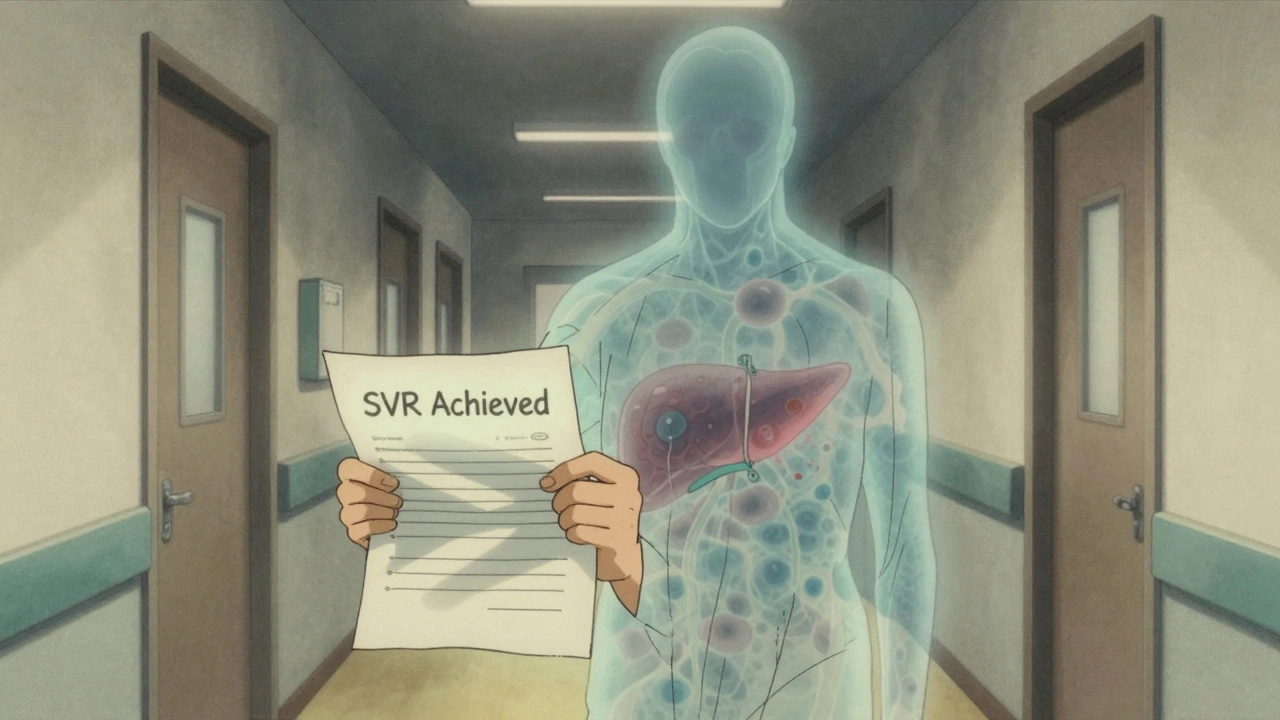
When you hear that hepatitis C has been cured, it’s natural to feel like the danger is over. After all, the virus is gone. Your liver is healing. You’re finally free from years of treatment, fatigue, and worry. But here’s the truth that many don’t hear: liver cancer risk after SVR doesn’t vanish just because the virus is gone.
Sustained Virologic Response (SVR) means the hepatitis C virus is undetectable in your blood 12 or 24 weeks after finishing treatment. That’s a win. Direct-acting antivirals (DAAs) cure over 95% of people. But curing the virus doesn’t mean your liver goes back to being a healthy, young liver. If you had advanced scarring-fibrosis or cirrhosis-before treatment, your risk of liver cancer remains real. And it’s higher than most people realize.
How Much Risk Is Left After a Cure?
Studies show that achieving SVR cuts your risk of liver cancer by about 71%. That sounds impressive-and it is. But that still leaves nearly 3 out of 10 people with some level of ongoing risk. And for those who already had cirrhosis, the numbers are more alarming.
In people with cirrhosis who achieved SVR, liver cancer still develops in about 2.1 to 2.3 cases per 100 people each year. Compare that to untreated cirrhotic patients, where the rate is 4.5 per 100 people annually. So yes, the risk dropped by more than half. But it didn’t disappear. That’s not a small number. It’s the difference between a rare event and something that still needs watching.
Why does this happen? Even after the virus is gone, the liver doesn’t reset. Scar tissue stays. Inflammation lingers. Certain biological pathways that drive cancer growth-like SPHK1 activation and abnormal cell cycles-don’t just shut off. The liver remembers the damage. And that memory can lead to tumors years later.
Who Still Needs Surveillance?
Not everyone needs ongoing liver cancer checks. But if you had advanced fibrosis (F3) or cirrhosis (F4) before treatment, you’re in the high-risk group. That’s the key. Your risk isn’t based on whether you had hepatitis C. It’s based on how much damage was already done.
Doctors use two main tools to measure that damage: transient elastography (FibroScan) and the FIB-4 index. After treatment, if your FibroScan reading is above 11.2 kPa, or your FIB-4 score is above 3.25, you’re still at elevated risk. These aren’t guesses-they’re proven thresholds backed by data from thousands of patients across multiple countries.
Here’s the catch: many people who had advanced fibrosis think they’re fine because their liver enzymes normalized or their symptoms disappeared. But those are not reliable signs. The real danger lies beneath the surface-in the scar tissue that doesn’t show up on blood tests.
Why Do Guidelines Differ So Much?
If you’ve talked to two doctors about this, you’ve probably heard two different answers. That’s because guidelines aren’t the same everywhere.
In Europe, the EASL recommends semiannual ultrasound scans for anyone with F3 or F4 fibrosis after SVR. In the U.S., AASLD says only people with cirrhosis (F4) need regular checks. They don’t recommend routine screening for those with advanced fibrosis alone.
Why the split? It comes down to risk tolerance and practical concerns. European experts worry that fibrosis can be misclassified-some people thought to have F3 actually have early cirrhosis. Missing a cancer because you skipped a scan is a far worse outcome than doing an extra ultrasound. Plus, ultrasounds are cheap, non-invasive, and widely available.
U.S. guidelines are more conservative. They argue that the absolute risk for F3 patients is low-around 0.5% per year-and that screening too broadly could lead to unnecessary stress, biopsies, and costs. But here’s the problem: low risk doesn’t mean no risk. And when liver cancer is caught late, survival rates drop sharply.
There’s no perfect answer. But the safest approach? If you had cirrhosis, keep getting screened. If you had advanced fibrosis, talk to your doctor. Don’t assume you’re in the clear.

The Real Problem: People Stop Getting Screened
The biggest threat isn’t the cancer risk-it’s the fact that most people stop showing up for scans.
Studies show that only about 25% of eligible patients get the recommended twice-yearly ultrasounds after achieving SVR. That’s not because they don’t care. It’s because they were never properly told the risk remains.
Patients hear: “You’re cured.” They assume that means “no more liver problems.” They stop seeing their hepatologist. They skip follow-ups. They feel fine. So why bother?
But here’s what no one tells them: liver cancer often grows silently. No pain. No symptoms. By the time you feel something, it’s usually too late. That’s why surveillance isn’t about feeling sick-it’s about catching cancer before it causes harm.
Health systems are starting to fix this. The Veterans Health Administration saw a 32% jump in screening rates after they set up automated reminders in their electronic records. Simple nudges-like text messages or appointment letters-make a huge difference.
What Does Surveillance Actually Look Like?
If you’re in the high-risk group, your screening plan is straightforward:
- Ultrasound of the liver every 6 months
- Alpha-fetoprotein (AFP) blood test, often done at the same time
That’s it. No needles, no fasting, no downtime. The ultrasound takes less than 15 minutes. It’s painless. It’s covered by most insurance plans.
Some newer tools are emerging. The GALAD score-combining age, gender, and three blood markers-has shown 85% accuracy in spotting early liver cancer in post-SVR patients. But it’s still mostly used in research settings. FibroScan results over time can also help. If your liver stiffness drops below 9.5 kPa after SVR, your risk may be low enough to extend screening to once a year. But that’s still being studied.
For now, stick to the basics. If you’ve been told to get screened, do it. Even if you feel fine. Even if you think you’re cured. Because you’re not fully out of the woods.

What’s Next? The Future of Liver Cancer Prevention
Researchers are working on smarter ways to manage this risk. One big idea: personalized surveillance. Instead of checking everyone every 6 months, what if we could adjust based on how your liver is healing?
Early data from Massachusetts General Hospital suggests that if your FibroScan drops below 9.5 kPa after SVR and stays there for a year, your cancer risk may be low enough to stretch screenings to once a year. That could cut unnecessary scans by nearly half for some F3 patients.
There’s also hope in blood tests that detect early cancer signals before tumors form. These aren’t ready for prime time yet, but they’re coming. Clinical trials are underway to see if we can safely stop surveillance altogether for patients whose livers show clear signs of healing.
For now, though, the message is clear: if you had cirrhosis or advanced fibrosis before hepatitis C treatment, you still need checks. Not because you’re not cured-but because your liver still carries the scars.
What Should You Do?
Here’s what to do right now:
- Check your medical records. Did you have F3 or F4 fibrosis before treatment?
- Ask your doctor: “Do I still need liver cancer screening?”
- If you’re unsure, get a FibroScan or FIB-4 test done. These are non-invasive and quick.
- Don’t skip your next ultrasound. Even if you feel great.
- Teach someone else. Someone you know might have been cured too-and they might not know the risk remains.
Liver cancer after hepatitis C cure is preventable-if you stay vigilant. You didn’t fight the virus for years just to let your guard down now. Keep watching. Keep showing up. Your liver still needs you.

Tejas Bubane
December 9, 2025 AT 14:28Let’s be real - if you had cirrhosis and think you’re ‘cured’ now, you’re living in a fantasy. The virus is gone, sure, but your liver is still a war zone with permanent damage. No amount of DAA magic turns scar tissue into a 20-year-old’s liver. Stop celebrating and start screening.
Sarah Gray
December 10, 2025 AT 11:01Actually, the data is far more nuanced than this post implies. The 71% risk reduction is statistically significant, but the absolute risk for F3 patients remains below 0.6% annually - well below the threshold for population-wide screening. The European approach is overly cautious, bordering on iatrogenic harm. Screening too broadly creates anxiety, false positives, and unnecessary biopsies - all while diverting resources from higher-yield interventions. Evidence-based medicine demands precision, not panic.
Maria Elisha
December 12, 2025 AT 02:26i just got svr last year and my doc said i dont need scans anymore because my enzymes are normal and i feel great. guess i’m just lucky? 😅
Angela R. Cartes
December 13, 2025 AT 02:12Ugh. Another ‘you’re not safe yet’ post. Look, I got cured, I’m not going to live in fear of a ghost tumor. I’ve had ultrasounds twice since SVR and they’re clean. My liver feels fine. My life feels fine. Why does everyone need to ruin the victory with doomscrolling? 🙄
Ajit Kumar Singh
December 14, 2025 AT 20:11in india we dont even have fibroscan machines in most cities and if we do its 5000 rupees and no insurance covers it so what do you want us to do just die quietly and hope for the best because your fancy american guidelines dont work here
Simran Chettiar
December 15, 2025 AT 18:45It is a profound truth that the human body does not possess the capacity to erase the memory of trauma even when the causative agent has been eradicated and this is especially true of the hepatic parenchyma which retains the epigenetic imprint of prior inflammatory insult and thus the potential for malignant transformation persists irrespective of virological clearance which is merely a biochemical marker and not a restoration of physiological integrity
Anna Roh
December 17, 2025 AT 14:25My dad had cirrhosis, got cured, stopped going for scans. Got diagnosed with stage 4 last year. He’s gone now. Don’t be him.
Katherine Chan
December 19, 2025 AT 09:43Thank you for writing this. I was one of those people who thought ‘cured’ meant ‘done.’ I started getting screened again after reading this. I’m alive today because I didn’t ignore it. You’re not just saving your liver - you’re saving your future. Keep showing up.
Raja Herbal
December 19, 2025 AT 10:31So let me get this straight - you’re telling me after all the suffering, the meds, the stigma, the years of feeling like a walking time bomb… I still have to go back to the clinic every six months like I’m on probation? Wow. What a victory.
Olivia Portier
December 21, 2025 AT 01:18Hey - if you’re reading this and you’re scared because you had fibrosis… you’re not alone. I was too. I thought I was fine. Then I got my first ultrasound and saw the scar tissue. It was terrifying. But I went back. And again. And again. Nothing found. That’s the point. It’s not about fear. It’s about peace of mind. You’ve already won the hardest part. Don’t quit now.
Jennifer Blandford
December 22, 2025 AT 12:38I cried reading this. Not because I’m scared - but because I wish someone had told me this three years ago. I stopped seeing my doctor after SVR. I thought I was done. I didn’t know my liver still needed me. I’m going back tomorrow. For everyone who feels like they’ve earned their freedom - you have. But freedom doesn’t mean forgetting. It means choosing to protect what you fought for.
Andrea Beilstein
December 22, 2025 AT 22:41What does it mean to be ‘cured’ if the body never forgets? We treat viruses like they’re bugs we squash - but the liver isn’t a clean slate. It’s a living archive. Every scar is a chapter. Every inflammation, a footnote. We celebrate eradication like it’s a clean ending - but some stories don’t end. They just change form. Surveillance isn’t paranoia. It’s reverence. For the body that carried you. For the years you thought you lost. For the future you’re still fighting for.