When you’re pregnant and diagnosed with gestational diabetes, the first thing you might feel is overwhelm. But here’s the truth: gestational diabetes diet isn’t about restriction-it’s about rhythm. It’s about knowing when to eat, what to eat, and how much to eat so your body and baby stay balanced. You don’t need to become a nutritionist overnight. You just need clear, practical guidance.
What Are the Real Blood Sugar Targets?
The numbers matter-not because they’re scary, but because they’re your roadmap. The International Association of Diabetes and Pregnancy Study Groups (IADPSG) sets the standard: fasting blood sugar below 95 mg/dL, under 140 mg/dL one hour after eating, and under 120 mg/dL two hours after eating. These aren’t arbitrary. They’re based on decades of research showing that staying within these ranges cuts your risk of having a baby over 9 pounds by nearly a third and reduces the chance of needing a C-section by over 20%.
Many women think they need to avoid sugar completely. That’s not true. It’s about how fast your body turns food into glucose. That’s why timing and food quality matter more than cutting out entire food groups. A banana eaten with peanut butter behaves very differently in your body than the same banana eaten alone. The goal is to keep those spikes gentle and predictable.
The Plate Method: Simple, Visual, and Effective
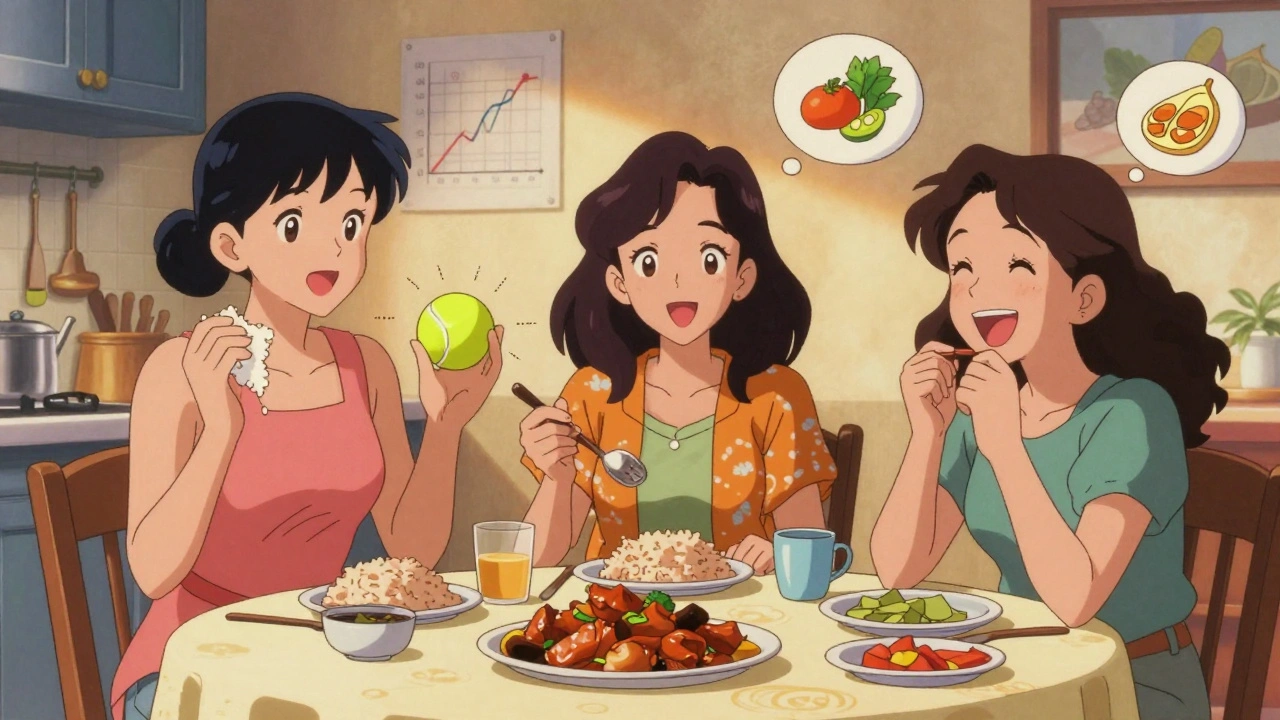
Forget counting grams if you’re drowning in morning sickness or just don’t have the mental bandwidth. The plate method works because it’s visual. Take a nine-inch plate. Fill half with non-starchy vegetables-broccoli, spinach, peppers, zucchini. These are low in carbs and high in fiber, which slows down sugar absorption. One-quarter of the plate gets lean protein: chicken, fish, tofu, eggs. The last quarter gets your carbohydrate source: brown rice, quinoa, sweet potato, whole grain bread.
This method isn’t just theory. A 2017 clinical trial with 1,200 women found it worked just as well as carb counting for controlling blood sugar. And here’s the kicker: 37% more women stuck with it long-term because it didn’t require scales or apps. If you’re wondering how big a serving is, think of it this way: one serving of cooked rice or pasta is about two heaped tablespoons-the size of a tennis ball. One slice of whole grain bread is one serving. One medium apple is one serving.
Carb Counting: Precision for Those Who Need It
If you’ve had insulin resistance before pregnancy, or your doctor recommends tighter control, carb counting gives you more precision. The American Diabetes Association recommends 45 to 60 grams of net carbs per meal and about 15 grams per snack. Net carbs = total carbs minus fiber. So if you eat a cup of cooked lentils with 40g total carbs and 15g fiber, that’s 25g net carbs.
But here’s the catch: fiber is your secret weapon. Meals with at least 6 grams of fiber help blunt blood sugar spikes. That’s why beans, lentils, chia seeds, and whole grains are your allies. A 2008 study in the New England Journal of Medicine showed meals with high fiber led to significantly lower post-meal glucose levels. Don’t just look at the carb count-look at the fiber.
When and How Often to Eat
It’s not just what you eat-it’s when. Skipping meals or going too long without eating can actually make your fasting blood sugar worse. That’s because your liver starts releasing stored glucose to keep you going, and with gestational diabetes, your body can’t handle the extra load.
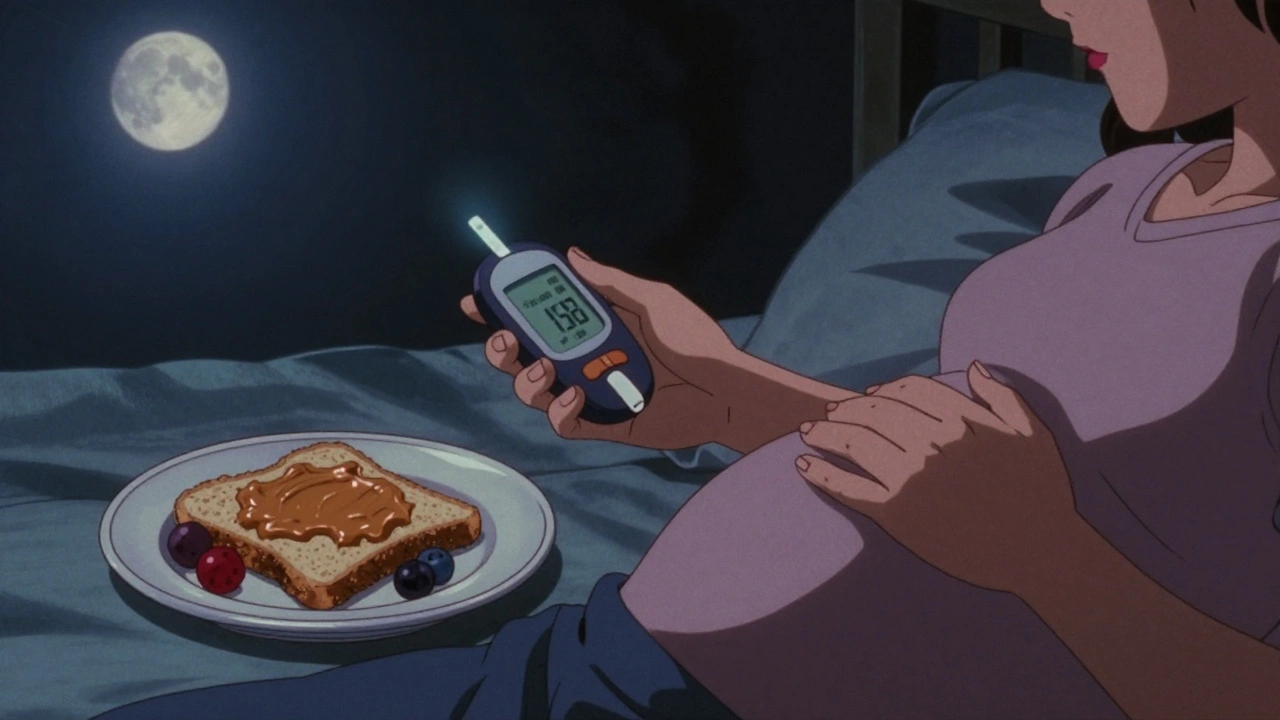
Most women do best with three meals and three small snacks spaced evenly through the day. For example: breakfast, mid-morning snack, lunch, afternoon snack, dinner, and a light bedtime snack. The bedtime snack is especially important-it helps prevent your liver from overproducing glucose overnight. A good option? 1 ounce of cheese with 15 grams of carbs, like half a whole grain English muffin. That combo gives you protein and slow-digesting carbs to stabilize overnight levels.
What Works in Real Life: Stories from Women Who’ve Done It
Reddit threads and patient surveys reveal something consistent: women who succeed with gestational diabetes don’t follow perfect meal plans-they follow ones that fit their lives.
One woman, u/Pregnant_and_Worried, said: “Measuring rice in tablespoons was impossible with morning sickness-I just fill half my plate with broccoli and it works.” That’s the plate method in action. Another woman, a Filipino mom, praised a cookbook that included adobo chicken with half a cup of brown rice-it hit her carb target while still tasting like home.
On the flip side, women who struggled often cited carb counting as overwhelming. Nearly half of those who dropped out of structured programs said they felt anxious or guilty when they couldn’t measure everything perfectly. That’s why simplicity often wins. You don’t need to be exact. You need to be consistent.
Foods That Help (and Foods That Don’t)
Not all carbs are created equal. Avoid white bread, sugary cereals, fruit juice, and sweetened yogurt. They spike blood sugar fast and leave you hungry again in an hour. Instead, choose:
- Whole grains: oats, barley, quinoa, whole wheat pasta
- Legumes: lentils, black beans, chickpeas
- Non-starchy vegetables: leafy greens, cauliflower, asparagus, cucumbers
- Fruits in moderation: berries, apples, pears (pair with protein)
- Healthy fats: avocado, nuts, olive oil, seeds
- Lean proteins: chicken, turkey, fish, eggs, tofu
Watch out for “diabetic-friendly” packaged foods. A 2023 Lancet study found these products often have 27% more sodium than regular whole foods. They’re marketed as safe, but they’re still processed. Stick to real food whenever you can.
What About the Mediterranean Diet?
Some women find success with the Mediterranean approach-lots of vegetables, olive oil, fish, nuts, and legumes. A 2019 study in the American Journal of Clinical Nutrition showed this diet led to 15% lower post-meal glucose spikes compared to standard GDM plans. The downside? It requires more cooking skills. In one 2022 study, 28% of women with lower health literacy struggled to adapt the plan to their kitchen.
If you already enjoy cooking and love olive oil, lentils, and grilled fish, this could be a great fit. If you’re short on time or energy, stick with the plate method. You don’t need to follow a trendy diet-you need to follow a plan that works for you.
Common Mistakes and How to Avoid Them
Here are the top three mistakes women make-and how to fix them:
- Underestimating portion sizes. A 2021 study found 38% of women misjudged cooked rice portions by nearly 22 grams-adding 7 extra carbs per meal. Use visual cues: 1/2 cup cooked grains = tennis ball. One serving of meat = deck of cards.
- Skipping meals to “save carbs.” This backfires. Fasting blood sugar rises because your liver dumps glucose. Eat every 2-3 hours, even if it’s just a hard-boiled egg and a few almonds.
- Ignoring protein at every meal. Protein slows carb absorption. If your breakfast is just toast and jam, you’ll spike and crash. Add eggs, Greek yogurt, or peanut butter. Protein-first meals are a game-changer.
Support Is Everything
Managing gestational diabetes alone is hard. That’s why community matters. The Facebook group “Gestational Diabetes Support” has over 147,000 members. In a 2023 survey, 89% said joining reduced their anxiety. You’re not alone. Share your struggles, ask for meal ideas, and celebrate small wins.
Many hospitals now offer free Gestational Diabetes Self-Management Programs. These are three 60-minute sessions covering carb identification, portion control, and timing. They’re designed to take the guesswork out. Ask your OB or midwife if they offer one.
And if you’re feeling overwhelmed, it’s okay to ask for help. Insurance now covers virtual dietitian visits for GDM under recent CMS guidelines. You don’t have to figure this out on your own.
What’s Next? Tools and Trends
The future of gestational diabetes care is personalization. The ADA just launched a mobile app that syncs with continuous glucose monitors (CGMs) and suggests meals based on your real-time numbers. In a 2023 pilot, users improved their time-in-range by 23%. Companies like Virta Health are using AI to adjust carb targets daily based on your glucose patterns-cutting hypoglycemia events by 31% in trials.
But even with all the tech, the foundation hasn’t changed: eat real food, spread carbs out, pair them with protein and fiber, and move your body. You’re not fighting your body-you’re helping it work better.
Can I still eat fruit with gestational diabetes?
Yes, but choose wisely. Berries, apples, pears, and oranges are lower in sugar and high in fiber. Eat them with a source of protein or fat-like a handful of almonds or a spoon of Greek yogurt-to slow the sugar spike. Avoid fruit juice, dried fruit, and tropical fruits like mango and pineapple in large amounts.
Do I need to take insulin if I follow a diet?
Not always. About 70% of women with gestational diabetes can manage their blood sugar with diet and exercise alone, according to a 2021 study in Diabetes Technology & Therapeutics. But if your numbers stay high after a few weeks, insulin isn’t a failure-it’s a tool. It’s safe for your baby and helps protect both of you from complications.
Is it okay to eat carbs at night?
Yes, but keep it light and balanced. A small snack with protein and slow-digesting carbs-like a slice of whole grain toast with peanut butter or cottage cheese with a few berries-can help prevent your liver from overproducing glucose overnight. Avoid sugary snacks or refined carbs before bed.
How much protein should I eat daily?
The recommended intake is about 0.8 grams of protein per kilogram of body weight during pregnancy, rising slightly in the third trimester. For most women, that’s 75-100 grams per day. Spread it across meals: eggs at breakfast, chicken at lunch, beans at dinner. Protein helps stabilize blood sugar and supports your baby’s growth.
Can gestational diabetes go away after pregnancy?
Most of the time, yes. Blood sugar levels usually return to normal after delivery. But having gestational diabetes increases your risk of developing type 2 diabetes later-up to 50% within 10 years. The good news? Maintaining a healthy diet and staying active after pregnancy can cut that risk in half.
Are there foods I should avoid completely?
You don’t need to eliminate anything forever, but it’s best to avoid sugary drinks, white bread, pastries, candy, and processed snacks labeled “diabetic-friendly”-they’re often high in sodium and artificial ingredients. Focus on whole, unprocessed foods instead. Occasional treats are fine if they fit your carb budget and are paired with protein or fat.

Mindy Bilotta
December 2, 2025 AT 19:22just ate a banana with peanut butter for snack and my glucose stayed steady. i thought i was doomed but this post literally saved my sanity. thank you.
Ethan McIvor
December 3, 2025 AT 23:57it’s wild how much our bodies just want to work with us if we stop fighting them. gestational diabetes isn’t a punishment-it’s a nudge to eat like humans evolved to eat. whole foods, spaced meals, protein first. no magic, just rhythm. 🌿
Michael Bene
December 4, 2025 AT 19:34lol the plate method? that’s what my 5-year-old uses for lunch. and yet somehow it’s more effective than the 17-page carb-counting spreadsheet my endo made me print out. also, ‘diabetic-friendly’ snacks are just sugar with a side of sodium guilt. 🤡
Joykrishna Banerjee
December 6, 2025 AT 00:58the plate method is statistically inferior to the Nordic Diet’s 16:8 intermittent fasting protocol with low-glycemic legumes and fermented dairy. unless you’re optimizing for mitochondrial efficiency, you’re just delaying metabolic decline. 📉
Myson Jones
December 6, 2025 AT 20:08i appreciate how this post avoids fear-based language and instead offers practical, evidence-based tools. many women feel isolated with this diagnosis-this kind of compassionate clarity is exactly what’s needed.
parth pandya
December 8, 2025 AT 17:29u forgot to mention that cinnamon helps lower post meal spikes. add a tsp to your oatmeal or coffee. also, walk 10 min after eating. it’s free and works better than meds for some. 🙌
Albert Essel
December 9, 2025 AT 20:06the data supporting the plate method is solid, and the emphasis on consistency over perfection is what makes this approach sustainable. too many programs fail because they demand impossible precision.
Charles Moore
December 11, 2025 AT 18:35if you’re feeling overwhelmed, start with one change: add protein to your breakfast. that one swap changes everything. you don’t need to overhaul your life today. just show up, one meal at a time.
Rashi Taliyan
December 13, 2025 AT 05:07i cried reading this. i thought i was failing because i couldn’t measure everything. but i’ve been doing the plate thing since week 2 and my numbers are better than my sister’s who’s on insulin. thank you for saying it’s okay to be messy.
Brian Perry
December 13, 2025 AT 17:34okay but what if your doctor is a dinosaur and still thinks you should eat 300g of carbs a day? i got scolded for eating avocado. like, i’m pregnant not on a keto cult. this post is the only thing keeping me from throwing my glucometer out the window. 😭
Gene Linetsky
December 14, 2025 AT 23:39they’re lying about insulin being safe. it’s a pharmaceutical scam to keep you dependent. your body can heal itself if you just stop eating carbs and start drinking apple cider vinegar. i know because i cured my diabetes with a lemon and a prayer.
Myson Jones
December 15, 2025 AT 22:19thank you for sharing your experience, Mindy. Your honesty about feeling overwhelmed is so important. For anyone reading this-your feelings are valid, and you’re not alone. Small steps still move mountains.