Gestational Diabetes Meal Plan: What Works and What to Avoid
When you're pregnant and diagnosed with gestational diabetes, a type of diabetes that develops during pregnancy due to hormonal changes that cause insulin resistance. It's not your fault, and it's not permanent—but it needs attention. About 6-9% of pregnant people in the U.S. get it, and the right gestational diabetes meal plan, a structured eating approach designed to keep blood sugar levels steady. It's not about starving yourself or cutting out carbs entirely. It’s about choosing the right kinds, at the right times, and pairing them with protein and fiber to slow absorption.
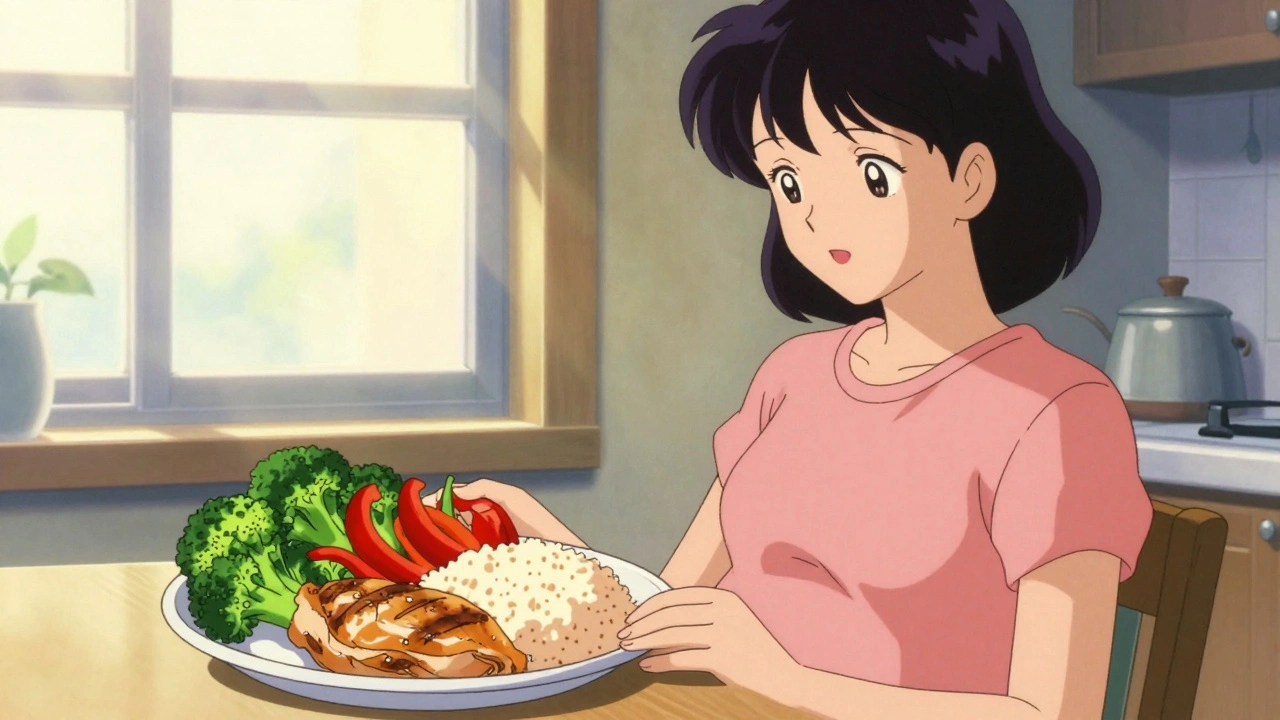
What makes this different from regular diet advice? Your body is doing something unique: it’s trying to feed a growing baby while fighting off the effects of pregnancy hormones that block insulin. That’s why eating three large meals won’t work. Smaller, balanced meals every 2-3 hours help keep blood sugar from spiking and crashing. A blood sugar control, the goal of managing glucose levels through food timing and composition. It’s not just about avoiding sugar—it’s about managing how fast your body turns food into glucose. Foods like white bread, sugary cereals, and fruit juices can cause sharp rises. Instead, swap them for whole grains, legumes, non-starchy vegetables, and lean proteins. Pairing an apple with peanut butter or yogurt with chia seeds gives you steady energy without the crash.
Many people worry they have to give up their favorite foods, but that’s not true. You can still enjoy pasta, rice, or even dessert—but portion size and timing matter. A quarter plate of whole grain pasta with a half cup of beans and grilled chicken works better than a full bowl of white rice with no protein. Snacks like hard-boiled eggs, cottage cheese, or a handful of almonds help bridge meals without spikes. And don’t skip breakfast. Morning insulin resistance is often worse, so starting the day with protein and fiber (like eggs with spinach and whole grain toast) sets the tone.
What’s missing from most advice? The role of movement. Even a 15-minute walk after meals helps lower blood sugar. It’s not a cure, but it’s a simple tool that works with your meal plan. Also, tracking your meals and glucose levels—even just a few days a week—helps you see what works for your body. Not everyone responds the same way to oats or bananas. Your plan should be flexible, not rigid.
You’re not alone in this. Thousands of pregnant people manage gestational diabetes successfully every year. The goal isn’t perfection—it’s progress. Small, consistent choices add up. And when you get the meal plan right, you reduce the risk of complications like large babies, early delivery, or future type 2 diabetes for both you and your child.
Below, you’ll find real advice from people who’ve been there—what worked, what didn’t, and how they made it manageable without feeling deprived. No myths. No extreme diets. Just practical, science-backed ways to eat well while you’re expecting.