What’s Really Happening When Your MS Symptoms Flare Up?
If you have multiple sclerosis, you’ve probably felt it: sudden weakness, blurry vision, numbness, or a spike in fatigue. Your first thought? Relapse. But what if it’s not? What if your body isn’t having a new attack - it’s just reacting to something else?
Up to 25% of symptom flare-ups in MS aren’t true relapses at all. They’re called pseudorelapses - temporary worsening of old symptoms caused by external triggers, not new nerve damage. Mistaking one for the other can mean getting unnecessary steroids, facing side effects like high blood sugar or mood swings, and missing the real fix.
Here’s how to tell the difference - and what to do next.
True MS Relapse: New Damage, New Symptoms
A true MS relapse happens when your immune system attacks the myelin sheath around nerves in your brain or spinal cord. This causes new inflammation, new lesions, and new neurological symptoms - or a significant worsening of existing ones.
The key? Duration and no trigger. If your symptoms last more than 48 hours and there’s no clear cause like fever, infection, or heat, it’s likely a true relapse. Common signs include:
- Sudden loss of balance or coordination
- New weakness in one leg or arm
- Blurred or double vision (not just heat-related)
- Loss of bladder or bowel control
- Severe numbness or tingling that doesn’t fade
On an MRI, you’ll see new or active lesions - areas where the immune system has attacked. These show up as bright spots on contrast scans. That’s the smoking gun.
True relapses can leave lasting damage. Even if you recover, some nerve function may never fully return. Each relapse adds up over time, especially in the early years of MS.
Pseudorelapse: The Body’s False Alarm
A pseudorelapse feels just as real - but it’s not new damage. It’s your damaged nerves struggling to send signals because something in your body is throwing them off.
Think of it like a frayed wire. Normally, it still works. But when it gets too hot, too tired, or too stressed, it shorts out. Turn off the trigger, and it works again.
Common triggers include:
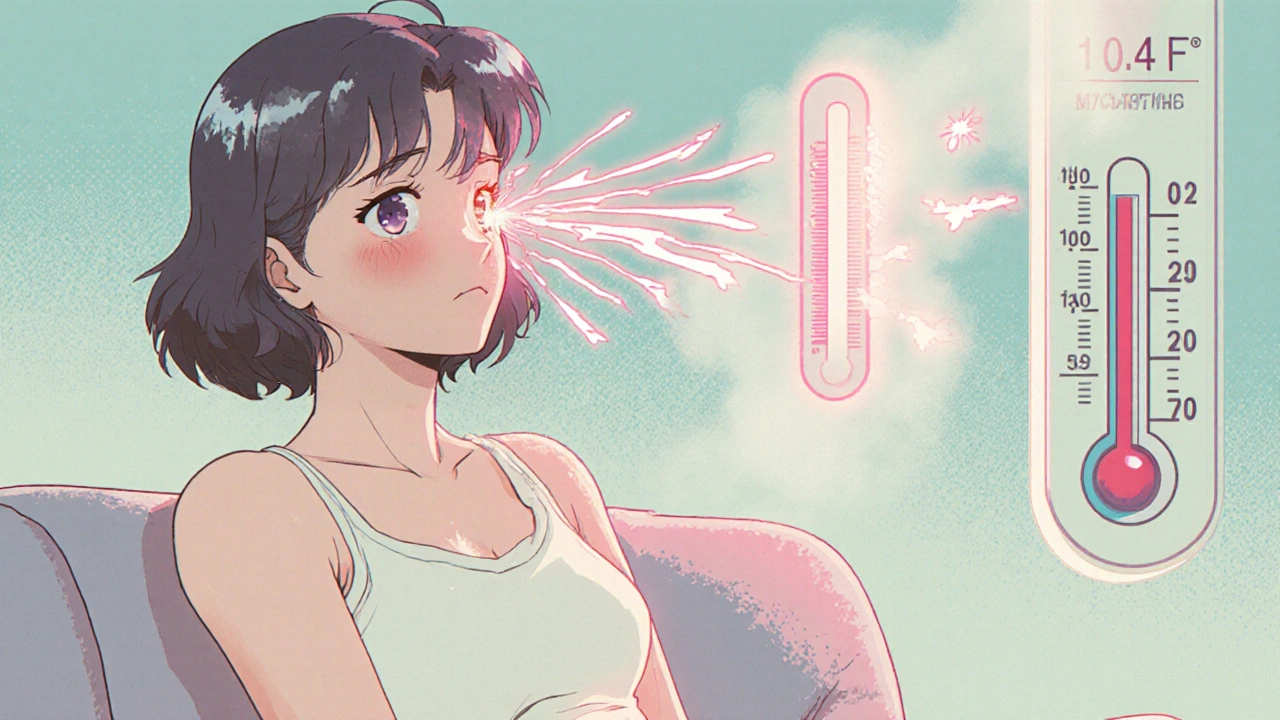
- Heat - Hot showers, summer weather, fever. Up to 80% of people with prior optic neuritis get Uhthoff’s phenomenon - vision blurs when body temperature rises.
- Urinary tract infections (UTIs) - The #1 trigger. In one study, 67% of pseudorelapses were linked to UTIs.
- Fever - Even a mild 100.4°F spike can make symptoms worse.
- Stress - Emotional or physical burnout can temporarily overload your nervous system.
- Exhaustion - Too much activity, poor sleep, or dehydration.
Here’s the big difference: pseudorelapse symptoms fade fast - usually within hours or a day - once the trigger is gone. No new lesions show up on MRI. No new damage is done.

Steroids: When They Help - and When They Don’t
High-dose IV methylprednisolone is the standard treatment for true relapses. It reduces inflammation, speeds up recovery, and helps you get back on your feet faster - especially if symptoms affect walking, bladder control, or vision.
Studies show about 70-80% of people see improvement with steroids. But only 45-55% fully recover. And the side effects? Real.
- Insomnia in 40%
- Mood swings or anxiety in 30%
- High blood sugar in 25%
- Increased risk of infection
Now, here’s the problem: steroids do nothing for pseudorelapses. No inflammation means no target for the drug. Giving steroids in these cases doesn’t help - it just risks harm.
Research shows 30-40% of pseudorelapses are mistakenly treated with steroids. One Reddit user, a nurse with MS, reported seeing five patients in a year get IV steroids for UTI-triggered flare-ups. One developed steroid-induced psychosis and had to be hospitalized.
That’s not just unnecessary - it’s dangerous.
How to Know for Sure: The 3-Step Check
Don’t guess. Use this simple process:
- Check duration. Did symptoms last less than 24 hours? Likely a pseudorelapse. More than 48? Could be a true relapse.
- Rule out triggers. Did you have a fever? A UTI? A hot day? Take your temperature. Get a urine test. Check your blood sugar and sodium levels. These are quick, cheap, and critical.
- Consider an MRI. If you’re still unsure, an MRI with contrast can show new lesions. No new lesions? Probably not a true relapse.
Many neurologists now use the MS-Relapse Assessment Tool (MS-RAT), which scores symptoms, duration, temperature, and function to give a probability of true relapse vs. pseudorelapse. It’s 92% accurate.
Who’s Most at Risk for Pseudorelapses?
It’s not random. People with:
- Longer disease duration (10+ years)
- Higher baseline disability
- History of optic neuritis (for Uhthoff’s phenomenon)
- Older age (over 55)
are more likely to experience pseudorelapses. Why? Because their nervous system has more damaged pathways. Even small stressors can overload them.
But here’s the catch: older patients with pseudorelapses sometimes don’t bounce back fully - not because of nerve damage, but because of deconditioning. After a week of weakness, they lose muscle tone. They don’t move as much. Recovery takes longer - even after the trigger is gone.

What to Do When It Happens
Don’t panic. Don’t rush to the ER for steroids.
For a suspected pseudorelapse:
- Cool down. Use cooling vests, cold drinks, air conditioning. For Uhthoff’s, symptoms often vanish in under two hours.
- Treat the trigger. Antibiotics for a UTI. Rest for exhaustion. Hydration for dehydration.
- Track it. Keep a simple log: date, symptoms, temperature, possible triggers, how long it lasted. This helps your neurologist spot patterns.
For a true relapse:
- Call your neurologist ASAP.
- Don’t wait to see if it gets worse.
- Be ready to discuss functional impact - can you walk? Use your hands? Control your bladder?
Why This Matters Beyond the Symptoms
Misdiagnosing a pseudorelapse as a true relapse doesn’t just waste time and money - it harms your body.
The National MS Society estimates that unnecessary steroid treatments for pseudorelapses cost the U.S. healthcare system over $12 million a year. That’s millions in IV drugs, hospital visits, and side effect management.
But the real cost? Trust. When patients get steroids they don’t need, they start to doubt their doctors. When they’re told it’s "just stress" and their symptoms don’t improve, they feel dismissed.
Accurate diagnosis builds confidence - in your care, in your body, and in your ability to manage MS.
What You Can Do Today
You don’t need to wait for your next appointment to take control.
- Download a symptom tracker app or use a notebook. Record triggers every time symptoms flare.
- Keep a thermometer and urine dipsticks at home. Test at the first sign of trouble.
- Ask your neurologist: "Can we review my relapse history and triggers together?"
- If you’ve had a pseudorelapse before, tell your ER doctor or primary care provider. Many don’t know the difference.
MS is complex. But knowing the difference between a relapse and a pseudorelapse gives you power - not just over your symptoms, but over your treatment.

Joseph Townsend
November 17, 2025 AT 11:00Okay but let’s be real - if your doctor can’t tell a pseudorelapse from a real one, maybe they shouldn’t be treating MS patients? I had a flare that lasted three days, got steroids, and woke up feeling like a caffeinated raccoon on a sugar high. Turned out I had a UTI. No new lesions. Just my nerves throwing a tantrum because I drank lukewarm coffee. Steroids didn’t fix my bladder, they fixed my anxiety… by making me cry at a commercial for laundry detergent. 🤡
Bill Machi
November 19, 2025 AT 01:08This article is an example of the dangerous over-medicalization of everyday human experience. In my view, the entire concept of pseudorelapse is a liberal construct designed to avoid accountability in healthcare. The immune system doesn’t ‘misfire’ - it responds. If you’re symptomatic, you’re having a relapse. The notion that heat or stress can mimic MS damage is pseudoscience masquerading as compassion. Steroids are a proven tool - use them. Stop overthinking. Stop coddling. Get strong or get out.
Elia DOnald Maluleke
November 19, 2025 AT 10:33One cannot help but contemplate the ontological weight of this distinction - between the new lesion and the temporary collapse of signal integrity. Is the body not a cathedral of broken circuits, each scar a hymn to survival? To label a flare as ‘pseudo’ is to diminish the lived reality of suffering - even when the damage is not new, the pain is not false. The nervous system remembers. The soul remembers. Perhaps the true relapse is not in the MRI, but in the doctor’s refusal to see the whole person - only the scan.
satya pradeep
November 19, 2025 AT 22:40Bro this is gold. I had a pseudorelapse last summer after hiking in 40°C heat. Legs went numb, vision went blurry - thought I was dying. Took a cold shower, drank electrolytes, slept 10 hours. All gone by morning. No steroids. No ER. Just common sense. Also, UTIs are the hidden monsters here. If you have MS and feel weird? Pee test first. Always. Save your liver from steroid chaos. Also, get a cheap thermometer and a urine strip kit - they cost less than a Starbucks latte. Worth it.
Prem Hungry
November 20, 2025 AT 23:46Dear friend, your dedication to understanding your condition is truly inspiring. I commend you for taking proactive steps to distinguish between relapse and pseudorelapse. It is through such mindful observation that we reclaim agency over our health. May I suggest you maintain a digital log - perhaps using Google Sheets - to track temperature, hydration, sleep, and symptom duration? This data will empower your neurologist to tailor your care with precision. You are not alone in this journey.
Leslie Douglas-Churchwell
November 22, 2025 AT 11:03Let’s be honest - this is Big Pharma’s quiet war on personal responsibility. 🧠💉 They want you to believe your body is broken so you’ll keep taking drugs. Steroids? Totally unnecessary. And why do you think UTIs are so common in MS patients? Because the immune system is compromised by YEARS of immunosuppressants - which were prescribed based on flawed MRI interpretations. The real trigger? The pharmaceutical-industrial complex. They profit from misdiagnosis. And the ‘MS-RAT’? Probably patented by a drug company. 🤫 #MSawareness #SteroidsAreNotTheAnswer
shubham seth
November 23, 2025 AT 09:07Look, this whole pseudorelapse thing is just a fancy way of saying ‘your nerves are trash.’ And yeah, heat and UTIs trigger it - but guess what? So does being lazy. You think your body’s ‘overloaded’? Maybe you’re just not moving enough. You sit around all day, eat junk, skip rehab, then blame the weather when your legs give out. Steroids don’t fix laziness. Movement does. Get off the couch. Hydrate. Walk. Stop waiting for a doctor to tell you it’s ‘not a relapse’ - your body’s screaming for you to stop being a victim.
Kathryn Ware
November 24, 2025 AT 09:01Thank you for writing this - seriously. As someone who’s had 3 pseudorelapses misdiagnosed as true ones, I can’t tell you how relieved I was to finally understand what was happening. I used to feel like I was making it up, or that my neurologist thought I was ‘hysterical.’ Now I keep a daily log on my phone - temperature, sleep, hydration, mood, and symptom intensity. Last month, I caught a UTI before I even felt pain - just because my urine strip turned pink. I took antibiotics, cooled down, and within 12 hours, the numbness vanished. No IV, no side effects, no panic. I wish I’d known this 5 years ago. To anyone reading: your symptoms are real, even if they’re not new damage. And you deserve to understand why. 💙