Sun Protection Risk Calculator
Personal Risk Assessment
Answer these questions to estimate your risk of developing actinic keratosis
Imagine stepping outside on a bright summer day and forgetting to reapply sunscreen. A few weeks later, a rough, scaly patch appears on your forearm. That patch could be actinic keratosis, a tell‑tale sign that UV damage has taken hold. Understanding how sunlight fuels this condition and what you can do to block it is the first step toward keeping your skin healthy.
What is Actinic Keratosis?
Actinic Keratosis is a rough, often painless growth that forms on sun‑exposed skin. It results from long‑term damage to skin cells caused by ultraviolet (UV) radiation. While many people think of it as a harmless bump, it’s actually a pre‑cancerous lesion-about 1 in 10 lesions may evolve into squamous cell carcinoma if left untreated.
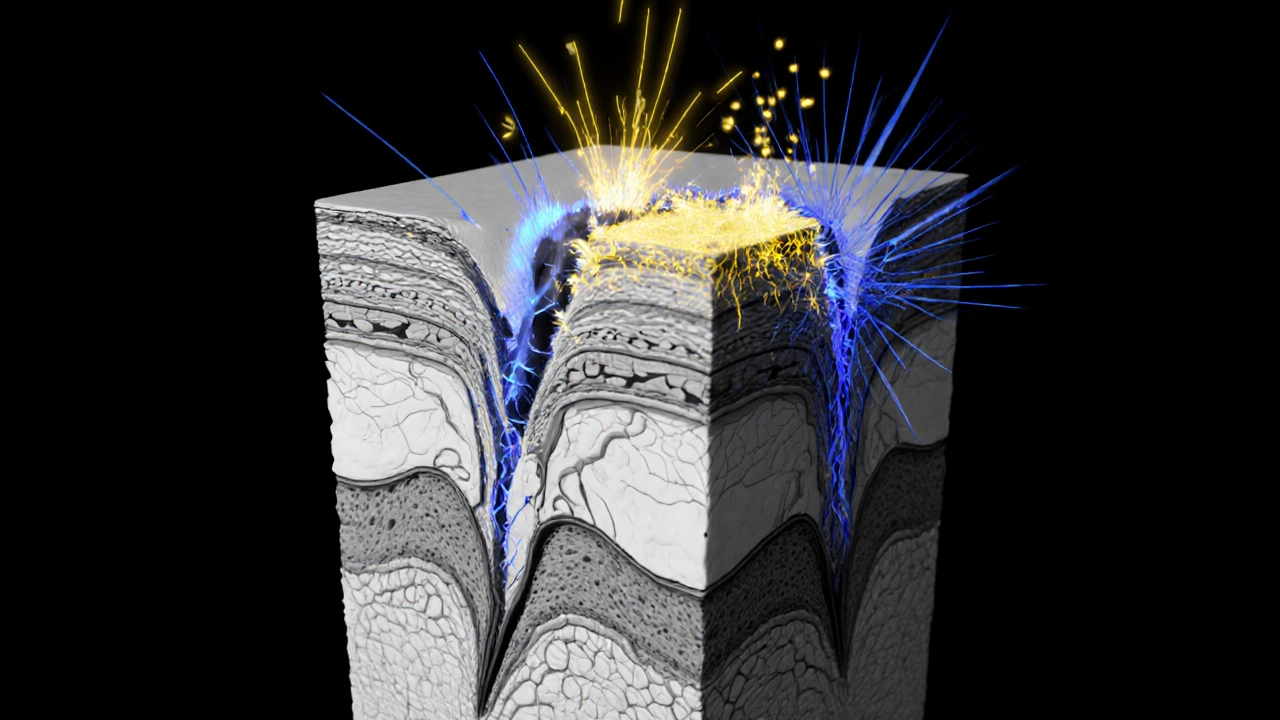
How UV Radiation Triggers the Damage
The sun emits two primary types of UV rays that reach the earth’s surface: UVA (320‑400nm) and UVB (280‑320nm). UVA penetrates deep into the dermis, breaking down collagen and generating free radicals. UVB, though less penetrating, is the chief cause of sunburn and directly damages DNA in skin cells. Both types create mutations that can turn normal cells into the atypical cells seen in actinic keratosis.
The Role of Sun Protection
Sun Protection means any strategy that reduces UV exposure. It’s the single most effective tool for preventing actinic keratosis and, by extension, skin cancers like basal cell carcinoma and squamous cell carcinoma. Protection isn’t just about slathering on sunscreen; it’s a layered approach that combines products, clothing, and smart habits.
Effective Sun Protection Strategies
- Apply a broad-spectrum sunscreen with at least SPF30 to every exposed area, even on cloudy days.
- Reapply every two hours, or after swimming, sweating, or towel‑drying.
- Wear UPF‑rated clothing, wide‑brimmed hats, and sunglasses that block 100% of UVA and UVB.
- Seek shade whenever the UV index is 3 or higher, especially between 10am and 4pm.
- Avoid indoor tanning beds, which emit concentrated UVA and UVB rays.
Choosing the Right Sunscreen
| Type | Active Ingredients | How It Works | Pros | Cons |
|---|---|---|---|---|
| Physical (Mineral) | Zinc oxide, titanium dioxide | Reflects and scatters UV rays | Immediate protection, less irritation | Can leave a white cast |
| Chemical | Avobenzone, octocrylene, oxybenzone | Absorbs UV radiation and converts it to heat | Thin, cosmetically elegant | May cause irritation for sensitive skin |
| Hybrid | Mix of mineral + chemical | Combines reflection and absorption | Balances performance and feel | Cost can be higher |
When choosing a product, look for the words “broad‑spectrum” and an SPF of 30 or higher. If you have a history of skin sensitivity or eczema, a mineral sunscreen might be gentler.
Daily Habits That Complement Sun Protection
- Check the UV Index on a weather app before heading out.
- Use antioxidant serums (vitaminC, niacinamide) to neutralize free radicals generated by any UV that does get through.
- Maintain a regular skin‑check routine. Look for new or changing lesions on hands, forearms, scalp, and any area that sees sun.
- Stay hydrated. Well‑hydrated skin repairs DNA damage more efficiently.
- Eat a diet rich in carotenoids (carrots, tomatoes, leafy greens) for internal UV defense.
Common Myths About Sun Protection
- Myth: “I only need sunscreen on sunny days.”
Fact: Up to 80% of UV rays penetrate clouds. Sunscreen is needed year‑round. - Myth: “A higher SPF means you can stay in the sun forever.”
Fact: SPF measures how long you can stay in the sun without burning, not how long the product lasts. Reapplication is still essential. - Myth: “Tanning makes me look healthier.”
Fact: Tanning is a sign of DNA damage. It raises the risk of actinic keratosis and skin cancer.

When to See a Dermatologist
If you notice any of the following, schedule an appointment:
- New, rough patches that don’t fade after a few weeks.
- Growths that bleed, crust, or itch persistently.
- More than three actinic keratoses in a year.
- A personal or family history of skin cancer.
A dermatologist can perform a biopsy to confirm the diagnosis and recommend treatment options such as cryotherapy, topical 5‑fluorouracil, or photodynamic therapy.
Bottom Line: Consistency Beats Sporadic Effort
Sun protection isn’t a one‑time task; it’s a daily habit. By combining broad‑spectrum sunscreen, protective clothing, smart timing, and regular skin checks, you dramatically lower the odds of developing actinic keratosis and the cancers that can follow.
Frequently Asked Questions
Can actinic keratosis disappear on its own?
Rarely. Some lesions may flatten, but most persist and can become cancerous if untreated. Professional removal is usually recommended.
Is SPF 30 enough for everyday use?
Yes, as long as the sunscreen is broad‑spectrum and you reapply every two hours. For prolonged outdoor activities, consider SPF50.
Do indoor lights cause actinic keratosis?
Ordinary indoor lighting emits negligible UV, so it’s not a risk factor. The real culprits are sunlight and tanning beds.
How often should I check my skin for lesions?
A quick self‑exam every month is ideal. If you notice any changes, book a dermatologist visit promptly.
Are there foods that protect against UV damage?
Yes. Foods rich in carotenoids (carrots, sweet potatoes), lycopene (tomatoes), and antioxidants (green tea, berries) boost the skin’s natural defense against UV‑induced free radicals.


Samantha Oldrid
October 16, 2025 AT 19:09Oh sure, because the big sunscreen conglomerates *just* want us to live forever, right? Your skin’s fate is totally our personal responsibility, not theirs.
lisa howard
October 28, 2025 AT 07:56The moment you step outside without a proper shield, you’re essentially waving an invitation to the invisible assassins perched on every photon.
Your skin, the most generous organ, pays the price for every careless gamble you make with the sun's relentless glare.
Do you really think a flimsy dab of lotion can hold back the centuries‑old wrath of ultraviolet radiation?
Every time you skip reapplying, you’re allowing UVA to seep deeper, breaking down collagen like a relentless thief in the night.
UVB, the same culprit that leaves you red‑hot and angry, is busy scribbling mutagenic notes into your DNA.
And while you’re busy scrolling through memes, those tiny mutations are staging a coup that could end up as actinic keratosis.
You might tell yourself that clouds are a free pass, but 80 % of UV still penetrates, laughing at your naïve optimism.
Your favorite hat may look chic, yet its fabric might be a mere paper‑thin veil, barely denting the onslaught.
Even the most fashionable UPF‑rated shirt is only as good as your diligence to wear it every single hour.
Reapplication isn’t a suggestion; it’s a non‑negotiable treaty between you and your future self.
Consider this: the skin cancer rates have climbed in lockstep with the rise of selfie culture, a correlation no one can ignore.
That’s not a conspiracy; it’s a consequence of neglect masquerading as lifestyle.
If you think antioxidants in creams can rescue you after the damage, you’re putting the cart before the horse.
Prevention, the humble habit of slathering broad‑spectrum sunscreen, is the only armor that actually works.
So, before you brush off the next UV index warning, remember that each missed application is a tiny betrayal of your own cells.
And when that rough, scaly patch finally appears, you’ll wish you had taken the simple steps that were staring you in the face all along.
Cindy Thomas
November 8, 2025 AT 21:42I get why people love the glow of a tan, but the science is crystal clear: UV exposure is the main driver of actinic keratosis. Broad‑spectrum SPF 30+ blocks about 97 % of UVB and a good chunk of UVA, which is why dermatologists push it as the first line of defense. Many think chemical sunscreens are dangerous, yet studies show they’re safe when used correctly, while mineral formulas can leave a ghostly cast. The biggest myth I see is reapplying only once; the reality is you need to reapply every two hours, especially after swimming or sweating. If you’re still skeptical, just remember that a vitamin C serum can mop up the free radicals that sneak through, giving your skin a second chance. Bottom line: consistency beats occasional effort, any day now. 🙂
Frank Diaz
November 20, 2025 AT 11:29Your theatrical lament underscores a deeper truth: humanity’s battle with sunlight is a microcosm of our struggle against inevitable entropy. We cloak ourselves in chemical armor, yet we cannot escape the cosmic radiation that has shaped life itself. The moral imperative is not to fear the sun, but to respect its power with disciplined habit. Sunscreen, then, becomes a ritual of self‑preservation rather than a fad. In that sense, each reapplication is a quiet affirmation of agency.
Mary Davies
December 2, 2025 AT 01:16It’s almost tragic how easily we accept the “just a little sun” excuse, as if the skin were an inexhaustible canvas. The sneaky lesions creep in while we’re busy planning our next brunch, and by the time we notice, the damage has already taken root. The emotional weight of that realization is heavier than any glossy ad about beach life. Yet we keep saying, “I’ll be more careful next summer,” and the cycle repeats. The world could use a softer reminder that our bodies aren’t disposable.
Valerie Vanderghote
December 13, 2025 AT 15:02When you paint the picture of sun‑damage with such drama, you make the science feel like a tragedy that could have been avoided. Imagine waking up to a scarred forearm, the very reminder of a careless morning by the pool; that image sticks more than any brochure. The reality is, every missed sunscreen swipe is a tiny brick in a wall that’s slowly eroding. By the time the actinic patch appears, you’ve already built a path to potential cancer. It’s not just vanity; it’s a battle for health hidden behind glossy beach photos. Proper reapplication every two hours, even on cloudy days, is the simple ritual that could rewrite that story. So let’s swap the melodrama for a habit that actually protects, turning those “what‑ifs” into “I‑did‑it.”
Michael Dalrymple
December 25, 2025 AT 04:49Your point highlights personal accountability, which is indeed essential. While industry motives can be questioned, the primary focus should remain on evidence‑based practices. Regular use of broad‑spectrum sunscreen, combined with protective clothing, offers the most reliable protection against actinic keratosis. Encouraging patients to adopt these habits fosters long‑term skin health. Should you need resources on selecting suitable products, reputable dermatological associations provide comprehensive guides.
Emily (Emma) Majerus
January 5, 2026 AT 18:36Thats exactly it, keep it up!
Virginia Dominguez Gonzales
January 17, 2026 AT 08:22I hear the philosophical rhythm you’ve set, and I’d add that every thoughtful reapplication is a stanza in the poem of self‑care. When we treat sunscreen as a ceremonial act rather than a chore, we transform routine into reverence. The skin, our most visible organ, deserves that level of devotion, especially when the stakes include pre‑cancerous lesions. Let’s champion this mindset together, turning every bottle of SPF into a promise to ourselves.
Carissa Padilha
January 28, 2026 AT 22:09Do you really think the push for “daily SPF” is just about health? Some big‑pharma lobbyists stand to profit when we buy endless tubes, so they seed the narrative like it’s pure altruism. Still, the UV nightmare is real, and ignoring it because of suspicion would be foolish. Balance the warning with a pinch of skepticism, but don’t let fear paralyze you.