FDA Pregnancy Guidelines: What You Need to Know About Medication Safety During Pregnancy
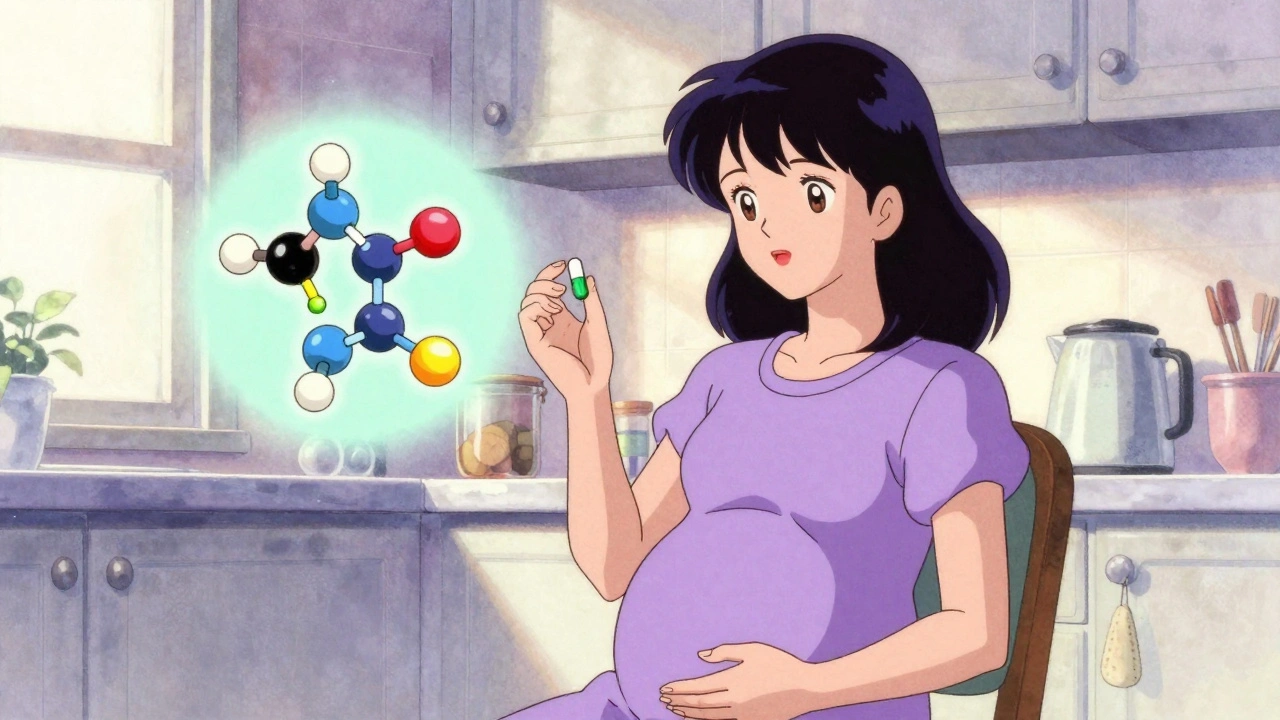
When you’re pregnant, every pill, supplement, or OTC remedy carries a question: FDA pregnancy guidelines are meant to answer that — but they’re not always clear. The FDA classifies drugs into categories based on known risks to the fetus, but those labels don’t tell the whole story. Many women take medications for conditions like thyroid disease, depression, or high blood pressure, and stopping them can be just as dangerous as continuing them. The real goal isn’t to avoid all drugs — it’s to use the right ones at the right time. The FDA pregnancy guidelines, a system used by the U.S. Food and Drug Administration to classify the potential risks of medications during pregnancy. Also known as pregnancy risk categories, it helps doctors and patients weigh benefits against possible harm to the developing baby.
These guidelines don’t exist in a vacuum. They’re built on data from animal studies, limited human trials, and post-marketing reports — the same systems that catch rare side effects like Neuroleptic Malignant Syndrome, a life-threatening reaction to certain psychiatric medications or Acute Generalized Exanthematous Pustulosis, a sudden, severe drug-induced skin rash. That means the guidelines evolve. A drug once thought safe might later be linked to birth defects after thousands of women use it. That’s why post-marketing pharmacovigilance matters — it’s how we learn what clinical trials missed. For example, some medications like levothyroxine, the standard treatment for hypothyroidism during pregnancy are considered safe because they replace a hormone your body needs, not because they’re harmless. Others, like certain antidepressants or acne drugs, carry known risks that require careful monitoring.
It’s not just about the drug itself — it’s about timing, dosage, and alternatives. A medication that’s risky in the first trimester might be fine later. A drug that’s risky for one woman might be necessary for another. That’s why your doctor doesn’t just look at the FDA label — they look at your health history, your condition, and what happens if you don’t treat it. For women with gestational diabetes, managing blood sugar with diet and safe meds like insulin follows its own set of rules. For those with chronic conditions, switching to a safer alternative before conception can make all the difference. And sometimes, the safest choice isn’t a drug at all — it’s acupuncture for pain, saline rinses for congestion, or lifestyle changes that reduce the need for medication.
What you’ll find in the posts below isn’t just a list of safe and unsafe drugs. It’s a practical guide to understanding how medications affect pregnancy, what the real risks are, and how to advocate for yourself when your care feels uncertain. From how generic drugs are tested for safety to how cultural beliefs shape what women are willing to take, these articles connect the dots between science, experience, and real-life decisions. You’ll learn how to spot dangerous interactions, what to ask your pharmacist, and why stopping a medication without guidance can be riskier than staying on it. This isn’t about fear — it’s about control. You deserve to know what’s in your body, why it’s there, and what it might do to your baby — without jargon, without guesswork, and without being talked down to.