When your asthma flares up every spring, or after you clean the house, or when your cat jumps on your lap-it’s not just bad luck. It’s likely your allergies are feeding the fire in your lungs. This is the asthma-allergy overlap, and it affects more than half of all asthma patients. It’s not a separate disease. It’s the hidden driver behind why so many people struggle to control their asthma, even with inhalers.
Why Allergies Make Asthma Worse
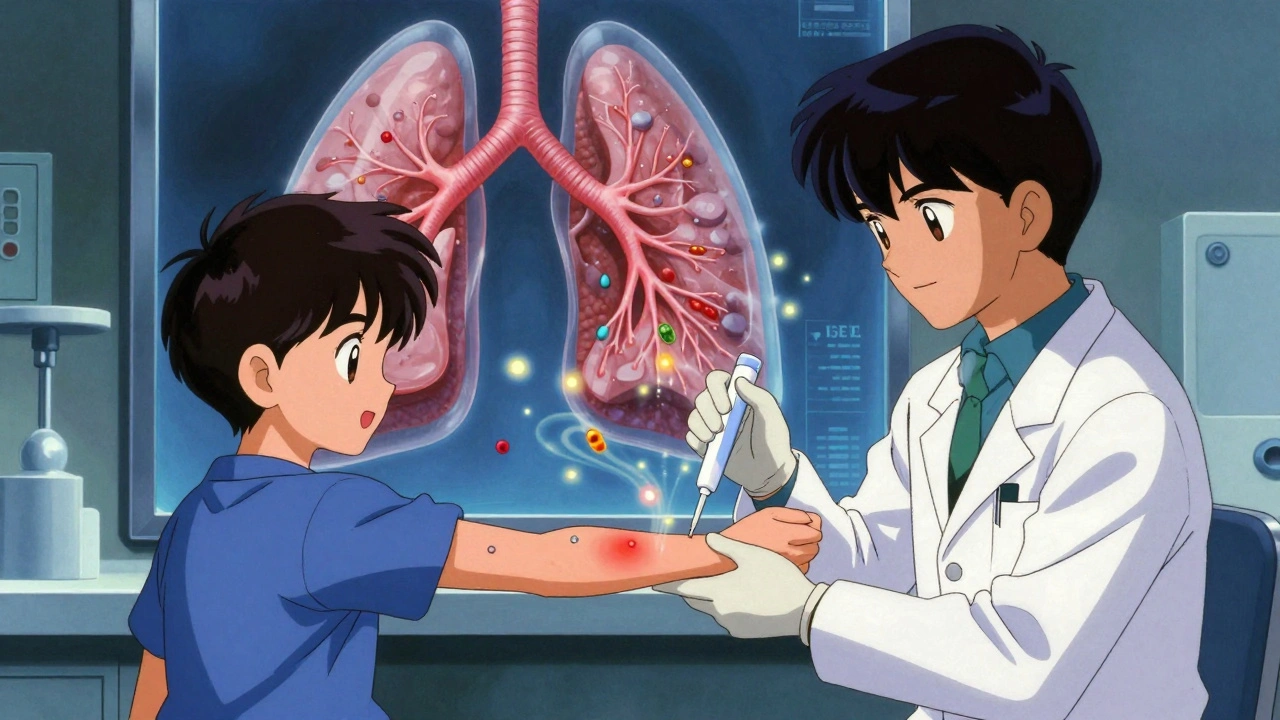
Think of your airways like a garden. In healthy lungs, things stay calm. But in allergic asthma, your immune system mistakes harmless things-like pollen, dust mites, or pet dander-for invaders. It launches an IgE-mediated attack, flooding your airways with inflammatory cells, especially eosinophils and mast cells. These cells release histamine, leukotrienes, and other chemicals that cause swelling, mucus, and tightening of the muscles around your bronchial tubes. The result? Wheezing, coughing, chest tightness, and shortness of breath.
The pattern is well-documented. Around 60% of adults and 80% of children with asthma have allergic triggers, according to the American College of Allergy, Asthma, and Immunology. Many start with eczema as babies, then develop allergic rhinitis, and eventually asthma-the so-called "allergic march." This isn’t random. It’s a progression of immune dysfunction that starts at the skin and mucous membranes and moves into the lungs.
How to Know If You Have Allergic Asthma
If your asthma gets worse during certain seasons, after being around pets, or in dusty rooms, that’s a red flag. But symptoms alone aren’t enough. You need confirmation.
The gold standard is skin prick testing. A tiny amount of allergen is placed on your skin, then lightly pricked. If you’re allergic, a small bump and redness appear within 15-20 minutes. Blood tests for specific IgE antibodies are also reliable, especially if skin testing isn’t possible. These tests aren’t just for diagnosis-they’re your roadmap for treatment.
Doctors also look at lung function. Spirometry showing reversible airflow obstruction (improvement after using a rescue inhaler) plus positive allergy tests = allergic asthma. Blood eosinophil counts above 300 cells/μL and elevated FeNO (fractional exhaled nitric oxide) levels further confirm the allergic, eosinophilic type of inflammation. These biomarkers help predict who will respond best to certain treatments.
What Works: The Four Pillars of Management
Managing this overlap isn’t about treating asthma alone. You have to tackle the allergy side too. There are four proven strategies:
- Allergen avoidance-This sounds simple, but it’s often the most overlooked. Dust mites live in bedding, carpets, and upholstered furniture. Use allergen-proof mattress and pillow covers. Wash bedding weekly in hot water (at least 130°F). Vacuum with a HEPA-filter vacuum at least twice a week. Keep pets out of the bedroom. Close windows during high pollen season. These steps take effort, but studies show they reduce rescue inhaler use by up to 50% when done consistently.
- Inhaled corticosteroids (ICS)-These are the foundation of asthma control. People with allergic asthma respond better to ICS than those without allergies. About 60-70% achieve good control with daily use. Don’t skip doses-even when you feel fine. The inflammation doesn’t disappear just because symptoms do.
- Allergen immunotherapy-This is the only treatment that can change the course of the disease. Whether through weekly shots or daily under-the-tongue tablets, immunotherapy trains your immune system to tolerate allergens. Cochrane reviews show a 40-60% reduction in asthma symptoms and medication use over time. It takes 3-5 years to see full benefits, and the first few months can be frustrating. But patients who stick with it cut their annual asthma costs by about $1,200 and often reduce or eliminate daily inhalers.
- Biologic therapies-For severe cases that don’t respond to standard treatment, biologics target specific parts of the immune response. Omalizumab (Xolair) blocks IgE. Dupilumab (Dupixent) blocks IL-4 and IL-13. Tezepelumab (Tezspire), approved in 2021, works even if you’re not allergic. These drugs reduce exacerbations by 50% or more. They’re expensive-$25,000-$35,000 a year-but for the right patient, they can mean the difference between hospital visits and living normally.
Real People, Real Results
One woman in Ohio stopped needing her rescue inhaler four times a week after removing her cat from her bedroom. Another man in Texas cut his steroid inhaler dose in half after two years of allergy shots for dust mites. On patient forums, 68% of those who identified their triggers reported major improvements.
But it’s not always easy. Many struggle with insurance coverage. Comprehensive allergy testing can cost $250-$400 out of pocket. Immunotherapy requires weekly visits for months, then monthly for years. Some patients quit because the results aren’t immediate. One Reddit user wrote: "I did shots for 8 months and felt worse. I gave up. Then I tried again a year later-and it worked. I wish I’d known to stick with it."
That’s the catch. Immunotherapy and biologics aren’t quick fixes. They’re long-term investments in your lung health.
What Doesn’t Work (and Why)
Not all asthma is allergic. If your asthma started in your 40s after a respiratory infection, or you have no history of eczema or hay fever, your triggers might be cold air, exercise, or stress-not pollen or pet dander. In these cases, allergy testing won’t help, and immunotherapy won’t work.
Also, some doctors still don’t test for allergies. A 2022 survey found only 35% of primary care doctors routinely screen asthma patients, compared to 65% of allergists. That’s a gap. If your asthma isn’t improving, ask: "Could allergies be making this worse? Can I get tested?"
And while allergen avoidance helps, it’s not perfect. Pollen forecasts are only 70-80% accurate. HEPA filters reduce dust mites by 85%-but only if you use them weekly. Most people stop after a month. Consistency is everything.

What’s New in 2025
The field is moving fast. The 2023 GINA guidelines now classify asthma by "endotype"-not just symptoms. That means treatment is becoming more precise. Blood tests for eosinophils and FeNO are now standard for guiding therapy.
Tezepelumab (Tezspire) is a game-changer because it works for both allergic and non-allergic severe asthma. And new research shows combining dupilumab with immunotherapy boosts results by 75% compared to either alone. Multi-allergen tablets-targeting five allergens at once-are in phase 3 trials and could replace multiple single-allergen shots.
But access remains unequal. In low-income countries, 75% of asthma patients can’t get basic allergy testing. Even in the U.S., insurance hurdles delay care. The good news? The global allergy diagnostics market is growing fast, and more health systems are making testing mandatory for uncontrolled asthma.
What You Can Do Today
If you have asthma and your symptoms flare with seasons, pets, or cleaning:
- Ask your doctor for allergy testing. Don’t wait for a crisis.
- Start allergen-proofing your bedroom. Covers, hot washes, HEPA vacuum.
- Track your symptoms and triggers in a journal. Note the date, weather, pets, and activities.
- Use a pollen app like Allergy Alert for hyperlocal forecasts.
- If you’re on daily inhalers and still having symptoms, ask about biologics or immunotherapy.
Managing asthma-allergy overlap isn’t about finding one magic solution. It’s about connecting the dots between your environment and your lungs. The more you understand your triggers, the more control you have. And that’s the real goal-not just fewer symptoms, but fewer limits on your life.
Is allergic asthma the same as regular asthma?
No. Allergic asthma is triggered by allergens like pollen, dust mites, or pet dander, and involves IgE-driven inflammation. Regular (non-allergic) asthma can be triggered by cold air, exercise, stress, or infections, and doesn’t involve the same immune pathway. About 60% of adults with asthma have the allergic type, but the treatment approach differs. Allergic asthma responds better to inhaled steroids and allergy-targeted therapies like immunotherapy.
Can allergy shots cure asthma?
No, but they can change how your body reacts to allergens over time. Allergen immunotherapy doesn’t cure asthma, but it reduces airway inflammation caused by allergies. Many patients see a 40-60% drop in symptoms and medication use after 3-5 years. Some stop needing daily inhalers. It’s the closest thing to a disease-modifying treatment we have for allergic asthma.
How long does it take for allergy immunotherapy to work?
It’s a slow process. You’ll start with weekly shots or daily tablets for 3-6 months (build-up phase), then move to monthly maintenance for 3-5 years. Most people notice improvement after 6-12 months, but full benefits take 2-3 years. Many quit too early because they don’t see instant results. The key is sticking with it-the long-term payoff is real.
Are biologics worth the cost?
For severe allergic asthma that doesn’t respond to standard treatment, yes. Biologics like omalizumab or dupilumab reduce exacerbations by 50% or more. That means fewer ER visits, hospital stays, and missed workdays. While they cost $25,000-$35,000 a year, many insurance plans cover them if you meet criteria (like high eosinophil count or frequent attacks). For the right patient, the cost is offset by avoided care.
Can I outgrow allergic asthma?
Some children do, especially if their allergies are mild and well-managed. But for many, allergic asthma persists into adulthood. The immune system doesn’t forget allergens-it just becomes less reactive over time with proper management. Avoiding triggers and using immunotherapy can help reduce severity, but stopping treatment without medical advice often leads to return of symptoms.
Do I need to see an allergist, or can my primary doctor handle this?
Your primary doctor can start treatment with inhalers and basic advice. But if your asthma is uncontrolled, seasonal, or linked to known allergies, you need an allergist. They’re trained in allergy testing, immunotherapy, and biologics. Only 35% of primary care doctors routinely test asthma patients for allergies-so if you’re not improving, ask for a referral.


Elliot Barrett
December 9, 2025 AT 00:18Yeah right, like I'm gonna spend $35k a year on some fancy biologic just to not wheeze. My inhaler works fine. Stop selling fear.
Shubham Mathur
December 9, 2025 AT 22:48Bro I been through this for 10 years. Dust mites in my bed? Changed sheets every week. Got covers. Vacuumed with HEPA. Still coughing. Then I did immunotherapy. Took 18 months. Felt worse at first. Quit. Came back. Now I don't need my rescue inhaler unless I'm around my neighbor's cat. Don't give up too soon. It's a grind but worth it. 🙌
Rich Paul
December 10, 2025 AT 20:52so like… IgE? eosinophils? feNO? bro i just know when i sneeze i start wheezing. doc says i got allergic asthma. i got the inhaler. why do i need to know all this science junk? also my cat is my emotional support animal so nope not letting him out the bedroom. he sleeps on my chest. deal with it.
Ruth Witte
December 11, 2025 AT 00:29OMG YES THIS!! 🙏 I used to be in the ER every other month. Then I started using that pollen app and switched to hypoallergenic pillowcases. My asthma is MILD now. I can run again!! 🏃♀️💨 Don’t let anyone tell you it’s just ‘bad luck’-you got power over this! 💪❤️
Katherine Rodgers
December 11, 2025 AT 15:53So let me get this straight. You want me to spend thousands on shots and special vacuum cleaners… so I can avoid my cat? The only thing that makes me happy? Also, who funded this article? Allergist ads? 😏
Lauren Dare
December 12, 2025 AT 03:15The GINA guidelines changed in 2023 to classify by endotype? Interesting. But you didn’t mention that the FDA only approved tezepelumab for patients with ≥3 exacerbations in the prior year. Most primary care docs don’t even know what FeNO is. So this whole ‘you can fix it’ narrative is built on a foundation of privilege. Not everyone can afford testing, let alone $30k/year biologics. Just saying.
Gilbert Lacasandile
December 13, 2025 AT 09:49I’ve been reading this thread and I just want to say… I get it. Some of you are frustrated. Some are hopeful. I’m somewhere in between. I tried the immunotherapy. It was a hassle. But I didn’t quit. I’m not cured. But I’m better. Maybe that’s enough for now.
Michael Robinson
December 13, 2025 AT 20:38It’s not about fixing your lungs. It’s about listening to them. Your body’s screaming at you through wheezes and coughs. Allergies aren’t the enemy-they’re the messenger. The real question is: what are you avoiding in your life that’s just as toxic as dust mites?
Kathy Haverly
December 15, 2025 AT 17:29Of course they say immunotherapy works. Who benefits? Pharma. Who pays? You. And don’t get me started on the ‘allergic march’-it’s just a story to sell more tests. My asthma started after a virus. I’m not allergic to anything. But they still want to poke my skin and charge me $400. I’m not your lab rat.
Andrea Petrov
December 16, 2025 AT 11:49Did you know the CDC quietly stopped tracking asthma hospitalizations in 2020? And that the WHO admitted allergen avoidance has no proven long-term benefit in double-blind trials? They’re just pushing this ‘allergy = asthma’ narrative to sell more tests and biologics. Your cat isn’t poisoning you. The air pollution from your HEPA filter’s motor is. 🤫