More people are using cannabis-whether it’s CBD oil for anxiety, THC for pain, or full-spectrum products for sleep-but many don’t realize how deeply it can affect their other medications. This isn’t theoretical. Real people are ending up in the hospital because they didn’t know mixing cannabis with blood thinners, seizure drugs, or antidepressants could be dangerous. If you’re taking any prescription meds and using cannabis, you need to understand what’s happening inside your body.
How Cannabis Changes How Your Medications Work
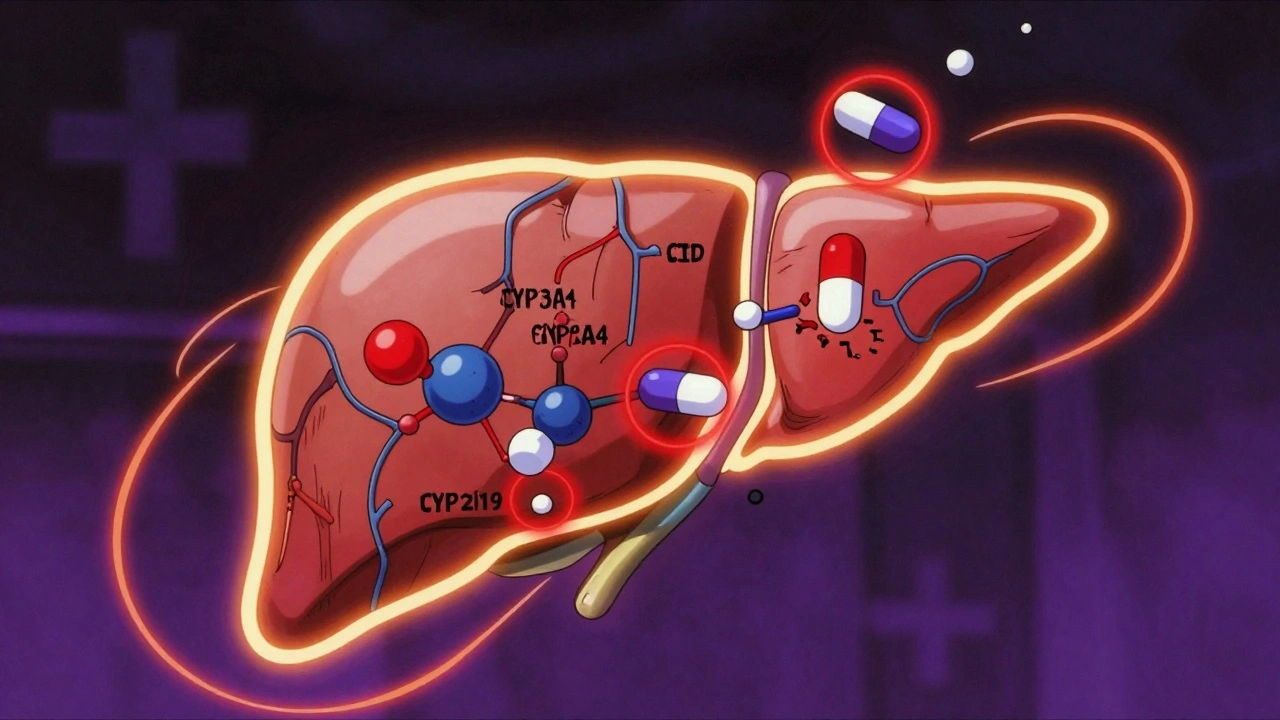
Cannabis doesn’t just float through your system. Its main active compounds-CBD and THC-directly interfere with enzymes in your liver that break down about 60% of all prescription drugs. These are called CYP450 enzymes, and when they’re blocked, your medications don’t get cleared the way they should. That means they build up in your blood, sometimes to dangerous levels.
CBD is especially powerful at shutting down CYP3A4 and CYP2C19. That’s the same enzyme family that handles blood thinners like warfarin, seizure meds like clobazam, and even some cholesterol drugs. THC also steps in, blocking CYP1A2 and CYP2C9. The result? A medication that was working fine suddenly becomes too strong-or, in rare cases, gets broken down too fast and stops working at all.
It’s not just about dose. Full-spectrum cannabis products-which include trace amounts of THC along with CBD-can be 22-37% more likely to cause interactions than pure CBD isolates. That’s because the other plant compounds amplify the effect, something called the "entourage effect." Even 5-10 mg of CBD per day can change how your body handles certain drugs. For some people, that’s enough to cause trouble.
High-Risk Interactions: When Mixing Could Be Life-Threatening
Some combinations are not just risky-they’re dangerous. The biggest red flags involve medications with a narrow therapeutic window, meaning the difference between a helpful dose and a toxic one is tiny.
Warfarin (Coumadin): This blood thinner is one of the most common culprits. When CBD or THC is added, INR levels-the measure of how long your blood takes to clot-can jump by 29-48% within just 72 hours. That means a simple bruise can turn into a major bleed. One study tracked 17 cases of serious gastrointestinal bleeding directly linked to cannabis use with warfarin. The American College of Clinical Pharmacy says: avoid this mix unless you’re under close medical supervision.
Tacrolimus and Cyclosporine: These are transplant drugs. If you’ve had a kidney or liver transplant, even small amounts of cannabis can cause tacrolimus levels to spike by 300-500%. That can lead to kidney failure or other organ damage. Transplant centers now routinely screen patients for cannabis use and adjust doses before any new product is started.
Antiepileptic drugs like clobazam: In epilepsy patients using CBD (like Epidiolex), clobazam levels can rise by 60-500%. That’s why neurologists often cut clobazam doses by 25-50% when adding CBD. One patient on Reddit described being so sedated they couldn’t walk straight-until their doctor slashed the clobazam dose. Without that adjustment, the risk of falls, confusion, and breathing problems skyrockets.
Moderate-Risk Interactions: Watch for Signs
These combinations won’t always cause emergencies, but they can make daily life harder-and sometimes more dangerous.
Benzodiazepines (alprazolam, lorazepam): Both cannabis and these anxiety meds slow down your central nervous system. Together, they can double your drowsiness. In older adults, this increases fall risk by 47%, according to the Pennsylvania Pharmacists Association. If you’re taking Xanax or Ativan and start CBD, pay attention to how you feel when standing up, driving, or walking down stairs.
Opioids (oxycodone, morphine): Cannabis can slow the body’s ability to clear these painkillers by 20-30%. That means longer-lasting effects and higher risk of slowed breathing. Some patients report no issues, but others have needed emergency care after combining them. Don’t assume you’re fine just because you’ve used both before.
Calcium channel blockers (amlodipine, diltiazem): These blood pressure meds can build up when taken with cannabis, causing dizziness, fainting, or dangerously low blood pressure. About 15-25% of users report these symptoms, especially when starting a new CBD product.
Lower-Risk Interactions: Still Worth Monitoring
Some medications show only minor changes when mixed with cannabis-and most people won’t notice.
SSRIs (sertraline, fluoxetine): CBD may slightly raise SSRI levels by 10-15%, but studies and patient reports show almost no clinical effect. In a survey of 872 people using both, 41% reported no change at all. That doesn’t mean it’s risk-free, but it’s far less urgent than warfarin or transplant drugs.
Statins (atorvastatin): CBD can increase statin levels by 20-25%, but there’s no documented case of muscle damage (rhabdomyolysis) from this combo. Still, if you start feeling unexplained muscle pain or weakness, get it checked.
Theophylline: This asthma drug behaves differently. Smoked cannabis actually lowers its levels by 25-30% because it speeds up the enzyme that breaks it down. If you’re on theophylline and start smoking cannabis, your asthma control could worsen. CBD tea or edibles don’t have this effect.
How You Take Cannabis Changes the Risk
It’s not just what you use-it’s how.
If you smoke or vape, THC hits your bloodstream in 6-10 minutes. That means sudden, intense interactions with sedatives or painkillers. You might feel overly sleepy or dizzy within minutes. This is especially risky if you’re driving or operating machinery.
Oral products-oils, capsules, gummies-take 2-4 hours to peak and last 6-8 hours. That creates a longer window for interactions with drugs like warfarin or clobazam. You might feel fine at first, then notice side effects the next day.
Topicals (creams, patches) rarely cause systemic interactions because they don’t enter the bloodstream in significant amounts. But if you’re using them over large areas of skin or broken skin, even these can become a concern.

What You Should Do Right Now
Here’s what to do if you’re using cannabis and any prescription medication:
- Be honest with your doctor and pharmacist. Don’t say "I use weed." Say: "I take 25 mg of CBD oil every night," or "I smoke cannabis twice a week for pain." Include the product type (full-spectrum, isolate), dose, and frequency.
- Check your meds. If you’re on warfarin, tacrolimus, clobazam, or any blood pressure, seizure, or pain drug, assume there’s a risk until proven otherwise.
- Get baseline tests. If you’re on warfarin, ask for an INR check before starting cannabis. For transplant drugs, ask for a blood level test.
- Monitor closely after starting. Check for new dizziness, excessive sleepiness, bruising, confusion, or unusual fatigue. These are early warning signs.
- Don’t self-adjust doses. Never reduce your prescription meds on your own. Talk to your provider first.
Pharmacists are your best ally here. The American Pharmacists Association says 76% of community pharmacists feel unprepared to answer these questions-but that doesn’t mean they can’t help. Ask: "Can you check if this CBD product interacts with my other meds?" Most can access tools like the University of Washington’s Cannabis Drug Interactions database.
What’s Changing Right Now
Research is catching up. The FDA launched the Cannabis Clinical Trials Network in 2023, and a major NIH-funded study at the University of Arkansas is tracking 200 patients on warfarin and CBD. Early results show a 37% average INR increase at doses over 25 mg/day. That’s not small.
By 2027, experts expect evidence-based guidelines for 85% of high-risk combinations. But right now, the rules are still being written. New products-like CBD-infused gummies, vape pens, or topical patches-are hitting the market faster than safety data can be collected.
One thing is clear: the more you use, the higher the risk. A 2022 survey found that 42% of cannabis users in the U.S. also take prescription meds. That’s over 24 million people. And only 12 states require pharmacists to counsel on these interactions. Most people are flying blind.
If you’re using cannabis with any medication, don’t wait for a crisis. Talk to your care team today. Keep a log: what you took, when, and how you felt. That information could save your life.
Can I take CBD with my blood thinner?
It’s risky. CBD can increase the levels of warfarin in your blood, raising your INR and increasing bleeding risk by up to 48% within 72 hours. If you’re on warfarin, do not start CBD without talking to your doctor. You’ll need frequent INR checks-every 3-5 days at first-until your levels stabilize. Some doctors will advise avoiding it entirely.
Does THC interact with medications the same way as CBD?
Not exactly. CBD mainly blocks CYP3A4 and CYP2C19, while THC affects CYP1A2 and CYP2C9. Both can interfere with warfarin, but THC is more likely to interact with antidepressants and asthma drugs like theophylline. Full-spectrum products (with both CBD and THC) carry higher interaction risks than CBD isolates. THC also adds sedation on top of other CNS depressants like opioids or benzodiazepines.
I’m using CBD for sleep. Will it mess with my antidepressant?
For most people, the interaction between CBD and SSRIs like sertraline or fluoxetine is mild. Studies show only a 10-15% increase in SSRI levels, and most users don’t notice any change. But if you’ve had side effects like nausea, agitation, or dizziness when starting CBD, it might be worth checking with your doctor. It’s rare, but not impossible.
How long should I wait between taking my meds and CBD?
Some sources suggest spacing them 2 hours apart, but there’s little solid evidence this helps. The enzymes that break down your meds are active all day. If you’re on a high-risk drug like warfarin or tacrolimus, timing won’t prevent the interaction. The only reliable way is to monitor blood levels and adjust doses under medical supervision.
Are topical CBD products safe with medications?
Generally, yes. Topical CBD creams and patches don’t enter your bloodstream in large enough amounts to affect liver enzymes. But if you’re using them over large areas, broken skin, or with high concentrations, there’s a small chance of absorption. If you’re on a high-risk medication, it’s still safest to check with your pharmacist.
What should I do if I start feeling too sleepy after adding CBD?
Stop the CBD immediately and contact your doctor. Excessive drowsiness can mean your other meds are building up in your system. If you’re on seizure meds, opioids, or benzodiazepines, this could be dangerous. Keep a log of when you took each substance and what symptoms you experienced. Bring that to your appointment.
Final Thoughts: Don’t Guess, Check
Cannabis isn’t a harmless supplement. It’s a powerful plant with real, measurable effects on your body’s chemistry. The same compounds that help with pain or anxiety can also make your heart medication too strong, your blood thinner too dangerous, or your seizure control worse.
There’s no universal rule. What’s safe for one person might be risky for another. Your age, liver health, other meds, and even your diet can change how this plays out. The only way to stay safe is to be informed, speak up, and get tested when needed.
If you’re using cannabis and medications, you’re not alone. But you shouldn’t be left to figure it out on your own. Ask your pharmacist. Talk to your doctor. Keep track. Your safety depends on it.

Eric Vlach
December 3, 2025 AT 06:13Souvik Datta
December 4, 2025 AT 15:17Irving Steinberg
December 6, 2025 AT 03:30Matt Dean
December 7, 2025 AT 00:56Walker Alvey
December 7, 2025 AT 14:06James Steele
December 8, 2025 AT 10:16Louise Girvan
December 8, 2025 AT 13:58Dennis Jesuyon Balogun
December 10, 2025 AT 04:17Grant Hurley
December 11, 2025 AT 17:06Nnaemeka Kingsley
December 13, 2025 AT 07:14Sean McCarthy
December 13, 2025 AT 17:31Jaswinder Singh
December 15, 2025 AT 07:44Bee Floyd
December 16, 2025 AT 03:39Jeremy Butler
December 17, 2025 AT 09:15Courtney Co
December 18, 2025 AT 00:12Eric Vlach
December 19, 2025 AT 03:26