AGEP Symptom Assessment Tool
This tool helps you assess whether your symptoms match clinical criteria for Acute Generalized Exanthematous Pustulosis (AGEP). It is NOT a medical diagnosis. If you have symptoms, consult a healthcare professional immediately.
AGEP is not just a rash. It’s a sudden, violent skin reaction triggered by a medication-often one you’ve taken without a second thought. Within 48 hours of taking a common antibiotic like amoxicillin-clavulanate, your skin can erupt with hundreds of tiny, pus-filled bumps. Fever spikes. Your body feels like it’s fighting an infection. But there’s no bacteria. No virus. Just your immune system overreacting to a drug. And if you don’t recognize it fast, you could end up in the hospital.
What AGEP Actually Looks Like
Imagine your skin turning bright red, then being covered in pinhead-sized white dots-each one a sterile pustule. These aren’t acne. They don’t come from clogged pores. They form deep in the top layer of skin, not around hair follicles. The rash usually starts in warm, moist areas: under the arms, in the groin, or on the face. Within a day or two, it spreads everywhere. You might feel burning, not just itching. Your lips or mouth could feel raw. Your tongue might swell.
Unlike psoriasis, AGEP rarely affects the palms or soles. It doesn’t have the thick, scaly plaques you’d see in chronic skin conditions. The pustules are shallow, fragile, and don’t last long. Within a week, they dry up and peel off like sunburned skin. That’s the hallmark: rapid rise, rapid fade. But the speed is what makes it dangerous. If you mistake it for a regular allergy or infection, you keep taking the drug-and the rash gets worse.
What Causes AGEP?
Nearly every case is linked to a medication. Antibiotics are the #1 culprit. About 56% of AGEP cases come from beta-lactams like amoxicillin, ampicillin, or penicillin-especially when combined with clavulanate. Macrolides like erythromycin and azithromycin are next. Then come antifungals like terbinafine, and even common heart meds like calcium channel blockers (diltiazem, amlodipine).
Here’s the twist: sometimes the drug that triggers AGEP isn’t the one you think. A patient might take amoxicillin for a sore throat, then get sick a week later. They switch to ibuprofen for fever. A few days after that, the rash appears. The real trigger? The amoxicillin. It lingers in your system. The reaction can show up as late as 14 days after the last dose.
And yes, even steroids can cause it. There are documented cases where patients developed AGEP after taking prednisolone. But here’s the odd part: the same patients sometimes tolerate methylprednisolone just fine. That’s why guessing the trigger isn’t always easy. It’s not about the drug class alone-it’s about your body’s unique response.
How Doctors Diagnose It
There’s no single blood test for AGEP. Diagnosis is clinical-and it’s tricky. In community clinics, up to 40% of cases are misdiagnosed as psoriasis, folliculitis, or even chickenpox. Dermatologists use a mix of signs:
- Rash onset within 1-5 days (median 2 days) after starting a new drug
- Thousands of non-follicular pustules on red skin
- Fever above 38°C
- High white blood cell count, mostly neutrophils
- Elevated CRP (a marker of inflammation)
A skin biopsy confirms it. Under the microscope, you’ll see neutrophils piled up just below the skin’s surface, with little damage to the deeper layers. That’s different from pustular psoriasis, where the inflammation goes deeper and lasts longer. The EuroSCAR group created a diagnostic tool called the AGEP Probability Score (APS). It’s 94% accurate when used by trained clinicians. But most ER doctors don’t have access to it. That’s why many patients get sent home with antihistamines-only to return days later, sicker.

What Happens If You Don’t Stop the Drug?
AGEP is self-limiting. That means, if you stop the drug, it will go away on its own-in about 10 to 14 days. But that doesn’t mean you should wait. The longer you keep taking the trigger, the worse it gets. Skin can break down. Fluids leak. You risk infection. Fever spikes. Your kidneys or lungs might start to struggle.
Hospitalization is recommended if:
- Your fever is above 38.5°C
- More than 20% of your skin is covered
- You’re dehydrated or confused
- Your white blood cell count is extremely high
Average hospital stays range from 6 to 9 days. Without proper care, mortality can climb to 4%. That’s low compared to Stevens-Johnson Syndrome (which kills up to 10%), but still serious. And recovery isn’t quick. The peeling phase lasts weeks. Your skin will be sensitive. Sun exposure can darken the patches permanently. You need moisturizers, gentle cleansers, and strict sun protection.
The Treatment Debate: Steroids or Not?
This is where things get messy. Some doctors swear by steroids. Others say they’re unnecessary-and risky.
The standard advice: stop the drug. That’s non-negotiable. Then, supportive care: cool compresses, antihistamines for itching, moisturizers, and fluids. That’s enough for most people.
But here’s the conflict:
- U.S. experts (Dermatology Advisor, 2021) say: avoid oral steroids. AGEP resolves on its own. Steroids mask symptoms, increase infection risk, and don’t improve long-term outcomes.
- European experts (Journal of the European Academy of Dermatology, 2023) say: use steroids if the rash covers more than 20% of your body or you’re very sick. Their study showed 87% of steroid-treated patients cleared in 7 days-compared to 63% without.
Studies show steroids can cut hospital stays by over 3 days. But they also raise blood sugar, weaken immunity, and can cause mood swings. So the decision isn’t just medical-it’s personal. If you’re diabetic, elderly, or immunocompromised, steroids might be too risky. If you’re a healthy 30-year-old with 40% skin coverage and a 102°F fever? The benefit may outweigh the risk.
New Hope: Biologics for Refractory Cases
What if the rash doesn’t budge? What if steroids aren’t an option? That’s where biologics come in.
Secukinumab-a drug used for psoriasis and arthritis-blocks IL-17, a key inflammation driver in AGEP. In a 2021 case report, a patient with AGEP who couldn’t take steroids got one shot of secukinumab. Within 72 hours, the pustules vanished. No infection. No side effects. Another patient saw improvement in just 48 hours.
It’s not FDA-approved for AGEP yet. But clinical trials are underway. Early results show 92% response rates in small groups. Other biologics targeting IL-23 are also being tested. This isn’t science fiction. It’s the next frontier. For patients who don’t respond to standard care, biologics might become the new standard.
What You Should Do If You Suspect AGEP
Here’s what to do right now:
- Stop taking any new medication you started in the last two weeks-even if you think it’s harmless.
- Don’t pop the pustules. Don’t scrub your skin. Don’t use hot water.
- Call your doctor or go to urgent care. Say: “I think I might have AGEP.” Mention every drug you’ve taken in the past 14 days.
- If you have fever, confusion, or trouble breathing, go to the ER immediately.
- Keep a list of all medications. Bring it with you. Include supplements, herbal products, and over-the-counter pills.
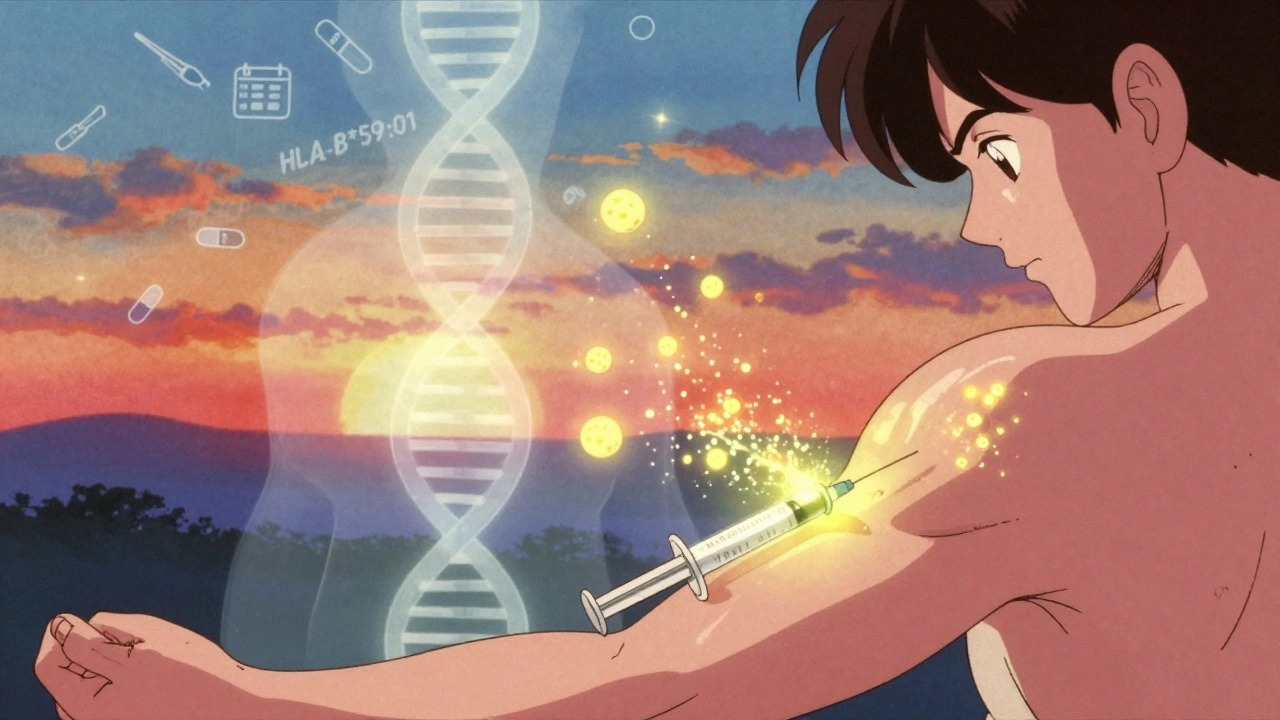
After recovery, get tested for drug allergies. You’ll need to avoid the trigger forever. And if you’re on long-term meds, ask your doctor about genetic testing. A gene called HLA-B*59:01 increases your risk of AGEP-especially if you’re Asian. Not everyone needs this test. But if you’ve had one reaction, it could save your life next time.
What’s Changing in 2025?
Pharmaceutical companies are now required to monitor for AGEP in clinical trials. The FDA and EMA updated their guidelines in 2022 and 2023. New drug labels now list AGEP as a possible side effect for antibiotics, antifungals, and even some blood pressure pills.
Doctors are getting better at spotting it. The AGEP Probability Score is being rolled out in major hospitals. And research is moving fast. By 2026, we may have a simple blood test to predict who’s at risk before they even take a drug.
For now, the message is simple: if your skin breaks out suddenly after a new medication, don’t ignore it. Don’t assume it’s just an allergy. AGEP is rare-but it’s real. And it’s fast. The sooner you act, the safer you’ll be.


Lynette Myles
December 4, 2025 AT 05:25Stop taking antibiotics. That’s it. That’s the whole post. Why are we wasting time on biologics when the solution is literally just stop the drug? The FDA knows this. Doctors know this. But they keep prescribing like it’s candy.
Annie Grajewski
December 5, 2025 AT 10:30so like… is this just the body’s way of saying ‘bro u took amoxicillin AGAIN??’ like i get it, your immune system’s like a toddler throwing a tantrum because you gave it sugar before dinner. but why do we treat it like a medical emergency instead of just… not being dumb? also, steroids? really? you’re gonna give a human body more fire when it’s already on fire?? 🤡
Harry Nguyen
December 6, 2025 AT 02:44Europeans want steroids? Of course they do. They think medicine is a buffet and you can just pile on whatever feels good. In America, we treat the body like a machine that needs to fix itself-not a garden you spray with chemicals. This is why our mortality rates are lower. We don’t coddle the immune system. We let it fight.
Philip Kristy Wijaya
December 6, 2025 AT 16:57It is a curious phenomenon that the human organism exhibits such an extreme and rapid hypersensitivity response to xenobiotic compounds particularly those of beta lactam origin yet the medical establishment persists in promoting these agents as first line therapy without adequate pre screening protocols or genetic risk stratification this is not medicine this is industrial pharmaceutical gambling with human physiology as the wager
Jennifer Patrician
December 7, 2025 AT 12:05They’re hiding something. AGEP isn’t random. It’s linked to vaccines. Look at the timing-people get antibiotics, sure, but they also get boosters. The same cytokine storm pattern. The same pustules. The same ‘it’s just an allergy’ dismissal. Why won’t the CDC admit this? Why do they call it ‘drug-induced’ when the real trigger is the same stuff they’re injecting into kids? They’re scared of the truth.
Mellissa Landrum
December 9, 2025 AT 01:32my cousin got this after taking some cheap azithromycin from a mexican pharmacy. they told her it was ‘heat rash’ for three days. she ended up in the ER with a 103 fever and her skin peeling like a snake. now she’s scared of every pill she sees. i swear if you go to a doctor now they just hand you a scrip like you’re ordering coffee. no questions asked. wake up people.
luke newton
December 10, 2025 AT 19:35I’ve seen this happen to my brother. He took amoxicillin for a sinus infection. Two days later, he was in the ER. They gave him steroids. He got better. But now he’s on insulin because of it. You think you’re saving skin but you’re breaking metabolism. This isn’t treatment. It’s trading one disaster for another. And the doctors? They just shrug. They don’t care about the long game.
Ali Bradshaw
December 11, 2025 AT 08:21This is such a vital post. I’ve been a nurse for 18 years and I’ve seen too many patients dismissed as having ‘allergic hives’ when it’s actually AGEP. The key is timing and persistence. If you’ve started a new med in the last two weeks and your skin is angry-trust your gut. Don’t wait for a biopsy. Go back. Push. You’re not overreacting. You’re saving your life.
an mo
December 12, 2025 AT 13:16Biologics are the only rational pathway forward. IL-17 inhibition directly targets the neutrophilic cascade that defines AGEP pathophysiology. The current standard of care is reactive and antiquated. Steroids are a blunt instrument with systemic immunosuppressive consequences. Biologics offer precision. The data is clear. The infrastructure is lagging. We need real-time pharmacovigilance pipelines and HLA-B*59:01 screening integrated into EHRs before prescribing any beta-lactam. This isn’t future medicine. It’s ethical necessity.
aditya dixit
December 14, 2025 AT 10:10In India, we don’t have access to biologics or even proper dermatologists in most towns. But we do have something better: community wisdom. Grandmothers know when a rash isn’t just an allergy. They say: stop the medicine. Let the body rest. Drink neem water. Don’t scratch. In villages, AGEP heals faster because no one gives steroids. No one panics. Maybe the answer isn’t more science-but less interference. Let the body do what it was made to do.