After a colonoscopy finds and removes polyps, many people wonder: When do I need to go back? It’s not a one-size-fits-all answer. The timing depends on what kind of polyps were found, how many, how big they were, and how they looked under the microscope. Getting this right matters - too soon, and you’re wasting time, money, and comfort. Too late, and you risk missing something serious.
Why Surveillance Intervals Even Exist
Colon polyps aren’t cancer - but some can turn into cancer over time. The goal of follow-up colonoscopies isn’t to check if the old polyps came back. It’s to catch new ones early, before they become dangerous. Most colorectal cancers develop slowly, over 10 to 15 years, from small, harmless-looking growths. That’s why surveillance isn’t about panic - it’s about smart timing.
Guidelines from major medical groups like the US Multi-Society Task Force (USMSTF), the British Society of Gastroenterology (BSG), and the European Society of Gastrointestinal Endoscopy (ESGE) are based on decades of research. They track thousands of patients after polyp removal to see who develops cancer later. The data shows that for many people, waiting longer between colonoscopies is not only safe - it’s better.
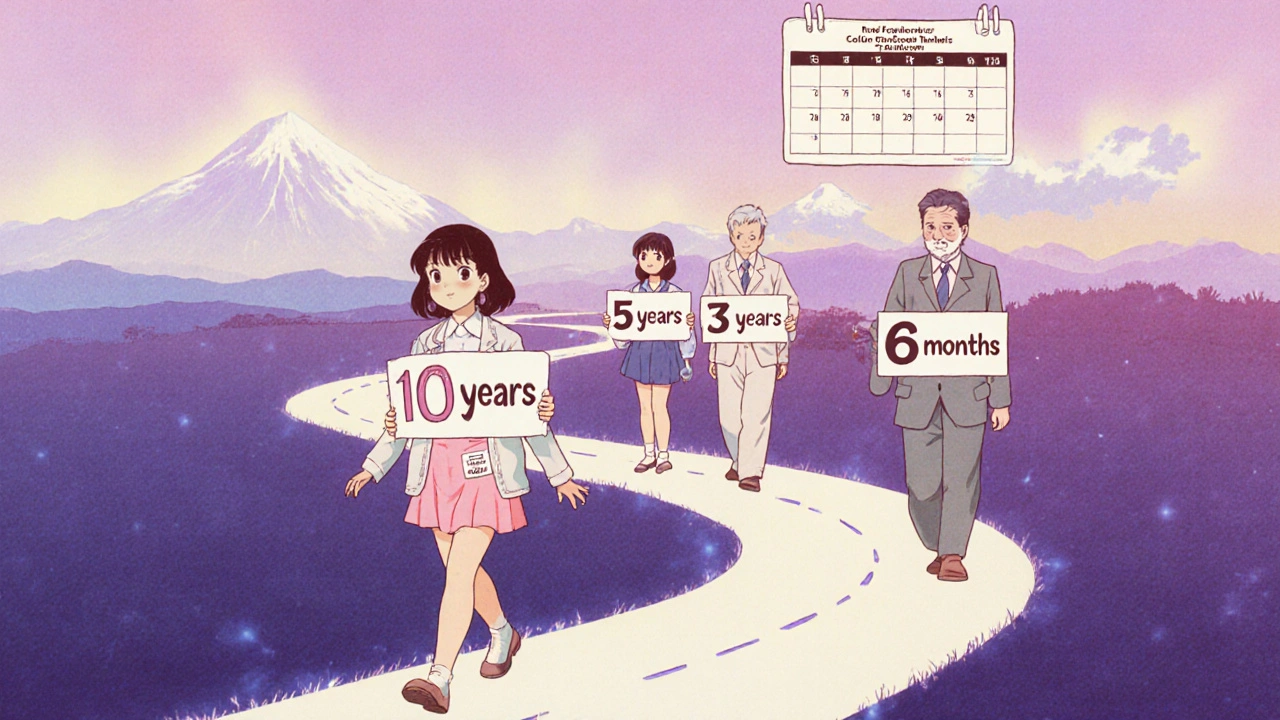
Low-Risk Polyps: You Might Wait 7 to 10 Years
If your colonoscopy found just one or two small adenomas (the most common type of pre-cancerous polyp) that were less than 10 mm in size, you’re in the lowest risk group. Under the 2020 USMSTF guidelines, you don’t need another colonoscopy for 7 to 10 years. That’s a big change from the old 5-year rule.
Why the shift? Studies show people with 1-2 small adenomas have nearly the same cancer risk over 10 years as someone with a completely normal colonoscopy. One major study found 99.3% of these patients remained cancer-free at the 10-year mark - almost identical to those with no polyps at all.
Even if you’re in the UK, the BSG/ACPGBI guidelines say you can wait more than 10 years if you only had one or two tiny adenomas. Many European doctors now feel comfortable stretching the interval even further, especially if your bowel prep was good and the polyps were fully removed.
More Polyps? Shorter Wait Times
If your doctor found three or four adenomas - all under 10 mm - the recommendation drops to 3 to 5 years. This isn’t because these polyps are more dangerous. It’s because having more of them suggests your colon might be more prone to developing new ones.
Five or more adenomas of any size? That’s a red flag. You’ll need a repeat colonoscopy in 3 years. Same goes if any polyp was 10 mm or larger, even if it was just one. Size matters. A 12 mm adenoma carries a higher chance of containing early cancer cells than a 5 mm one.
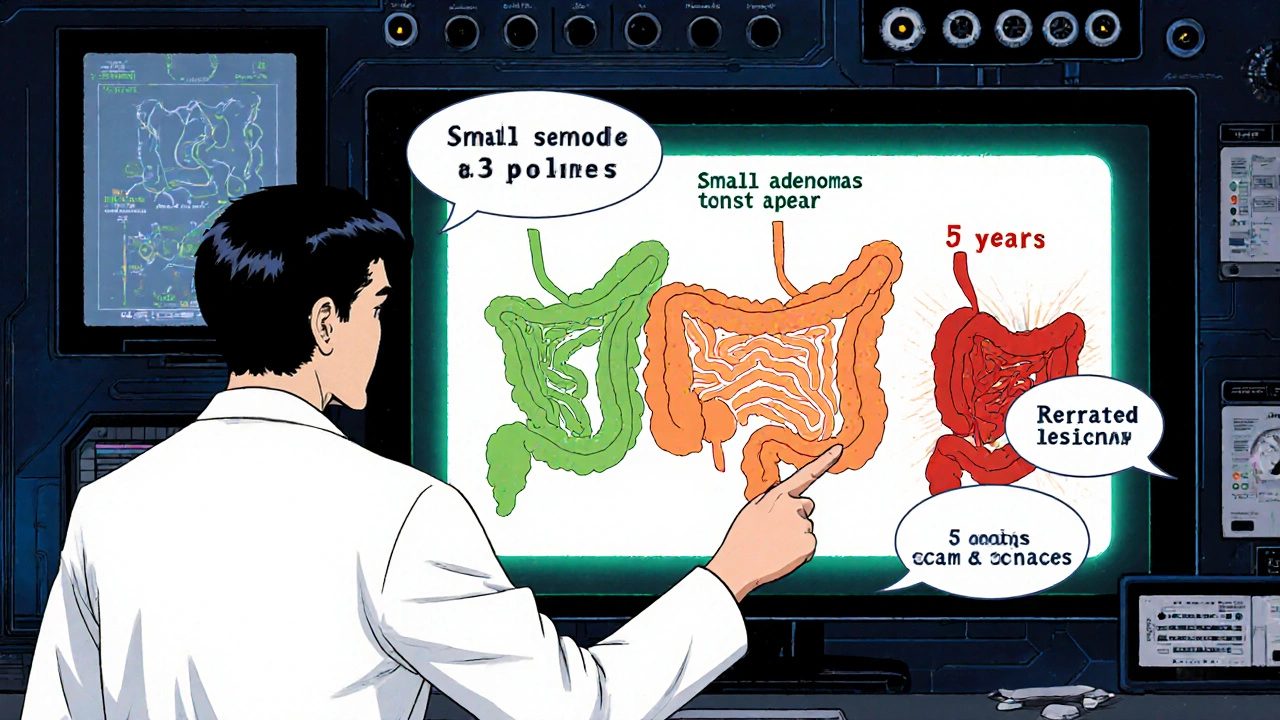
High-Risk Features: The 3-Year Rule
Some polyps look scary under the microscope - even if they’re small. If any polyp had villous features, high-grade dysplasia, or was a traditional serrated adenoma, you’re in the high-risk group. You’ll need a repeat colonoscopy in 3 years, no matter how many there were or how big they were.
Same goes for sessile serrated lesions (SSLs), especially if they’re 10 mm or larger. SSLs are trickier than regular adenomas. They’re flatter, harder to spot, and can turn into cancer faster. If you had one SSL that was 10 mm or bigger, 3 years is the minimum wait. If you had 3 to 4 SSLs under 10 mm, go back in 3 to 5 years. Five or more? Back in 3 years.
Here’s a key point: if your doctor isn’t sure whether a small polyp is a hyperplastic polyp (harmless) or an SSL (potentially risky), they’ll treat it like an SSL. Better safe than sorry.
Large Polyps and Piecemeal Removal: The 6-Month Rule
If a polyp was bigger than 20 mm and had to be removed in pieces - not in one go - you’re at higher risk for leftover tissue or missed areas. The USMSTF, Japanese, and Korean guidelines all say: come back in 6 months. This isn’t about cancer yet. It’s about making sure every bit of the polyp was taken out.
The UK’s BSG/ACPGBI guidelines are more cautious. They recommend two follow-ups: one at 2 to 6 months to check for healing and residual tissue, and another at 18 months to confirm no new growths. This extra step can feel overwhelming, but it’s designed to catch anything early.
European guidelines (ESGE) give a range: 3 to 6 months. That flexibility lets doctors adjust based on how clean the resection looked and whether the bowel prep was excellent. If the view was poor or the polyp was messy, they’ll lean toward 3 months.
Serrated Polyposis Syndrome: Annual Checks
This is rare, but serious. If you have serrated polyposis syndrome - meaning you have 20 or more serrated polyps total, or at least 5 that are 10 mm or larger - you need annual colonoscopies. The American guidelines say this until age 75. The UK says 1 to 2 years, but if you go 2 years and find no polyps larger than 10 mm, they might stretch it.
It’s not just about counting polyps. It’s about the pattern. If your family has a history of this, or if you’ve had multiple polyps removed over several years, your doctor should be thinking about this diagnosis. Genetic testing might be offered.
Why So Many Doctors Get It Wrong
Even though the guidelines are clear, many doctors still recommend 5-year intervals for low-risk polyps. A 2020 study at a Veterans Affairs hospital found only 18.6% of gastroenterologists followed the updated 7-10 year rule. Most stuck with the old advice.
Why? Fear. Fear of missing something. Fear of lawsuits. Fear that patients won’t come back if they’re told to wait too long. One doctor in the study admitted he recommends 7 years for small adenomas - not 10 - because it feels safer to him.
Another problem? Confusion around serrated polyps. A 2022 survey found only 28.5% of US gastroenterologists correctly knew the interval for small SSLs. Many thought they needed 3-year checks, when 5-10 years is often enough.
Patients get caught in the middle. Your primary care doctor might tell you to come back in 5 years because that’s what they remember. Your gastroenterologist says 7. Who do you believe?
Tools That Help - And What You Should Ask For
There are digital tools now that make this easier. Polyp.app, developed by Massachusetts General Hospital, lets doctors input polyp details and instantly get the right interval. Many hospitals now have EHR systems (like Epic or Cerner) that auto-suggest follow-up dates based on what was found.
But not all systems are updated. Not all doctors use them. So here’s what to do after your colonoscopy:
- Ask for a written summary of what was found - including number, size, and type of polyps.
- Ask: “Based on the 2020 USMSTF guidelines, what’s my recommended interval?”
- Ask: “Were any polyps serrated or had high-grade dysplasia?”
- Ask: “Will this be entered into my electronic record so my next doctor knows?”
If they can’t answer, ask for a referral to a specialist who follows current guidelines. Don’t assume your next appointment is automatic. You need to be the one to keep track.
The Future: Personalized Screening
The next big shift won’t be based on polyp counts anymore. Researchers are testing blood and stool tests that look for DNA changes linked to cancer risk. One trial (NCT04567821) is testing if a simple biomarker test can tell you whether you need a colonoscopy in 3 years or 10.
Imagine a future where your interval isn’t based on how many polyps you had - but on your unique biology. Your age, family history, gut bacteria, and genetic markers could all help tailor your screening. This isn’t science fiction. It’s happening now.
For now, stick to the facts. Know what was found. Know the guidelines. And don’t let outdated advice keep you coming back too soon - or too late.
How long should I wait for my next colonoscopy after having one small adenoma removed?
If you had just one small adenoma (less than 10 mm) and no other high-risk features, current US guidelines recommend waiting 7 to 10 years. In the UK and Europe, some doctors may suggest even longer - up to 12 years - if the polyp was very small and the colon was otherwise clean. Always get your results in writing and confirm the interval with your doctor.
What if I had three polyps removed? Do I need a colonoscopy every 3 years?
If all three were small (under 10 mm) and were regular adenomas (not serrated or dysplastic), the recommended interval is 3 to 5 years. But if any were 10 mm or larger, had villous features, or were serrated lesions, you’ll need a repeat colonoscopy in 3 years. The number alone doesn’t decide it - the type and size matter more.
Are serrated polyps more dangerous than regular adenomas?
They can be. Sessile serrated lesions (SSLs) are harder to spot during colonoscopy and can turn into cancer faster than traditional adenomas - especially if they’re 10 mm or larger. Even small SSLs (under 10 mm) need careful follow-up. If you had one or two small SSLs, wait 5 to 10 years. Three to four? Go back in 3 to 5 years. Five or more? Back in 3 years. Don’t assume they’re harmless just because they’re flat or look like normal tissue.
Why do some doctors still say I need a colonoscopy every 5 years?
Many doctors were trained under older guidelines that said 5 years was standard. Even after the 2020 update, some are hesitant to change because they fear missing cancer or facing legal risk. Others simply haven’t kept up with the latest research. Studies show less than 20% of US doctors correctly follow the new 7-10 year rule for low-risk polyps. Ask for the specific reason behind their recommendation - and don’t be afraid to get a second opinion.
Can I skip a colonoscopy if I feel fine?
Yes - if your last colonoscopy showed low-risk polyps and you’re following the recommended interval. Most colorectal cancers grow slowly, and feeling fine is normal even when precancerous polyps are present. Symptoms usually appear only when cancer is advanced. That’s why screening is so important. Skipping your follow-up because you feel okay is one of the most common reasons people develop cancer after a previous colonoscopy.
Does poor bowel prep affect my follow-up timeline?
Absolutely. If your bowel prep was poor - meaning the colon wasn’t fully cleaned - your doctor may recommend a repeat colonoscopy sooner, often within 1 year. This isn’t because of the polyps you had. It’s because they couldn’t see everything. A bad prep means they might have missed a polyp. Don’t assume your interval stays the same if your prep was subpar. Always ask if your prep was adequate.

Elise Lakey
November 26, 2025 AT 12:10I was so relieved to read this. I had one small adenoma removed last year and my doctor said 5 years, but I dug into the guidelines myself and found the 7-10 year window. Felt like I finally got some peace of mind. Thanks for laying it out so clearly.
Roscoe Howard
November 28, 2025 AT 06:46It is absolutely unacceptable that medical institutions in this country continue to rely on outdated protocols. The United States has led the world in gastrointestinal oncology research for decades, yet many practitioners remain entrenched in the 2000s. This is not merely negligence-it is institutional failure. The 2020 USMSTF guidelines are evidence-based, peer-reviewed, and universally accepted by accredited societies. To ignore them is to endanger lives.
Shirou Spade
November 29, 2025 AT 14:42It’s funny how we treat medical guidelines like laws when they’re really just maps drawn by people who’ve seen thousands of cases. We forget that the colon doesn’t care about consensus-it just grows polyps. The real question isn’t when to come back, but why we’re so afraid of waiting. Is it the procedure? Or is it the fear that we’re not in control of our own bodies?
Patricia McElhinney
November 30, 2025 AT 18:48Ugh. I can’t believe people are still falling for this ‘7-10 year’ nonsense. I had a friend who waited 8 years because she ‘read it online’ and now she’s got stage 3. You think you’re being smart but you’re just playing Russian roulette with your colon. If you had polyps once, you’re not ‘low risk’-you’re high risk forever. 5 years. No exceptions. And if your doc says otherwise, find a new one. Period.
Dolapo Eniola
December 1, 2025 AT 12:13Bro this is why Africa is behind 😭. We don’t even have colonoscopies in most villages. You guys worry about 5 vs 7 years? We worry about if we’ll ever see a doctor who knows what a polyp is. 😅 But seriously-this info is gold. Save it. Print it. Send it to your cousin who thinks ‘feeling fine’ means you’re cured. 🙏
Agastya Shukla
December 2, 2025 AT 17:52From a clinical epidemiology standpoint, the shift from 5 to 7-10 years for low-risk adenomas is statistically robust. The NNT (number needed to treat) for early detection in this cohort is negligible beyond 7 years, and the cost-benefit ratio improves significantly. However, the real challenge lies in implementation fidelity-especially in decentralized care systems where EHR integration is inconsistent. The 2022 survey data on SSL misclassification is particularly alarming, suggesting cognitive bias persists despite evidence.
Rachel Villegas
December 3, 2025 AT 17:49This is the most helpful thing I’ve read all year. I just got my results and had three small adenomas. I was so stressed about coming back in 3 years, but now I see it’s not a punishment-it’s a plan. Thank you for explaining the why behind the numbers. I’ll be printing this out for my doctor.
Emily Craig
December 5, 2025 AT 01:10So let me get this straight-we’re supposed to wait up to 10 years to check for something that can kill you… but we’ll get a reminder for our Netflix subscription every 3 days? 😒 I’m just saying, if your colon’s got a personality, it’s probably screaming right now. But hey, at least we’ve got apps now to tell us when to go. #ColonoscopyChronicles