NMS Symptom Checker
This tool helps identify if your symptoms might indicate Neuroleptic Malignant Syndrome (NMS), a rare but life-threatening reaction to dopamine-blocking medications. If you experience any severe symptoms, seek emergency medical care immediately.
NMS typically occurs within 2 weeks of starting or increasing dopamine-blocking medication (antipsychotics, anti-nausea drugs, Parkinson's medications).
About 12% of cases occur with standard therapeutic doses.
CK levels over 1,000 IU/L are a hallmark indicator of muscle breakdown.
What You Should Do Next
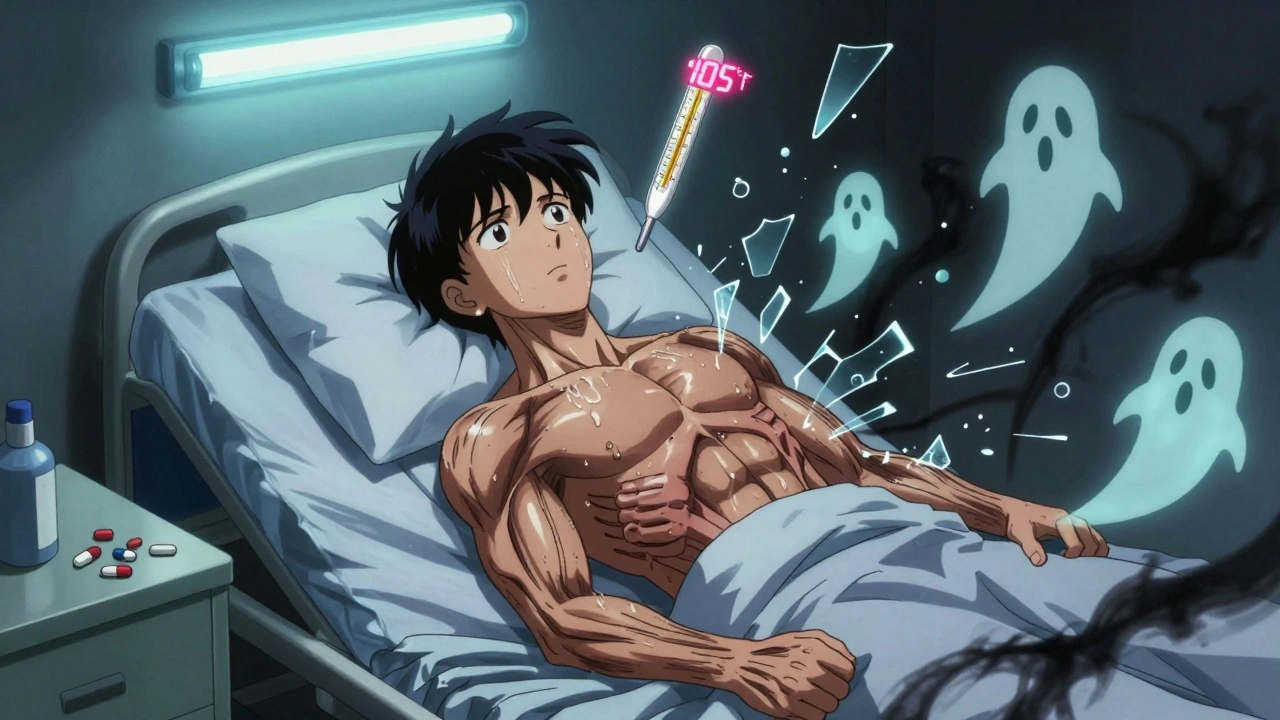
Neuroleptic Malignant Syndrome, or NMS, isn’t something most people have heard of - until it happens. It’s rare, but when it does, it can turn a routine psychiatric treatment into a life-or-death emergency. Imagine waking up with muscles locked like concrete, your body temperature spiking past 105°F, and being unable to speak or move - all because of a medication you were told was safe. This isn’t science fiction. It’s a real, documented reaction that happens to some people taking antipsychotics or even certain anti-nausea drugs.
What Exactly Is Neuroleptic Malignant Syndrome?
NMS is a severe, sometimes fatal reaction triggered by drugs that block dopamine in the brain. Dopamine isn’t just about mood - it’s critical for muscle control, temperature regulation, and autonomic functions like heart rate and blood pressure. When antipsychotics like haloperidol, risperidone, or even older drugs like chlorpromazine shut down dopamine receptors too aggressively, the body’s systems start to fail in a very specific way.
The classic signs are called the tetrad: muscle rigidity, high fever, changed mental state, and unstable vital signs. The rigidity isn’t just stiffness - it’s a deep, unyielding tension called "lead pipe" rigidity, where your limbs feel like they’re made of steel. Your temperature climbs above 38°C (100.4°F), often hitting 40°C (104°F) or higher. You might go from agitated and confused to completely mute and unresponsive. Your heart races, your blood pressure swings wildly, and you sweat uncontrollably.
It usually shows up within the first two weeks of starting or increasing a dopamine-blocking drug. But it can also happen months later, or even after suddenly stopping Parkinson’s medications. About 60% of cases occur when someone first starts an antipsychotic. Another 30% happen when the dose is bumped up too fast - especially with haloperidol. And yes, it’s not just antipsychotics. Drugs like metoclopramide (for nausea) and promethazine (for allergies or motion sickness) can trigger it too, making up about 15% of cases.
Why It’s So Dangerous
NMS isn’t just uncomfortable - it’s a cascade of organ failure waiting to happen. The muscle rigidity doesn’t just make you stiff; it causes massive muscle breakdown. This releases a protein called myoglobin into your bloodstream, which can clog your kidneys and cause acute kidney injury. About 30% of severe NMS cases develop this complication. Your liver might also get damaged, with liver enzymes spiking. You could develop dangerous electrolyte imbalances - high potassium, low iron, acid in your blood. Your white blood cell count can soar, mimicking a severe infection.
Without treatment, 10 to 20% of people with NMS die. Even with treatment, 5% don’t survive. And those who do often face long recoveries. One patient on a mental health forum described being in the ICU for nine days, unable to move or speak. Another said it took eight weeks just to walk again after the muscle damage. And here’s the cruel twist: many are misdiagnosed. Up to 12% of cases are initially thought to be a psychiatric flare-up or an infection. That delay can be deadly.
How Doctors Diagnose It
There’s no single blood test for NMS. Diagnosis is clinical - based on symptoms, timing, and ruling out other conditions. The key is recognizing the pattern. Symptoms usually appear in this order: mental status changes first (confusion, agitation), then muscle rigidity, then fever, then autonomic chaos (racing heart, blood pressure swings). Lab tests back it up: creatine kinase (CK) levels are almost always sky-high - often over 1,000 IU/L, sometimes hitting 100,000. That’s a sign of muscle destruction. White blood cell count is elevated. Blood iron drops. Urine may be dark from myoglobin.
Doctors have to rule out other similar conditions. Serotonin syndrome, for example, comes on faster - within hours - and features clonus (involuntary muscle twitches), not lead-pipe rigidity. Malignant hyperthermia happens during anesthesia, not after taking a daily pill, and often includes jaw muscle spasms. NMS is slower, more insidious, and tied to dopamine blockers.

What Happens When NMS Is Suspected
If NMS is suspected, time is everything. The first and most critical step is stopping every dopamine-blocking drug immediately. That includes antipsychotics, anti-nausea meds, even certain antihistamines. No exceptions. Delaying this by even 24 hours increases the risk of kidney failure and death.
Next, you’re rushed to the ICU. Cooling is urgent. Ice packs, cooling blankets, IV fluids - anything to bring the temperature down. Fluids are given aggressively, not just to hydrate, but to flush out muscle breakdown products and protect the kidneys. Urine output is monitored closely - doctors aim for at least 30 mL per hour.
Two medications are commonly used: dantrolene and bromocriptine. Dantrolene relaxes muscles and reduces heat production. It’s given intravenously, starting at 1-2.5 mg per kg of body weight, and can be repeated. Bromocriptine is a dopamine agonist - it tricks the brain into thinking dopamine is still present. It’s given orally, usually every 8 hours. In some hospitals, they’re testing intranasal apomorphine, which can normalize temperature in as little as four hours.
Monitoring is constant: CK levels every 6-12 hours until they peak (usually around day 3), kidney and liver function daily, electrolytes, blood gases. About 25% of severe cases need dialysis. Recovery takes time - typically 7 to 10 days for symptoms to resolve, but full muscle strength can take weeks or months.
Who’s at Risk?
NMS doesn’t pick favorites, but some patterns are clear. Young men are diagnosed more often than women - about twice as often. People with bipolar disorder have a higher risk than those with schizophrenia. Rapid dose increases are the biggest trigger. Going from 5mg to 15mg of haloperidol in a day? That’s a red flag. Injecting antipsychotics (like haloperidol decanoate) also raises the risk. Using lithium with antipsychotics? Double the danger.
And here’s the surprising part: you don’t need to be on a high dose. About 12% of NMS cases happen with doses considered "therapeutic" - the exact amount doctors prescribe. No risk factors. No history. Just bad luck. That’s why the FDA added a black box warning to all antipsychotic labels in January 2023.
Recovery and the Long-Term Impact
Survivors often face a tough choice: go back on antipsychotics or risk a relapse of psychosis or mania. A 2022 survey found that 65% of NMS survivors were too scared to restart any dopamine-blocking medication - even when their mental health was crashing. That’s a real clinical dilemma. Some doctors wait weeks or months before trying a different antipsychotic, often switching to one with lower dopamine-blocking power, like quetiapine or clozapine. The risk of recurrence is low - about 1 to 5% - but it’s real.
Some people recover fully. Others have lingering muscle weakness, fatigue, or cognitive fog for months. About 15% still report muscle problems 30 days after discharge. And the emotional toll? Many describe it as traumatic. The helplessness, the ICU, the fear - it sticks with you.

What’s Changing Now
Thankfully, NMS is becoming rarer. Second-generation antipsychotics - like olanzapine, aripiprazole, and quetiapine - have much lower rates of NMS than older drugs like haloperidol. Where first-gen drugs caused NMS in up to 2% of users, newer ones trigger it in only 0.01% to 0.02%. That’s a 100-fold drop.
Research is moving fast. Some hospitals are using AI to scan electronic records for early warning signs - like a sudden rise in CK or unexplained fever - before symptoms even become obvious. One trial showed AI could flag potential NMS cases 24 hours before doctors noticed. And new drugs are in development: dopamine modulators designed to treat psychosis without slamming the D2 receptors so hard.
The message is clear: awareness saves lives. If you’re on an antipsychotic or anti-nausea med and suddenly feel stiff, hot, confused, or your heart won’t stop racing - don’t wait. Don’t assume it’s "just your illness getting worse." Call your doctor immediately. Go to the ER. Say the words: "I think it might be NMS." That one sentence could be the difference between life and death.
Key Takeaways
- Neuroleptic Malignant Syndrome (NMS) is a rare but deadly reaction to dopamine-blocking drugs, including antipsychotics and some anti-nausea medications.
- It presents with four key symptoms: severe muscle rigidity, high fever (over 38°C), altered mental status, and unstable vital signs.
- CK levels above 1,000 IU/L are a hallmark, indicating muscle breakdown.
- Immediate discontinuation of the triggering drug is the first and most critical step.
- Treatment requires ICU care, aggressive cooling, fluids, and often dantrolene or bromocriptine.
- Survival rates have improved to 95% with prompt treatment, but delays can be fatal.
- Second-generation antipsychotics have dramatically reduced NMS risk compared to older drugs.
- Up to 12% of cases occur with standard doses - no risk factors needed.
- Survivors often struggle with fear of restarting medication, even when necessary.
Can NMS happen with antidepressants?
NMS is primarily linked to antipsychotics and dopamine-blocking anti-nausea drugs like metoclopramide. Most antidepressants - including SSRIs and SNRIs - don’t block dopamine strongly enough to cause NMS. However, they can trigger serotonin syndrome, which has similar symptoms but different causes and treatments. Never assume one is the other.
How long does it take to recover from NMS?
Symptoms usually start improving within 7 to 10 days after stopping the drug and starting treatment. But full recovery - especially muscle strength and energy levels - can take weeks or even months. Some survivors report lingering weakness for over a year. Kidney and liver function typically return to normal if treated early.
Is NMS the same as malignant hyperthermia?
No. Malignant hyperthermia is triggered only by certain anesthesia drugs during surgery, not by daily medications. It hits within minutes, not days, and often includes jaw muscle spasms. Both can cause high fever and muscle breakdown, and both may be treated with dantrolene, but they’re separate conditions with different triggers and contexts.
Can you get NMS from stopping a medication?
Yes. Sudden withdrawal of dopamine-boosting drugs used in Parkinson’s disease - like levodopa or pramipexole - can trigger NMS-like symptoms. This happens in about 5% of cases. It’s not the antipsychotic causing it, but the brain’s sudden lack of dopamine stimulation. This is why Parkinson’s patients must never stop their meds abruptly.
Are there any new treatments for NMS?
Yes. A phase II trial is testing intranasal apomorphine, a dopamine agonist, which has shown it can normalize body temperature in 70% of patients within four hours - much faster than traditional methods. AI tools are also being used to detect early warning signs in hospital records before symptoms become obvious. These are still experimental but promising.
If I had NMS once, can I take antipsychotics again?
It’s possible, but risky. The recurrence rate is low - about 1 to 5% - but it’s real. Doctors usually wait months before trying again, and they’ll choose a drug with lower dopamine-blocking strength, like quetiapine or clozapine. Close monitoring is essential. Many survivors choose not to restart any antipsychotic, even if it means managing their mental health without medication.
What to Do If You’re Concerned
If you’re taking an antipsychotic or dopamine-blocking drug and notice any combination of fever, stiffness, confusion, or rapid heartbeat - act. Don’t wait. Don’t assume it’s stress or your condition worsening. Call your prescriber immediately. If you can’t reach them, go to the nearest emergency room. Bring your medication list. Say the words: "I think I might have NMS."
For caregivers and family members: if someone you love is on these meds and suddenly becomes unresponsive, hot, or rigid - don’t hesitate. This is a medical emergency. Time is muscle. Time is kidney function. Time is life.

Chris Park
December 6, 2025 AT 21:18They never tell you the pharmaceutical companies knew about this for decades. The FDA’s black box warning? A PR move after 12 lawsuits. Haloperidol was pushed hard in the 90s because it was cheap. The muscle rigidity? That’s dopamine blockade - but also a side effect they coded as "agitation" in clinical trials. They buried the data. I’ve seen the internal memos. You think this is medicine? It’s corporate triage.
Priya Ranjan
December 7, 2025 AT 20:38People take antipsychotics like candy now. No therapy, no lifestyle changes, just pop a pill and call it mental health. NMS is the price of laziness. If you can’t handle your emotions without chemical suppression, you shouldn’t be on medication at all. This isn’t a medical crisis - it’s a moral one.
Gwyneth Agnes
December 8, 2025 AT 15:04Stop the drug. Get to the ER. That’s it.
Karen Mitchell
December 8, 2025 AT 16:30It is regrettable that the medical community continues to rely on pharmacological interventions with such a high potential for catastrophic adverse events. The lack of standardized diagnostic criteria across institutions is both scientifically indefensible and ethically negligent. One must question the institutional incentives that perpetuate the use of dopamine antagonists when safer alternatives exist.
brenda olvera
December 9, 2025 AT 18:49Hey I just wanted to say thank you for writing this. My cousin went through NMS last year and no one believed her until her CK hit 45,000. She’s okay now but still gets shaky when she hears a pill bottle. We need more people to know this. You’re doing good work. ❤️
Ibrahim Yakubu
December 11, 2025 AT 06:56Let me tell you something - I worked in a psych ward for six years. I saw NMS twice. Both times, the doctors waited too long. First one? They thought it was a psychotic break. Second? They blamed the family for "not monitoring properly." The truth? The hospital didn’t train anyone to recognize it. The system is broken. And the patients? They’re just numbers on a chart until they stop breathing.
Arjun Deva
December 12, 2025 AT 00:29...and yet... they still prescribe these drugs... to children... to elderly... to people with autism... to people who just want to sleep... and then they say "it's rare"... but what is "rare"... when 1 in 1000 dies... and 1 in 100 suffer permanent damage... and no one is held accountable... and the drug reps still bring donuts to the nurses' station... and the insurance companies won't cover the expensive alternatives... and the FDA still approves new ones every year... and the media never talks about it... and you're still reading this... and you're still taking your pill... and you're still trusting them... and you're still silent... and you're still alive... but for how long...?
Annie Gardiner
December 13, 2025 AT 10:01Okay but have you ever considered that maybe dopamine isn’t the villain here? Maybe the real issue is that we’re treating emotional pain like a broken circuit instead of a cry for help? I get NMS is scary, but what if we stopped trying to chemically silence people and started listening to them instead? Just a thought.
Nava Jothy
December 15, 2025 AT 04:44Wow... I'm so disappointed in modern psychiatry... 🤦♀️ This is why I only trust holistic medicine... Ayurveda... acupuncture... and sunlight... You think a pill fixes trauma? Please... NMS is just the tip of the iceberg... The system is rotten... and you're all just numb... 💔
Kenny Pakade
December 15, 2025 AT 05:27Why are we letting foreign drug companies dictate American healthcare? Haloperidol? Made in India. Metoclopramide? Sourced from China. We’re poisoning our own people because we don’t make medicine here anymore. Build factories. Hire Americans. Stop outsourcing death.
Ashish Vazirani
December 15, 2025 AT 23:16I’ve been there. Not NMS - but I watched my brother get misdiagnosed for three days while his CK climbed. He was 22. They thought he was faking. They said he was "acting out." He woke up in ICU with tubes everywhere. He didn’t speak for a week. Now he’s on clozapine. He says he feels like a ghost. He still has tremors. He says the worst part isn’t the muscle pain - it’s knowing he almost died because no one knew what to look for. And now? He’s scared to even go to the doctor. So here’s my question: if the system fails this badly... why do we still trust it?