Adenoma Follow-Up: What You Need to Know About Monitoring and Management
When an adenoma, a noncancerous growth in the colon or rectum that can turn into cancer if left unchecked. Also known as adenomatous polyp, it is one of the most common findings during a colonoscopy. is found, the real work begins—not with surgery, but with adenoma follow-up. This isn’t just a routine reminder from your doctor. It’s your best defense against colorectal cancer. Most adenomas grow slowly, but without regular checks, some can become malignant over time. The goal isn’t to panic, but to stay ahead.
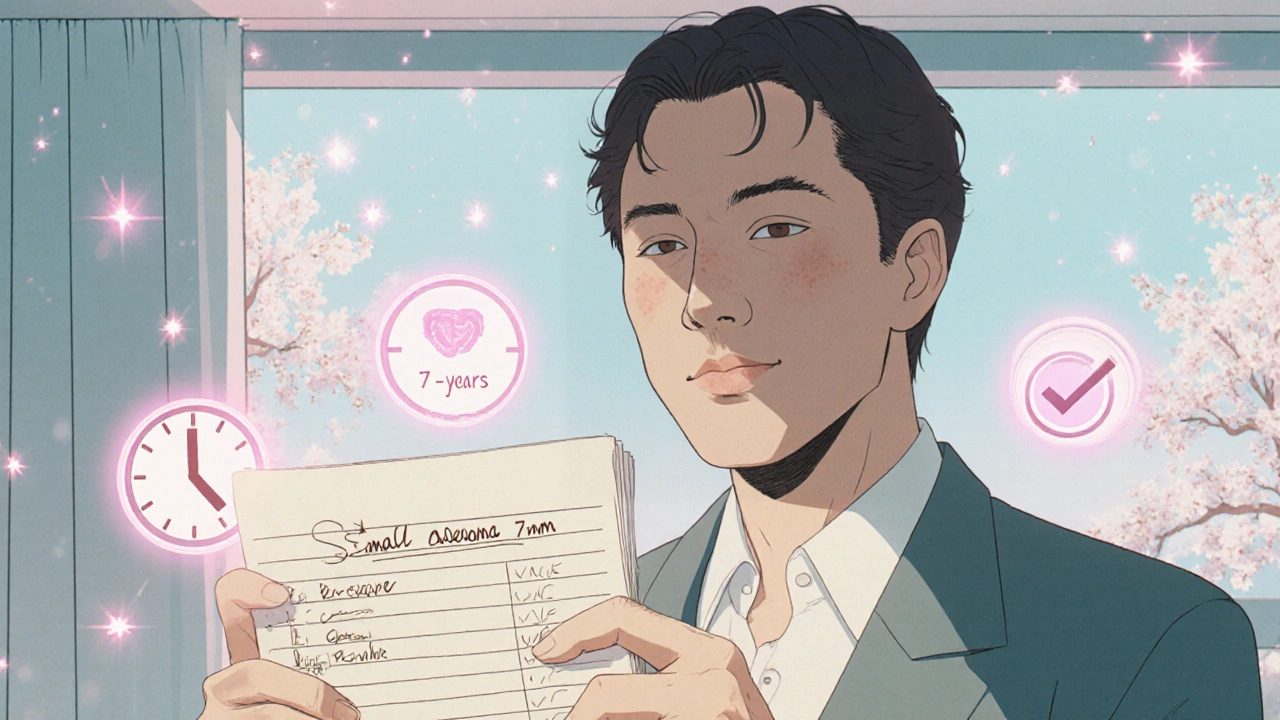
What happens after an adenoma is removed? It depends on the size, number, and type. A small, low-risk adenoma might only need a repeat colonoscopy in five to ten years. But if you had three or more, or if any were larger than one centimeter, or had advanced features like villous components, your follow-up could be as soon as three years. This is where colonoscopy after adenoma, a targeted surveillance procedure used to detect new or recurring growths after removal becomes essential. It’s not a one-size-fits-all plan. Your doctor uses guidelines from the U.S. Multi-Society Task Force on Colorectal Cancer, which base timing on your specific pathology report—not just the fact that you had a polyp.
People often worry about the procedure itself, but the bigger issue is skipping it. Studies show that skipping follow-up colonoscopies increases cancer risk by up to five times. And it’s not just about the colon. If you’ve had an adenoma, you’re more likely to develop another one—sometimes in different spots. That’s why polyp surveillance, the systematic, scheduled monitoring of polyp recurrence after removal matters more than ever. It’s not about fear. It’s about control. You’re not waiting for symptoms. You’re catching problems before they become emergencies.
Some patients think if they feel fine, they don’t need another scope. But adenomas rarely cause pain or bleeding until they’re advanced. That’s why follow-up isn’t optional—it’s preventive medicine at its most effective. Lifestyle changes help, like eating more fiber, cutting back on red meat, and staying active, but they don’t replace monitoring. Your body can’t tell you when a tiny adenoma is growing. Only a scope can.
What about other tests? Stool-based tests like FIT or Cologuard are good for initial screening, but they’re not enough after an adenoma. If you’ve already had one, colonoscopy remains the gold standard. It lets your doctor see and remove anything suspicious right away. No waiting. No guesswork.
You’ll also hear about cancer risk after adenoma, the likelihood of developing colorectal cancer following the detection and removal of an adenomatous polyp. The good news? If you stick to your follow-up schedule, your risk drops dramatically—often to near-normal levels. The bad news? If you don’t, your chances go up fast. One study from the New England Journal of Medicine found that people who missed their follow-up colonoscopy were 11 times more likely to die from colon cancer within 15 years than those who didn’t.
So what’s next? Look at your last colonoscopy report. Note the size, number, and type of adenomas found. Write down your next appointment date. Set a reminder. Talk to your doctor about your personal risk. This isn’t about being told what to do. It’s about knowing what’s at stake—and taking charge.
Below, you’ll find real-world guides on how to manage medication side effects, understand drug interactions, and protect your health long-term—all tied to the same goal: staying informed so you can make smart choices. Because when it comes to adenoma follow-up, knowledge isn’t just power. It’s protection.