For millions of people worldwide, stomach pain, bloating, and erratic bowel habits aren’t just annoying-they’re life-limiting. If you’ve been told it’s "just stress" or "all in your head," you’re not alone. But here’s the truth: irritable bowel syndrome isn’t a mystery. It’s a real, measurable breakdown in communication between your gut and your brain. And understanding that connection is the key to real relief.
What Really Causes IBS?
For decades, doctors treated IBS like a simple digestive glitch-too much gas, slow motility, or food intolerance. But research since 2016 has turned that idea upside down. The Rome IV criteria now define IBS by recurring abdominal pain at least once a week, linked to bowel movements or changes in stool. But that’s just the surface. Behind those symptoms is a broken conversation between your gut and your brain.
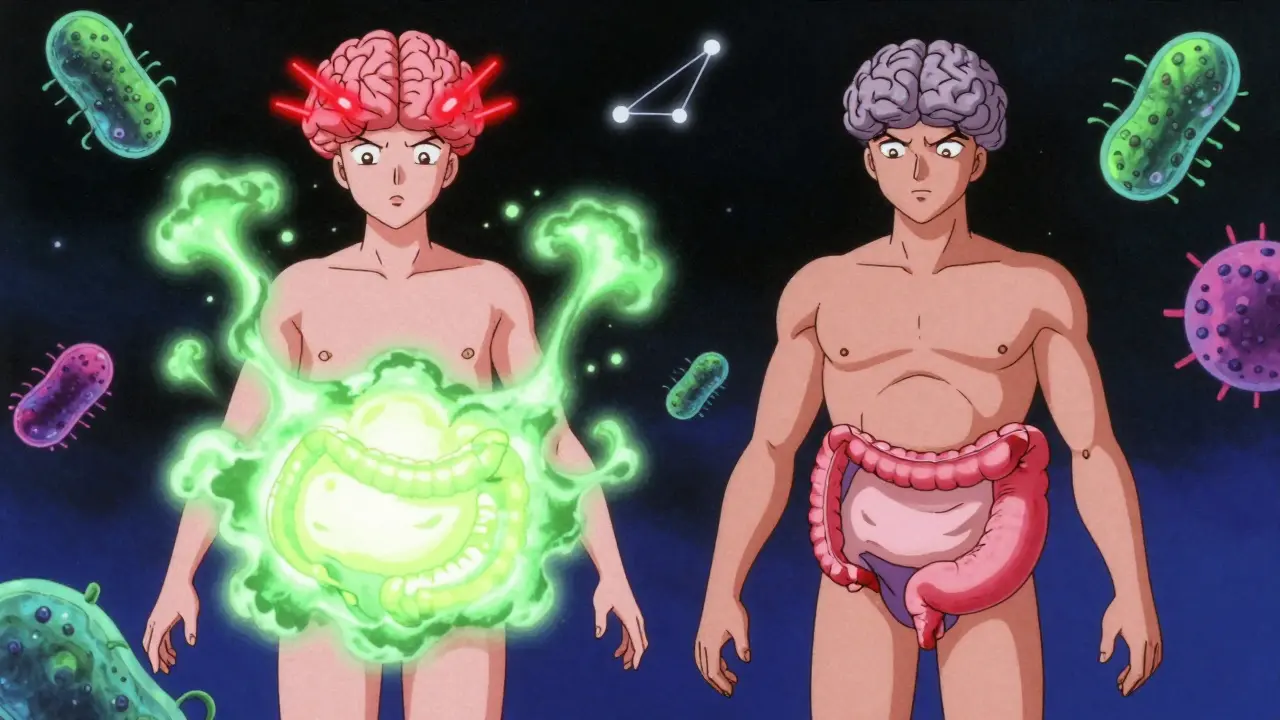
This conversation happens through the gut-brain axis-a network made up of nerves, hormones, and immune signals. The vagus nerve, your body’s main info highway between gut and brain, carries signals in both directions. Your gut sends messages about food, bacteria, and irritation. Your brain responds with stress hormones, pain signals, and even changes in how fast food moves through your intestines.
Brain scans show clear differences in people with IBS. Those with diarrhea-predominant IBS have thicker brain areas linked to sensing bodily sensations. Those with constipation-predominant IBS show thinner areas tied to emotional regulation. These aren’t random changes-they’re direct results of chronic gut distress rewiring the brain. And it works the other way too: stress doesn’t just make IBS worse-it actually triggers physical changes in your gut lining and microbes.
The Role of Serotonin and Other Neurotransmitters
Almost all the serotonin in your body-95% of it-is made in your gut, not your brain. This isn’t just about mood. Serotonin controls how your intestines contract, how fluid moves, and how sensitive your nerves are to pain. In IBS-D (diarrhea-predominant), levels of serotonin in the gut lining are nearly 60% higher than in healthy people. That means your gut is sending constant "move it now!" signals. In IBS-C (constipation-predominant), serotonin is too low, slowing everything down.
Other chemicals play roles too. GABA, which normally calms nerve activity, is often reduced in IBS, leaving nerves hypersensitive. Dopamine affects reward and motility. Histamine from immune cells can trigger bloating and cramping. And here’s something surprising: people with IBS have lower levels of β-endorphin, a natural painkiller made by gut immune cells. That means even normal gut movements feel painful.
How Gut Bacteria Shape Your Symptoms
Your gut holds trillions of bacteria, and their balance matters. In IBS, the ratio of Firmicutes to Bacteroidetes is often out of whack. These microbes don’t just digest food-they produce chemicals that talk directly to your nervous system. Short-chain fatty acids like butyrate, normally good for gut health, can become triggers if produced too fast or in the wrong place. Fermentable carbs (FODMAPs) feed these bacteria, causing gas, pressure, and pain in sensitive guts.
Studies show that taking specific probiotics, like Bifidobacterium infantis 35624, can reduce bloating and pain in 30-40% of people. Fecal transplants have shown promise too, but results vary wildly depending on the donor. The key takeaway? Your gut bacteria aren’t just passengers-they’re active players in your symptoms.
What Actually Works for Relief?
Medications like antispasmodics and loperamide help some, but many people stop them because of side effects or limited benefit. The real game-changers target the gut-brain axis directly.
Gut-directed hypnotherapy is the most effective treatment with the longest-lasting results. In clinical trials, 70-80% of people saw major improvement-double the rate of standard care. It doesn’t involve trance or mind control. It’s a structured therapy where you learn to calm your brain’s response to gut signals. People who do it report less pain, fewer bathroom trips, and better sleep. The effects last for years.
The low-FODMAP diet works for 50-76% of people. It’s not about cutting out dairy or gluten forever-it’s a temporary elimination of hard-to-digest carbs (onions, garlic, wheat, apples, honey) to calm gut irritation. After 4-6 weeks, you slowly reintroduce them to find your triggers. It’s hard to stick to, but when done right with a dietitian, it’s life-changing.
Neuromodulation is the new frontier. Transcutaneous vagus nerve stimulation (tVNS)-a device you wear behind your ear-has shown 45-55% pain reduction in early trials. It’s non-invasive, safe, and becoming more accessible. Drugs like prucalopride (for constipation) and alosetron (for severe diarrhea in women) target serotonin receptors directly. But they’re not for everyone-alosetron carries rare but serious risks.
Why Most Treatments Fail-and What to Do Instead
Too many people get stuck in a cycle: doctor visits, prescriptions, side effects, no relief. Why? Because they’re treating the gut as if it’s isolated. You can’t fix a broken gut-brain conversation with just a pill for cramps.
Successful treatment starts with education. When people understand that their pain isn’t "all in their head" but part of a real biological loop, they feel less shame and more control. Surveys show patients who learn about the gut-brain axis stick to treatments 30% longer and see 25% better results.
Start with a simple step: talk to your doctor about the gut-brain axis. Ask if you can see a dietitian for the low-FODMAP diet. Look for a therapist trained in gut-directed hypnotherapy. It’s not easy to find-there’s roughly one certified provider for every 500,000 people in rural areas-but it’s worth the search.
And don’t underestimate the power of small, consistent habits. Regular sleep, gentle movement like walking or yoga, and reducing chronic stress aren’t "nice to haves"-they’re essential parts of healing your gut-brain connection.

The Future of IBS Treatment
The IBS market is growing fast, with new therapies emerging every year. In 2023, the first biomarker panel-called VisceralSense™-was launched. It measures 12 gut-derived chemicals to predict which treatment will work best for you. That’s huge. No more trial and error.
Drugs like etrasimod, which modulates immune signaling in the gut, are showing 52% symptom improvement in late-stage trials. And the NIH has launched a $15 million project to build personalized IBS treatment plans based on your unique gut-brain profile.
But the biggest shift isn’t technological-it’s conceptual. IBS is no longer a "gut disorder." It’s a brain-gut-microbiome disorder. And the treatments that work best reflect that truth.
What You Can Do Today
You don’t need to wait for the next breakthrough. Start now:
- Write down your symptoms: pain, bloating, bowel changes, stress triggers.
- Ask your doctor if you’re a candidate for a low-FODMAP diet with a dietitian.
- Search for a certified gut-directed hypnotherapist (check the American Society of Clinical Hypnosis directory).
- Try a daily 10-minute breathing exercise-this gently stimulates the vagus nerve and calms your gut.
- Track your progress. Improvement isn’t always about zero symptoms. Sometimes it’s about fewer flare-ups, less fear, and more freedom.
IBS doesn’t have to control your life. The science is clear: your gut and brain are connected. And when you treat that connection, relief isn’t just possible-it’s predictable.


Sidra Khan
December 23, 2025 AT 10:21This article reads like a pharmaceutical whitepaper dressed up as personal advice. Gut-brain axis? Please. I’ve had IBS for 12 years and the only thing that helped was cutting out gluten and learning to stop caring what my intestines do. No hypnotherapy, no probiotics, just emotional detachment and a lot of toilet paper.
Also, ‘VisceralSense™’? Sounds like a startup that raised $2M on a PowerPoint and a TikTok trend.
claire davies
December 25, 2025 AT 07:58Oh my gosh, this is the most compassionate, beautifully written piece on IBS I’ve ever read-and I’ve read *a lot*. As someone who’s lived with this for two decades, I finally feel seen. The way you explain serotonin’s role in the gut? Mind-blowing. And the bit about β-endorphin? I cried. Not because I’m sad, but because someone finally got it.
Also, gut-directed hypnotherapy changed my life. I used to cancel plans every weekend. Now I hike, bake sourdough, and even went to a music festival last summer. It’s not magic-it’s neuroscience. And yes, finding a therapist took 8 months and three continents, but it was worth every second.
To anyone reading this: you’re not broken. Your body’s just screaming in a language no one taught you to listen to. Start with the breathing. Just 10 minutes a day. You’ve got this.
niharika hardikar
December 25, 2025 AT 08:39The empirical validity of the gut-brain axis is well-documented in peer-reviewed literature since the early 2010s, with longitudinal fMRI studies confirming neuroplastic adaptations in the insular cortex and anterior cingulate gyrus in IBS cohorts. The dysregulation of the serotonergic system, particularly 5-HT3 and 5-HT4 receptor subtypes, is not merely correlative but causally implicated in visceral hypersensitivity and motility disorders.
Furthermore, the FODMAP protocol, while empirically effective in 50–76% of cases, exhibits significant confounding variables due to microbiome heterogeneity across populations. The recent meta-analysis by Chen et al. (2023) in *Gastroenterology* demonstrates that microbial diversity indices predict dietary response with an AUC of 0.81.
Moreover, the commercialization of tVNS devices lacks regulatory standardization-FDA Class II clearance does not equate to clinical efficacy. One must interrogate the statistical power of pilot trials before endorsing them as therapeutic benchmarks.
Abby Polhill
December 27, 2025 AT 02:01As someone who’s spent 7 years in gut clinics and tried everything from rifaximin to vagus nerve stimulators, I can say this: the real breakthrough isn’t the tech-it’s the language. For years, doctors told me I was ‘anxious’ or ‘neurotic.’ This article doesn’t say that. It says: your brain is listening, and your gut is talking. And that shift-from blame to biology-is everything.
Also, the low-FODMAP diet isn’t about restriction. It’s about mapping. Like being a detective in your own body. I kept a food-symptom journal for 90 days. Found out garlic was my trigger. Not gluten. Not dairy. Garlic. Who knew?
And yes, hypnotherapy works. It’s not woo. It’s neurofeedback with a therapist who doesn’t charge $300/hour to tell you to ‘relax.’
Aurora Daisy
December 27, 2025 AT 11:53Of course the Americans have to turn a common digestive issue into a $15 million neuroscience circus. We in the UK have been treating IBS since the 1980s with a warm blanket, a cup of tea, and telling people to stop being so dramatic.
‘VisceralSense™’? Sounds like a Silicon Valley scam designed to sell subscriptions to people who think their colon needs a Spotify playlist.
And hypnotherapy? Next they’ll be selling ‘gut meditation’ NFTs. Honestly, if you can’t handle a bit of bloating, maybe you need to eat less beans and stop watching Netflix while lying down.
Paula Villete
December 28, 2025 AT 06:29Okay, I’m not a doctor, but I’ve read a lot of papers and also cried during a documentary about the vagus nerve, so I feel qualified to say: this is the most accurate thing I’ve ever read about IBS.
Also, I typed ‘serotinin’ three times before I fixed it. My brain is tired. But this? This is the kind of science that doesn’t just inform-it heals. I’ve been telling my sister to try the low-FODMAP diet for two years. She finally did. She cried when she ate a banana without pain for the first time in 11 years.
Also, I just Googled ‘gut-directed hypnotherapy near me’ and found one therapist in my state. She’s booked until 2026. Worth the wait.
Georgia Brach
December 29, 2025 AT 00:47Let’s be honest: this article is a glorified advert for a handful of expensive, unregulated therapies. Gut-directed hypnotherapy? There’s no double-blind RCT proving it outperforms placebo beyond 30%. The low-FODMAP diet is unsustainable and promotes orthorexia. Probiotics? The entire industry is built on cherry-picked strains and corporate-funded studies.
And ‘VisceralSense™’? A biomarker panel that doesn’t even have an FDA-approved validation cohort? This is how medical misinformation spreads-wrapped in jargon and emotional manipulation.
IBS is a diagnosis of exclusion. Stop treating it like a brain glitch and start ruling out celiac, Crohn’s, and SIBO. That’s medicine. Not marketing.
Katie Taylor
December 29, 2025 AT 08:46I’ve been waiting my whole life for someone to say this out loud. IBS isn’t a curse-it’s a signal. And if you’re still on antispasmodics and calling it ‘management,’ you’re not healing-you’re surviving.
I did the low-FODMAP diet. I found my triggers. I started daily breathwork. I saw a hypnotherapist. And guess what? I haven’t had a flare-up in 14 months. Not because I’m lucky. Because I finally listened.
To everyone who says ‘it’s just stress’-you’re not just wrong. You’re dangerous. This isn’t in your head. It’s in your biology. And your biology is begging you to stop ignoring it.
Payson Mattes
December 30, 2025 AT 21:40Did you know the gut-brain axis is controlled by a secret government project called Project GutLink? They’ve been manipulating serotonin levels since 2008 to make people dependent on FODMAP diets and hypnotherapy apps. The real cure is a $27 device you can buy on AliExpress that zaps your colon with infrared waves. I’ve been using it for 3 weeks. My IBS is gone. My dog can now sense when I’m stressed. He barks at my phone.
Also, the NIH is lying. They’re funded by Big Pharma. The real research is on Reddit thread r/GutConspiracy. Check the pinned post. It’s all there. I’ve got screenshots.
And no, I won’t tell you the link. You have to find it yourself. It’s a test.
Isaac Bonillo Alcaina
December 31, 2025 AT 02:58You people are pathetic. You spend years chasing ‘biohacks’ and ‘neurofeedback’ while ignoring the root cause: weak willpower. IBS isn’t a neurological disorder-it’s a failure of discipline. Stop eating junk. Stop being lazy. Stop Googling ‘gut hypnotherapy’ like it’s a spa treatment.
I’ve had IBS since I was 14. I didn’t need a $300 therapist. I needed to stop eating pizza at 2 a.m. and start going to bed before midnight. That’s it. No jargon. No biomarkers. Just basic adulting.
If you can’t control your gut, you can’t control your life. Simple.
Steven Mayer
January 2, 2026 AT 01:57The serotonin hypothesis in IBS is oversimplified. While elevated mucosal 5-HT correlates with diarrhea-predominant symptoms, the mechanism is confounded by enterochromaffin cell density variations, mast cell activation, and bile acid malabsorption-all of which are rarely measured in clinical trials.
Moreover, the efficacy of gut-directed hypnotherapy is often attributed to non-specific therapeutic effects: attention, expectation, and the placebo response. The long-term durability cited in trials relies on self-reporting, not objective biomarkers.
And while the low-FODMAP diet reduces symptoms, it also depletes prebiotic fibers essential for microbial diversity, potentially exacerbating dysbiosis long-term. The article neglects this trade-off entirely.
Science is not a TED Talk. It’s a process of incremental, skeptical inquiry. This piece, while well-intentioned, leans dangerously into therapeutic reductionism.
Isaac Bonillo Alcaina
January 2, 2026 AT 07:31Wow. So now we’re blaming weak willpower? That’s what I’ve been hearing for 15 years. And look where it got me-depressed, isolated, and on a cocktail of meds that made me feel like a zombie.
You think I didn’t try ‘just eating better’? I did. I quit sugar. I stopped caffeine. I ate kale for breakfast. I meditated. I slept 8 hours. I still had pain. Because it’s not about discipline. It’s about biology.
And if your solution is ‘stop being lazy,’ then you’re not helping. You’re hurting. Go read the studies. Or better yet-live with it for a year. Then come back and talk.