, set up a simple routine: pick a day each week to check your blood pressure at home, even if it’s just the quick cuff you bought from the pharmacy. Third, keep a brief journal – a line or two each day about how you feel, any new symptoms, or changes in mood. Fourth, schedule a quarterly appointment with your prescriber specifically to review those numbers and discuss any side‑effects you’ve noticed. Fifth, don’t hesitate to bring up weight changes; a nutritionist or a simple diet tweak can often help manage modest gains. Sixth, if you notice any sexual side‑effects, let your doctor know right away – there are often adjustments or supplemental strategies that can help. Seventh, be proactive about withdrawal: if you ever need to stop, ask for a taper plan that gently lowers the dose over weeks or months, depending on how you respond. Eighth, stay informed about drug interactions – a quick check on any new medication with your pharmacist can prevent unexpected spikes in blood levels. Ninth, remember that mental health isn’t static; it’s okay to reassess the need for medication every year or so, especially if you feel stable. Tenth, practice self‑care: regular sleep, balanced nutrition, and light exercise can boost the overall effectiveness of your treatment. Eleventh, reach out to a therapist if you experience lingering anxiety or depressive thoughts – therapy often works well alongside medication. Twelfth, keep an open line with your doctor – honesty about side‑effects builds trust and leads to better care. Thirteenth, celebrate small victories – a day with stable mood or a good night’s sleep is worth noting. Fourteenth, if you ever feel your blood pressure climbing above 140/90, schedule an earlier check‑up; early intervention is key. Finally, know that adjusting or switching medications is a normal part of the journey; it doesn’t mean failure, just that you and your doctor are fine‑tuning the approach to keep you thriving.