Cannabis and Prescription Drugs: Risks, Interactions, and What You Need to Know
When you use cannabis and prescription drugs, the combination can alter how your body processes medications, sometimes with life-threatening results. Also known as marijuana and meds, this mix isn’t just about feeling higher—it’s about how your liver, brain, and heart respond when two powerful substances collide. Many people think if it’s natural, it’s safe. But cannabis, whether smoked, vaped, or taken as oil, doesn’t play nice with common prescriptions. It can make your blood thinner too strong, turn your antidepressant useless, or turn your painkiller into a breathing hazard.
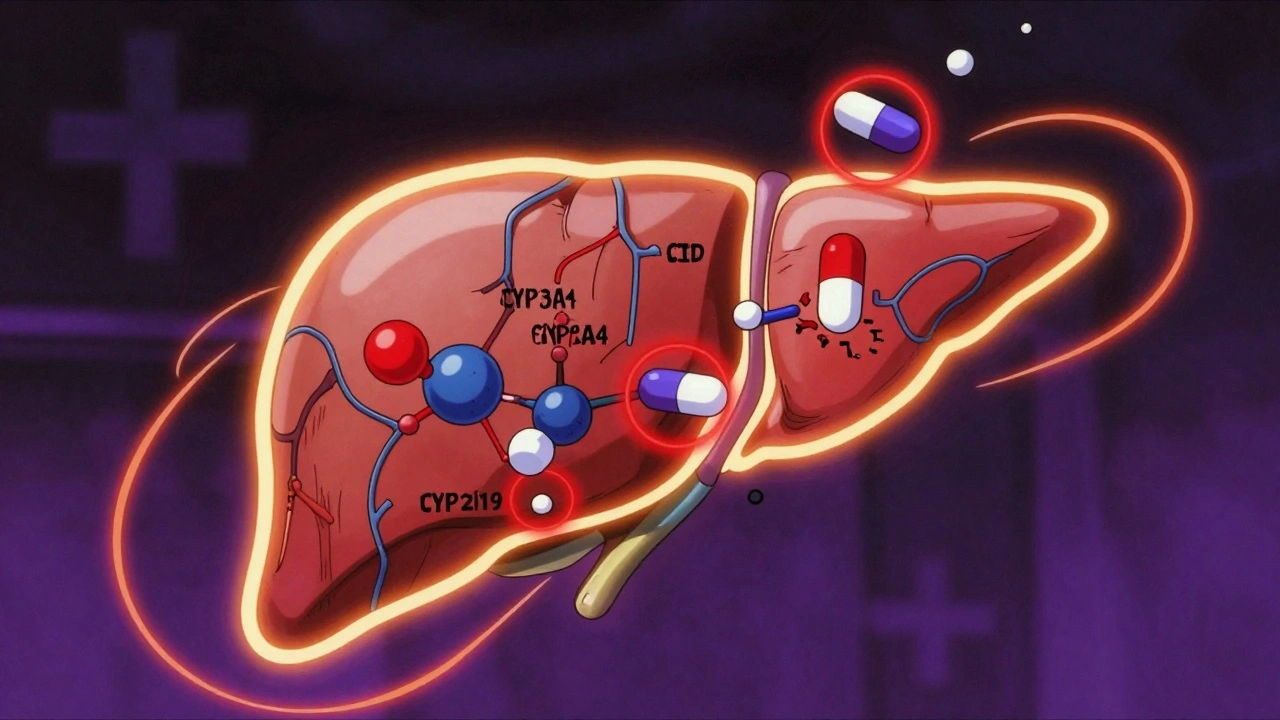
The real danger isn’t always obvious. Take CBD, a compound in cannabis often sold as a supplement for anxiety or pain. Also known as cannabidiol, it’s the same molecule that blocks the liver enzymes responsible for breaking down over 60% of all prescription drugs. That means if you’re on statins, blood pressure pills, or seizure meds, CBD can cause those drugs to build up in your system—like pouring more gas into a car that’s already full. The FDA has warned about this with epilepsy drugs like clobazam, where CBD raised levels by up to 600%. Even over-the-counter pain relievers like ibuprofen can become riskier when mixed with cannabis, especially if you have kidney issues.
It’s not just CBD. THC, the psychoactive part of cannabis, affects your brain’s receptors in ways that clash with antidepressants, antipsychotics, and sedatives. People on SSRIs like sertraline or fluoxetine report feeling more dizzy, nauseous, or overly sleepy when they use cannabis. Those on opioids for chronic pain? Mixing them with cannabis can slow your breathing to dangerous levels—especially if you’re older or have sleep apnea. And if you’re on blood thinners like warfarin, cannabis can make your INR numbers swing unpredictably, raising your risk of internal bleeding.
What’s missing from most conversations is the lack of monitoring. Doctors rarely ask about cannabis use, and patients rarely volunteer it—thinking it’s harmless or illegal to mention. But the data is clear: in emergency rooms, nearly 1 in 5 cannabis-related visits involve a drug interaction. The problem grows when people switch brands, doses, or forms—like going from a low-THC edible to a high-potency vape. One dose might be fine. The next could be a hospital trip.
You don’t have to quit cannabis to stay safe. But you do need to talk to your pharmacist or doctor before combining it with anything. Keep a log: what you took, when, and how you felt. Bring your bottles to appointments—even the supplements. If your doctor doesn’t know about cannabis, they can’t protect you. The posts below show real cases: how antihistamines worsen movement disorders, how statins and antifungals clash, how alcohol and opioids can kill. These aren’t abstract warnings. They’re lessons from people who didn’t realize their meds and cannabis were working against each other. What you learn here could keep you out of the ER.