Medication Weight Change Calculator
Estimate potential weight changes from medications you're taking. Based on clinical data showing average weight changes over 6 months.
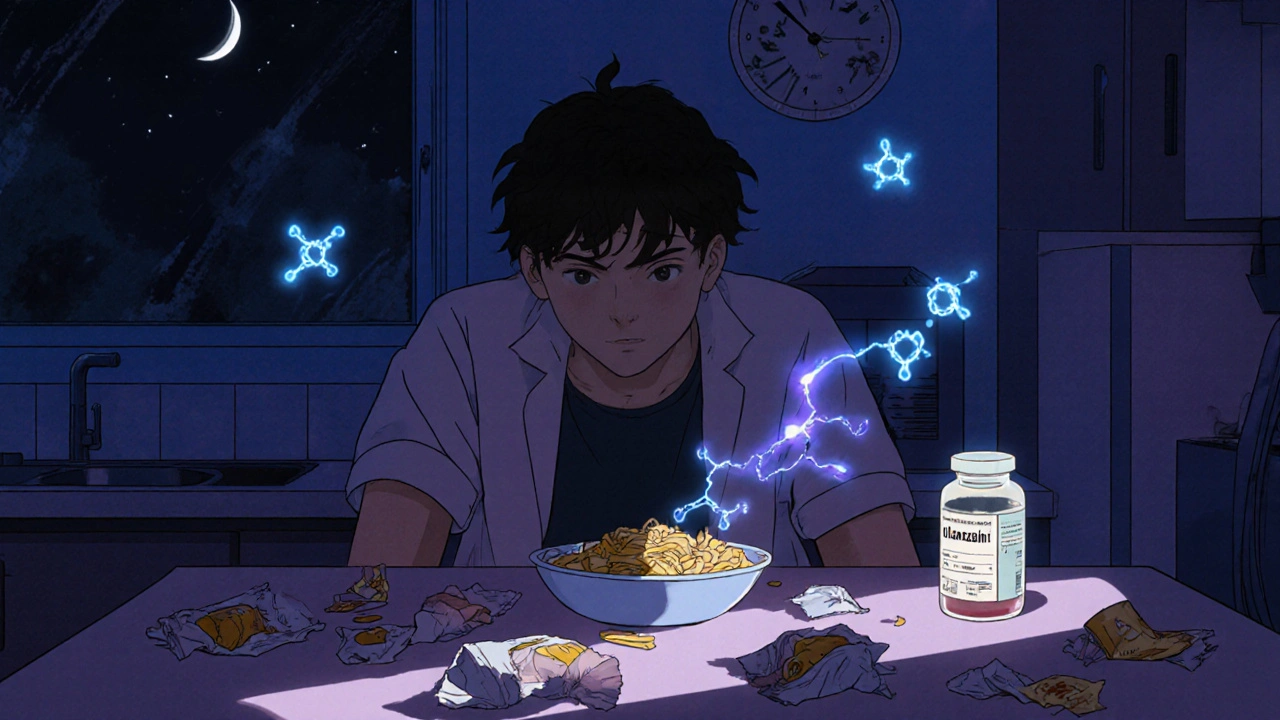
Many people start a new medication expecting relief from pain, anxiety, or depression-but end up dealing with something they didn’t sign up for: constant hunger or no appetite at all. It’s not just in your head. Medications can directly alter how your body signals hunger, processes food, and stores energy. And if you’re one of the millions affected, you’re not alone. About 40% of U.S. adults live with obesity, and medications are responsible for 15-20% of those cases. Whether you’re gaining weight on an antidepressant or losing your appetite on a stimulant, these changes are real, measurable, and manageable-with the right approach.
Why Do Medications Change Your Appetite?
It all starts in your brain. Your appetite isn’t controlled by willpower-it’s regulated by chemicals called neurotransmitters. Serotonin, dopamine, histamine, and others send signals to your hypothalamus, the part of your brain that tells you when to eat and when to stop. Many medications interfere with these signals. For example, antipsychotics like olanzapine and risperidone boost ghrelin, the hormone that makes you feel hungry. Studies show ghrelin levels can rise by 15-20% within just four weeks of starting these drugs. That’s why so many people on these medications report feeling hungry all the time-even after eating. Antidepressants work differently. In the first few weeks, SSRIs like sertraline or fluoxetine might suppress appetite because they increase serotonin, which makes you feel full faster. But after six to twelve months, your brain adapts. Serotonin receptors become less sensitive, and suddenly, you crave carbs. That’s when weight gain starts creeping in. Meanwhile, drugs like mirtazapine directly block histamine receptors, which triggers intense hunger. Up to 40% of people taking mirtazapine gain more than 7% of their body weight in just six months. On the flip side, stimulants like amphetamines and drugs like topiramate reduce appetite by boosting norepinephrine and dopamine. These drugs can cut daily calorie intake by 300-500 calories. That’s why some people lose weight on ADHD meds or seizure drugs-even when they’re not trying. Even diabetes medications aren’t immune. Insulin helps your body store glucose as fat, which often leads to 2-4 kg of weight gain in the first six months. Metformin does the opposite: it helps you lose 2-3 kg by improving insulin sensitivity and reducing cravings.Which Medications Are Most Likely to Cause Appetite Changes?
Not all drugs affect appetite the same way. Some are notorious for weight gain, others for weight loss. Here’s a breakdown based on clinical data:| Medication Class | Examples | Typical Appetite Effect | Average Weight Change (6 Months) |
|---|---|---|---|
| Second-generation antipsychotics | Olanzapine, Risperidone, Quetiapine | Strong increase | +4 to +10 kg |
| Antidepressants | Mirtazapine, Amitriptyline, Paroxetine | Increase | +2 to +5 kg |
| Antidepressants (low-risk) | Bupropion, Vortioxetine | Neutral or decrease | -1 to +0.5 kg |
| Diabetes meds | Insulin, Sulfonylureas | Increase | +2 to +4 kg |
| Diabetes meds (weight-neutral) | Metformin, GLP-1 agonists | Decrease | -2 to -5 kg |
| Stimulants | Amphetamine, Methylphenidate | Decrease | -1 to -3 kg |
| Antihistamines | Diphenhydramine, Hydroxyzine | Mild increase | +1 to +2 kg |
| Weight-loss drugs | Topiramate, Orlistat | Strong decrease | -3 to -5 kg |
Notice how mirtazapine and olanzapine top the list for weight gain, while bupropion and metformin are among the few that help you lose or stay steady. If you’re starting a new medication, knowing this list can help you and your doctor make smarter choices.
When Do These Changes Happen?
Appetite changes don’t happen overnight-but they don’t take years either. Most weight gain from medications happens fast, especially in the first three to six months. For antipsychotics like olanzapine, the biggest jump in weight occurs within the first 10 weeks. That’s why experts like Dr. David Brendel from Harvard Medical School recommend weighing yourself weekly during the first three months. Catching a 2-3 kg gain early gives you time to act before it becomes a 10 kg problem. Antidepressants follow a different timeline. In the first month, you might feel less hungry. But by month six, cravings for bread, pasta, and sweets often kick in. This is because your brain adjusts to the drug’s effect on serotonin. It’s not laziness-it’s biology. Even medications you wouldn’t expect, like beta-blockers or antihistamines, can cause slow, steady weight gain over time. A 1-2 kg gain might seem small, but over a year, it adds up. And if you’re already overweight, even a small increase can raise your risk for diabetes, high blood pressure, or heart disease.
How to Manage Appetite Changes-Without Stopping Your Medication
The good news? You don’t have to choose between mental health and your waistline. There are proven ways to manage these side effects while staying on your medication. 1. Eat protein-rich snacks every 3-4 hours. A snack with 15-20 grams of protein-like Greek yogurt, hard-boiled eggs, or a handful of nuts-keeps your blood sugar stable. That cuts down on hunger spikes by up to 40%. This is especially helpful if you’re on a drug that causes carb cravings. 2. Swap refined carbs for whole grains. White bread and sugary snacks spike your blood sugar, then crash it. That makes you hungrier sooner. Whole grains like oats, quinoa, and brown rice digest slower. People who make this switch report feeling full 45 minutes longer after meals. 3. Drink water before meals. A simple trick: drink two glasses of water 20 minutes before eating. In a study of 200 users, this reduced calorie intake by 13% on average. It’s not magic-it’s just filling your stomach so you eat less. 4. Meal prep twice a week. When you’re hungry and tired, you grab whatever’s handy. That’s how chips and cookies end up in your cart. Planning meals ahead reduces impulsive eating by 35%. One study found people who prepped meals ate 200 fewer calories per day than those who didn’t. 5. Move your body, even a little. Resistance training-like lifting weights or doing bodyweight exercises-builds muscle. Just 2-3 sessions a week can raise your metabolism by 50-100 calories per day. That’s like burning an extra apple every day. You don’t need to run marathons. Just move consistently. 6. Practice mindful eating. Eat without distractions. Put your phone away. Chew slowly. Notice how your food tastes and feels. People who do this reduce portion sizes by 15-20% without feeling deprived.When to Talk to Your Doctor
Never stop or change your medication on your own. Abruptly stopping antipsychotics or antidepressants can cause withdrawal, rebound symptoms, or even dangerous health risks. But you should talk to your doctor if:- You’ve gained more than 5% of your body weight in six months
- Your appetite changes are affecting your mood or self-esteem
- You’re developing symptoms of diabetes-like increased thirst, frequent urination, or fatigue
- You’re losing weight unintentionally and it’s causing weakness or dizziness

What About Genetic Testing?
There’s emerging science that might make this even easier. A 2023 study in Nature Medicine identified 12 genetic markers linked to higher risk of weight gain from antipsychotics. In the future, doctors might test your DNA before prescribing certain drugs-so you avoid ones that are likely to cause problems. Right now, that’s still experimental. But if you’re struggling with weight gain and have tried everything, ask your doctor if genetic testing or pharmacogenomics is an option in your area. It’s not standard yet, but it’s coming.Real People, Real Results
One Reddit user shared how he gained 30 pounds on quetiapine in four months. He felt hopeless-until he started meal prepping, drinking water before meals, and adding two 20-minute walks a day. Over six months, he lost 22 pounds. He stayed on his medication. He didn’t quit. He just changed his habits. Another woman switched from mirtazapine to bupropion. She lost 15 pounds in six months and said her depression didn’t get worse. She felt like herself again-not just a person who couldn’t stop eating. These aren’t outliers. They’re examples of what’s possible when you combine medical awareness with practical, daily changes.Final Thoughts: You’re Not Broken
Appetite changes from medication aren’t your fault. They’re a side effect-not a failure. You didn’t lose control. Your brain chemistry did. The key is to act early, stay informed, and work with your doctor. Don’t wait until you’ve gained 20 pounds to say something. Don’t feel ashamed if you’re struggling. Millions are. And there are tools, strategies, and newer medications that can help you feel better-without sacrificing your health. Start small. Pick one habit to change this week. Drink more water. Add one protein snack. Walk for 10 minutes. Progress isn’t about big leaps. It’s about consistent steps-ones that keep you on your medication, on your path, and in control of your life.Can antidepressants cause weight gain even if I eat the same amount?
Yes. Some antidepressants, like mirtazapine and paroxetine, slow your metabolism and increase cravings for carbs-even if your food intake doesn’t change. This happens because they alter serotonin and histamine pathways in your brain, which affects how your body stores fat and signals hunger. You might not eat more, but your body holds onto calories differently.
Is it safe to switch medications to avoid weight gain?
It can be, but only under medical supervision. Switching medications too quickly can cause withdrawal symptoms, mood crashes, or even seizures in rare cases. Most psychiatric drugs need to be tapered over 2-4 weeks. Your doctor can help you transition to a weight-neutral alternative like bupropion, vortioxetine, or metformin, depending on your condition and history.
Do all antipsychotics cause weight gain?
No. First-generation antipsychotics like haloperidol cause less weight gain than second-generation ones like olanzapine or quetiapine. Newer options like aripiprazole and lurasidone are considered weight-neutral in most patients. If weight gain is a concern, ask your doctor about switching to a lower-risk option.
Can exercise reverse medication-induced weight gain?
Exercise alone won’t fully reverse it-but it helps significantly. Resistance training builds muscle, which raises your resting metabolism by 50-100 calories per day. Combined with dietary changes, it can prevent further gain and help you lose 1-2 kg per month. The key is consistency, not intensity. Even walking 30 minutes a day makes a difference.
Why do I feel hungrier at night on my medication?
Many medications, especially antipsychotics and antidepressants, disrupt your circadian rhythm and ghrelin levels. Ghrelin-the hunger hormone-peaks at night in people on these drugs. Add in stress, boredom, or poor sleep, and nighttime cravings become overwhelming. Eating protein-rich snacks earlier in the day and avoiding screens before bed can help reset your hunger signals.
Are there any supplements that help with medication-related appetite changes?
No supplement has been proven to reliably block medication-induced appetite changes. Some people report benefits from fiber supplements or chromium, but studies are small and inconsistent. The most effective strategies are behavioral: eating protein, meal prepping, and managing stress. Always talk to your doctor before taking supplements-they can interact with your medication.

Conor McNamara
November 17, 2025 AT 15:46so uhh... did u know that Big Pharma secretly adds sugar to antidepressants to make us fat? i mean, why else would everyone gain weight but the docs stay skinny? they got a deal with the food industry. i saw a video on a forum once. they even put tracking chips in the pills. i’m not crazy, i just read the fine print.
steffi walsh
November 18, 2025 AT 06:18you’re not alone!! 🥺 i was on mirtazapine and went from size 8 to 14 in 5 months. i felt like a monster. then i started drinking water before meals and adding hard-boiled eggs to my snacks. lost 12 lbs without quitting my med. you got this. 💪
Leilani O'Neill
November 19, 2025 AT 09:44How quaint. The average person doesn’t have the discipline to manage their own biology. You’re not ‘affected by medication’-you’re just lazy. If you ate like a civilized human being and stopped gulping down processed carbs, you wouldn’t need a 2000-word essay on why your body betrayed you.
Riohlo (Or Rio) Marie
November 20, 2025 AT 18:17Oh honey, you think this is about ghrelin? Please. This is capitalism’s finest weapon: make you dependent on drugs that make you crave Doritos, then sell you keto meal kits at $30 a pop. The real villain isn’t olanzapine-it’s the $87 billion weight-loss industrial complex that profits from your shame. I’ve seen the leaked emails. They call us ‘metabolic sheep.’
Louie Amour
November 21, 2025 AT 05:31Stop being so dramatic. I’ve been on 3 different SSRIs and never gained a pound. You just don’t have willpower. Eat less. Move more. That’s it. No magic. No conspiracy. Just basic human responsibility. If you can’t control your eating, maybe you shouldn’t be on meds at all.
Kristina Williams
November 22, 2025 AT 13:57they're putting fluoride in the water and the meds to make us docile. i read a guy on 4chan who said his cousin's neighbor's dog got fat after the new water plant opened. same week his sister started on sertraline. coincidence? i think not.
Shilpi Tiwari
November 24, 2025 AT 11:08Interesting neuropharmacological modulation of the hypothalamic-pituitary-adrenal axis via serotonergic and histaminergic receptor downregulation. The adipokine dysregulation observed in patients on second-gen antipsychotics correlates with elevated NPY expression. However, the clinical efficacy of protein-snacking protocols remains underpowered in RCTs-n=200 is insufficient. Need larger longitudinal studies with DEXA scans.
Christine Eslinger
November 24, 2025 AT 16:23Thank you for writing this. I’ve been on olanzapine for 3 years and felt so guilty about the weight gain-like I was failing at life. But reading this? It’s not me. It’s the medicine. And the tips? Water before meals, protein snacks, walking after dinner-I’ve done all three. Lost 18 lbs in 6 months. I didn’t quit. I didn’t give up. I just learned how to work with my body, not against it. You’re not broken. You’re adapting. And that’s brave.
Denny Sucipto
November 25, 2025 AT 13:48man. i was on topiramate for seizures and lost 20 lbs in 4 months. couldn’t even eat a slice of pizza without feeling sick. then i switched to gabapentin and gained it all back. felt like i lost myself. but then i started meal prepping with my mom on Sundays. now i eat like a human again. not perfect. but better. you’re not alone. we’re all just trying to survive our own bodies.