Generic vs Brand Name Drugs: What Really Matters for Your Health
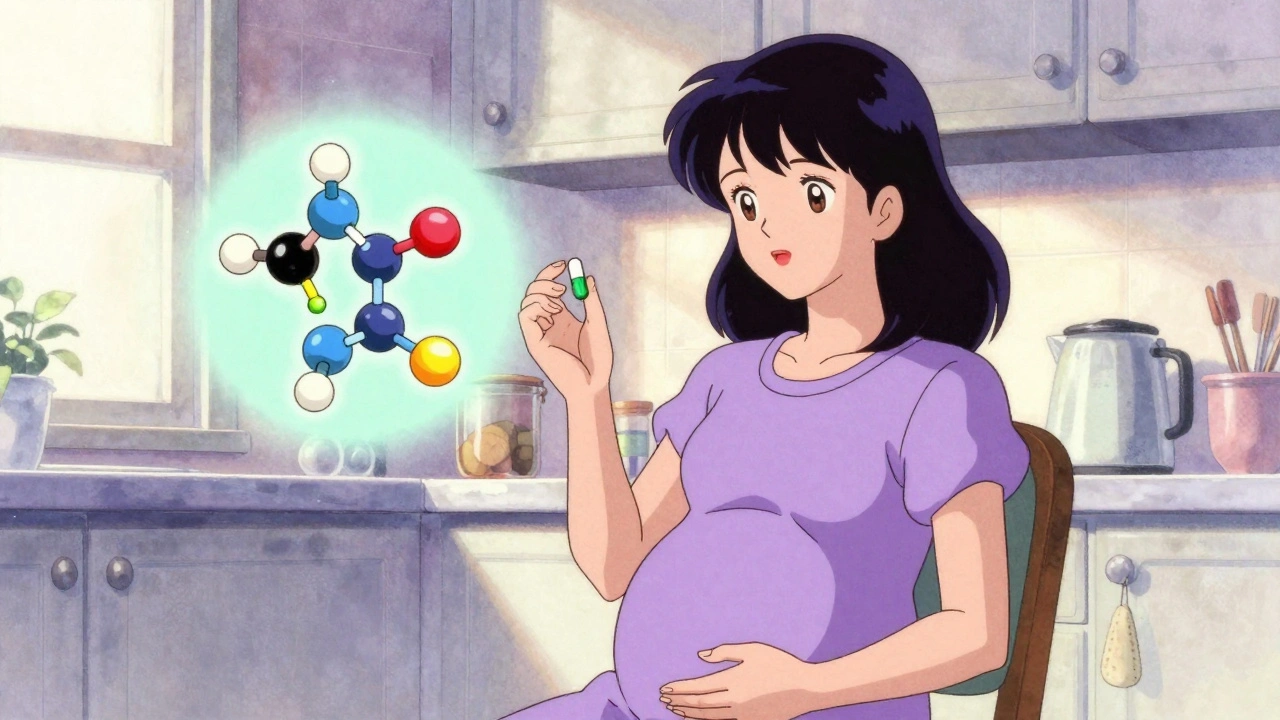
When you pick up a prescription, you might see two options: the familiar brand name or a cheaper generic version. Generic drugs, are FDA-approved copies of brand-name medications that contain the same active ingredient, strength, and dosage form. Also known as generic equivalents, they’re designed to work the same way—just at a fraction of the cost. But here’s the question most people don’t ask: does that mean they’re always exactly the same? The short answer is usually yes—but not always. For most meds, like antibiotics or blood pressure pills, generics perform just as well. But for drugs where tiny differences matter—like thyroid medication, seizure control, or blood thinners—small changes in how the drug is absorbed can affect how you feel.
Brand name drugs, are the original versions developed by pharmaceutical companies after years of research and clinical trials. Also known as innovator drugs, they carry the patent protection that lets companies recoup their investment. Once that patent expires, other manufacturers can produce the same drug under its chemical name. The FDA requires generics to match the brand in active ingredients and how quickly they release into your body—but they can differ in fillers, dyes, or coating. These differences are usually harmless. But for some people, especially those on narrow therapeutic index drugs, even small variations can trigger side effects or reduce effectiveness. That’s why switching from brand to generic isn’t always as simple as saving money. It’s about your body’s response. And if you’ve ever noticed a change in how you feel after switching, you’re not imagining it. Studies show that for drugs like levothyroxine or warfarin, sticking with the same manufacturer—even if it’s generic—can help avoid fluctuations in your levels.
Drug equivalence, is the standard the FDA uses to approve generics, based on dissolution testing and bioequivalence studies. This means the generic must release its active ingredient at the same rate and to the same extent as the brand. But equivalence doesn’t mean identical. The pills might look different, taste different, or even have slightly different inactive ingredients. That’s why some patients report better results with one brand over another—even when both are labeled generic. It’s not placebo. It’s pharmacology. What you’re really looking for is consistency. If your doctor or pharmacist recommends switching, ask if it’s from the same manufacturer. If you’re on a mail-order service, check if your generic changes every month. And if you’re managing a chronic condition like epilepsy, heart disease, or hypothyroidism, don’t assume all generics are created equal.
What you’ll find below is a collection of real stories, data, and warnings from people who’ve been through this. From why your thyroid med acts up after a switch, to how tiered copays make generics cost more than expected, to why some people react to fillers in pills they’ve taken for years. These aren’t theoretical concerns—they’re daily realities for millions. Whether you’re saving money, switching insurers, or just wondering if you’re getting the same medicine, this guide cuts through the noise. You deserve to know what’s in your pill—and why it might be working differently than before.