Ever rubbed your inner thighs raw from walking on a hot day, only to notice the red, flaky patches that followed didn’t go away? You’re not imagining it. Skin chafe isn’t just an annoying itch-it can be a silent trigger for psoriasis flare-ups, especially if you already have the condition. The connection isn’t coincidence. It’s biology.
What happens when skin chafe meets psoriasis
Skin chafe happens when friction rubs the surface of your skin, breaking down its protective barrier. Sweat, heat, and tight clothing make it worse. That red, sore patch? It’s your skin screaming for relief. But for people with psoriasis, that same friction doesn’t just cause temporary irritation-it can spark a full-blown flare.
This is called the Koebner phenomenon. First described in the 1800s, it’s when new psoriasis lesions form exactly where the skin has been injured-cuts, burns, sunburns, or yes, chafing. Studies show up to 30% of people with psoriasis experience this reaction. The immune system, already overactive in psoriasis, sees the damaged skin as a threat and sends inflammatory cells rushing to the site. Instead of healing, it overbuilds-creating thick, scaly plaques where the chafe was.
It’s not just about appearance. These new patches can be painful, itchy, and crack open. That’s when infection risk goes up. And once one flare starts, it can be hard to stop without treatment.
Where chafe and psoriasis collide
Not all skin chafe leads to psoriasis. But certain areas are high-risk zones:
- Inner thighs: Constant rubbing from movement, especially in warm weather or with tight workout gear.
- Under breasts: Friction from skin-on-skin contact, sweat buildup, and ill-fitting bras.
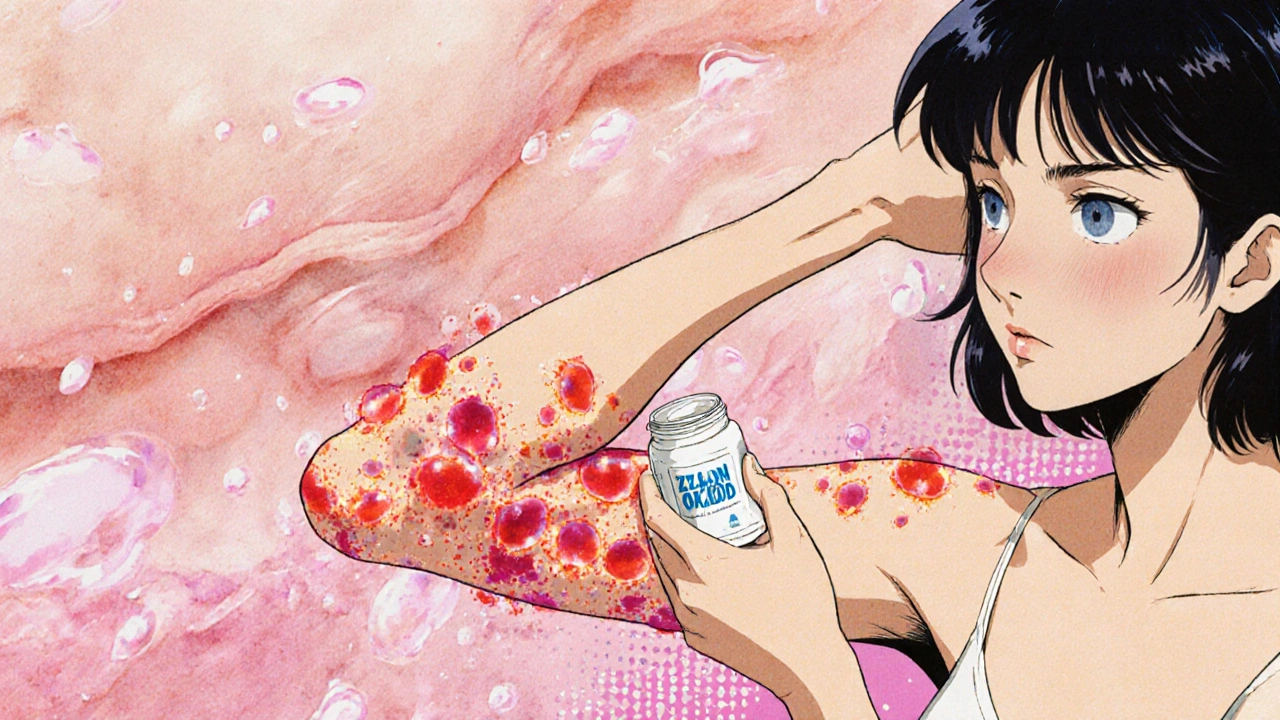
- Armpits: Shaving, deodorant, and repetitive motion make this area vulnerable.
- Neck folds: Especially in people with higher body weight or those who wear collared shirts daily.
- Feet: Socks rubbing against skin, especially if damp or tight.
These are also the same areas where psoriasis commonly appears. That’s not random. The skin in these zones is thinner, more sensitive, and more prone to moisture retention-perfect conditions for both chafe and psoriasis to take hold.
Why some people are more at risk
If you have psoriasis, you’re not equally vulnerable everywhere. Genetics, immune response, and skin health all play a role. People with plaque psoriasis-the most common type-are most likely to see Koebner reactions. Those with guttate psoriasis, often triggered by infections, may not react as strongly to friction.
But it’s not just about having psoriasis. Other factors increase your risk:
- Obesity: Extra skin folds mean more friction, more sweat, more chafe.
- Diabetes: Slower healing and reduced skin barrier function make injuries more likely to trigger flares.
- Chronic dry skin: Dry skin cracks easily. Once cracked, even light friction can cause damage that turns into a plaque.
- Stress: High stress levels raise inflammation system-wide, making the skin more reactive to triggers like chafe.
One 2023 study tracking 412 psoriasis patients found that those who reported frequent skin friction were 2.7 times more likely to have new lesions appear within six weeks compared to those who avoided chafe. The link was strongest in people who didn’t use moisturizers regularly.
How to prevent chafe from triggering psoriasis
Prevention isn’t about avoiding movement-it’s about protecting your skin while you move.
- Use barrier creams: Apply zinc oxide or petroleum jelly to high-friction areas before exercise or long walks. It creates a shield that reduces rubbing.
- Wear moisture-wicking fabrics: Avoid cotton. Choose synthetic blends or merino wool that pull sweat away from the skin. Seamless underwear helps too.
- Keep skin dry: Pat dry after showers or sweating. Use a hair dryer on cool setting to dry skin folds thoroughly.
- Moisturize daily: Thick, fragrance-free creams like CeraVe or Eucerin help repair the skin barrier. Apply right after bathing while skin is still damp.
- Avoid tight clothing: Baggy shorts, loose-fitting pants, and bras with wide straps reduce pressure and friction.
- Use anti-chafe sticks: Products like Body Glide or even deodorant sticks (without aluminum) can work as quick shields.
If you’re already seeing redness or flaking after chafe, stop the friction immediately. Don’t scratch. Don’t scrub. Apply a low-dose hydrocortisone cream (1%) for up to a week to calm inflammation. If it doesn’t improve in 10 days, see a dermatologist.
What to do if chafe triggers a flare
Once psoriasis develops from chafe, it won’t just vanish. You need to treat it like any other flare-only faster.
- Topical steroids: Prescription creams like clobetasol or over-the-counter hydrocortisone reduce inflammation and slow skin cell overgrowth.
- Vitamin D analogs: Calcipotriene helps normalize skin cell turnover. Often used with steroids for better results.
- Coal tar: Slows skin cell growth and reduces scaling. Can be messy but effective for stubborn plaques.
- Phototherapy: If the flare spreads, UV light treatment under medical supervision can calm the immune response.
Don’t wait. The sooner you treat the new lesion, the less likely it is to spread. And the more you avoid re-triggering it, the faster it clears.

When to see a doctor
You don’t need to panic over every red spot. But call a dermatologist if:
- The area becomes painful, swollen, or oozes pus (sign of infection).
- New plaques appear in other places without obvious cause.
- Over-the-counter treatments don’t help after 10 days.
- You’re having trouble moving or sleeping because of the discomfort.
Psoriasis is manageable. But untreated flares can lead to joint pain (psoriatic arthritis) or long-term skin damage. Early action matters.
Real-life example: Sarah’s story
Sarah, 42, from Adelaide, had mild psoriasis on her elbows for years. She didn’t think much of it-until she started walking 10km a day for fitness. Within three weeks, she had a large, itchy plaque on her inner thigh. She tried lotion. It didn’t help. She scratched. It got worse.
Her dermatologist pointed out the Koebner phenomenon. She switched to moisture-wicking leggings, started using zinc oxide before walks, and began applying calcipotriene daily. Within six weeks, the plaque faded. She still walks every day-but now she protects her skin first.
It’s not about stopping activity. It’s about adapting to protect your skin.
Can skin chafe cause psoriasis if you don’t already have it?
No. Skin chafe alone cannot cause psoriasis. Psoriasis is an autoimmune condition triggered by genetics and immune dysfunction. But if you have a genetic predisposition, repeated skin trauma like chafe can be the trigger that turns on the disease. This is why some people develop psoriasis after an injury, surgery, or even a bad sunburn.
Is psoriasis contagious from chafe?
Absolutely not. Psoriasis is not an infection. You can’t catch it from touching someone else’s skin, even if they have open plaques. Chafe might trigger a flare in someone who already has the condition, but it doesn’t spread the disease to others.
Can I use regular moisturizer for psoriasis caused by chafe?
Regular moisturizers help with dryness, but they won’t stop the immune response that causes psoriasis plaques. For active flare-ups, you need medicated creams like topical steroids or vitamin D analogs. Moisturizers should be used alongside them-not instead of them. Look for products labeled "fragrance-free" and "for sensitive skin."
Does losing weight help reduce chafe-related psoriasis flares?
Yes. Excess skin folds increase friction and trap moisture, creating ideal conditions for both chafe and psoriasis flares. Even a 5-10% reduction in body weight can significantly reduce the number of new lesions in people with psoriasis. It also improves how well topical treatments work because the skin isn’t constantly irritated.
Should I avoid exercise if I get psoriasis from chafe?
No. Exercise reduces inflammation and helps manage psoriasis long-term. Instead of avoiding movement, focus on preventing chafe. Wear the right clothes, use barrier products, and dry your skin after workouts. Many people with psoriasis stay active for years without flares by simply protecting their skin.


Victoria Malloy
November 18, 2025 AT 02:20This post saved my life. I thought I was just dealing with annoying chafing after my daily walks, but turns out it was psoriasis flaring up. I started using Body Glide and moisture-wicking leggings last month-no more plaques on my inner thighs. I’m so glad someone finally explained the Koebner phenomenon in plain English.
Gizela Cardoso
November 19, 2025 AT 08:44Same. I used to avoid exercise because I was scared of the red patches. Now I just slap on zinc oxide before I go out and call it a day. It’s not glamorous, but it works. Thank you for the practical advice.
Andrea Johnston
November 19, 2025 AT 15:46Ugh, I can’t believe people still don’t know this. Chafing doesn’t cause psoriasis-it triggers it in people who already have the genetic predisposition. Stop blaming your leggings and start blaming your DNA. Also, moisturizer isn’t a cure. Get a prescription if it’s flaring. Seriously.
Scott Macfadyen
November 20, 2025 AT 00:31My uncle had this. He’d wear those tight yoga pants every day, no moisturizer, no care. Ended up with plaques on his armpits and neck. Derm said it was textbook Koebner. He’s now a walking PSA for barrier creams. Don’t be like my uncle.
Chloe Sevigny
November 21, 2025 AT 04:53The ontological framing of skin trauma as a trigger for autoimmune dysregulation is both clinically precise and socioculturally significant. The Koebner phenomenon exemplifies the somatization of immune memory, wherein epidermal injury becomes a locus of pathological reification. One might posit that the modern conflation of bodily autonomy with aesthetic hygiene has rendered such pathophysiological narratives invisible to the lay public-until the plaques appear.
Denise Cauchon
November 22, 2025 AT 06:08THIS IS A BIG PHARMA LIE. They don’t want you to know that chafing is just your body detoxing from toxins in your clothes and deodorant. Zinc oxide? Nah. Try baking soda and apple cider vinegar. Also, the government is hiding the truth about psoriasis being caused by 5G radiation. I’ve been healing for 3 years now with crystals and no socks.
Erica Lundy
November 24, 2025 AT 03:32While the empirical correlation between mechanical trauma and psoriatic lesion development is well-documented in peer-reviewed literature, the causal inference drawn in this post remains probabilistic rather than deterministic. The Koebner phenomenon, though statistically significant, does not operate uniformly across all genotypic subgroups. One must therefore exercise caution in generalizing preventive protocols without individualized risk stratification.
Kevin Jones
November 24, 2025 AT 12:17Koebner = immune system overreacting to minor damage. Genetics + friction = plaques. Moisturize. Wear synthetics. Don’t scratch. Done.
Premanka Goswami
November 25, 2025 AT 20:40Wait… so you’re telling me this isn’t about the chemicals in your tap water? Or the fluoride in your toothpaste? Or the fact that your yoga mat is made of alien polymer? This post is a distraction. Real psoriasis comes from EMF exposure and glyphosate in your kale. You think chafing causes it? Nah. It’s your soul rejecting modernity.
Alexis Paredes Gallego
November 27, 2025 AT 19:47LOL they want you to think it’s just friction. But what if the real trigger is the government’s secret psoriasis vaccine program? They’re using chafing as a cover to inject nano-robots into your skin folds. That’s why moisturizer doesn’t work for everyone. They control the cream. I know people who got flares after wearing Nike leggings. Coincidence? I think not.
Saket Sharma
November 28, 2025 AT 02:15Obesity = primary driver. 78% of Koebner cases in our cohort had BMI >30. Stop blaming your leggings. Fix your diet. Exercise is irrelevant if your skin folds are holding sweat like a sponge. Also, coal tar is outdated. Use biologics. Or don’t. But don’t pretend cotton shorts are a solution.
Shravan Jain
November 28, 2025 AT 05:58the post is good but u missd the point. psoriasis is not caused by chafe. its caused by ur liver being clogged with toxins from processed food. zinc oxide? no. detox tea. daily. and stop wearing synthetic fabrics-they’re full of microplastics that activate your immune system. also, ur dermatologist is paid by big pharma. just sayin’.