MS Relapse: What Happens, How to Spot It, and What You Can Do
When you have MS relapse, a sudden return or worsening of multiple sclerosis symptoms due to inflammation in the central nervous system. Also known as an exacerbation, it’s not just feeling tired or stressed—it’s a biological event that can change how your body moves, feels, or thinks. This isn’t a one-time thing for many people with multiple sclerosis, a chronic autoimmune condition where the immune system attacks the protective covering of nerve fibers. Relapses can happen months or years apart, and each one leaves a mark—sometimes temporary, sometimes lasting.
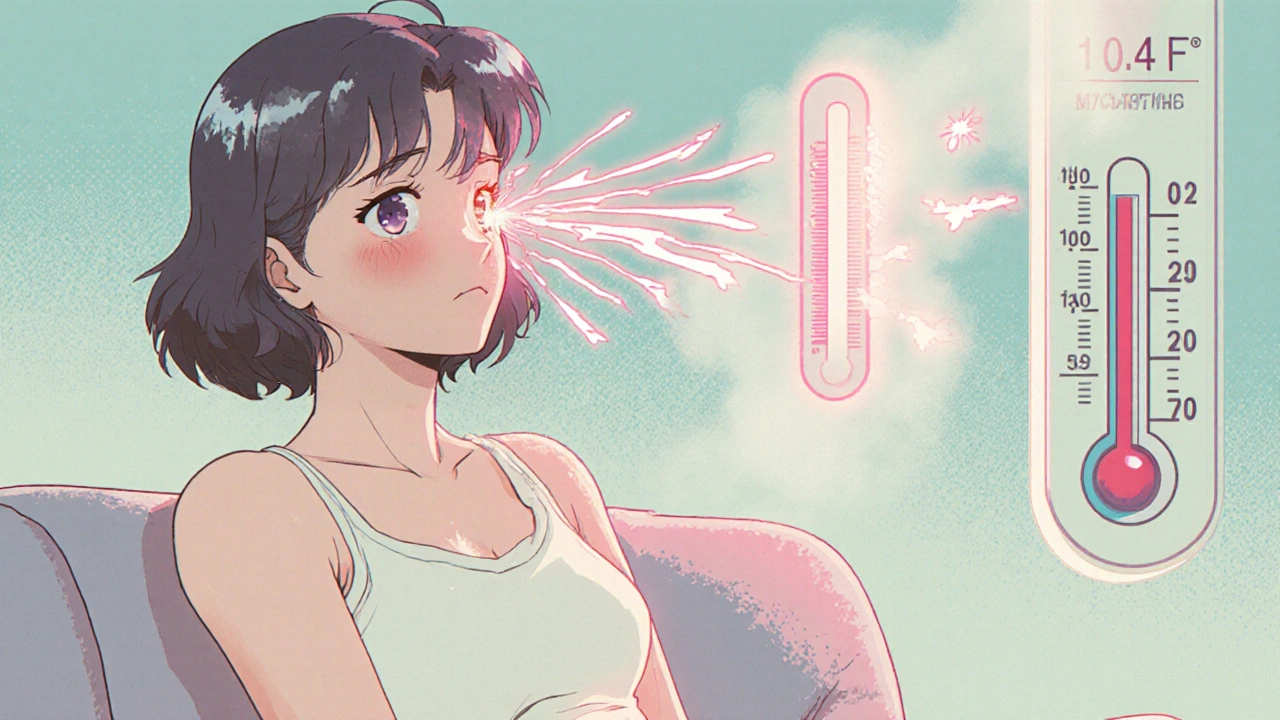
Not every bump in symptoms is a relapse. If you feel more fatigued after a long day or your legs feel heavy after walking too far, that’s often just heat sensitivity or overexertion. A true MS relapse, requires new neurological symptoms or a significant worsening of old ones that lasts at least 24 hours and occurs at least 30 days after the last episode. Common signs include sudden vision loss in one eye, numbness spreading down one side of your body, trouble walking without support, or bladder control issues that weren’t there before. These aren’t random—they’re signals your nervous system is under attack.
What causes these flare-ups? Stress, infections like the flu or a UTI, and even extreme heat can trigger them. Some people notice a pattern—maybe their relapses happen after skipping doses of their disease-modifying drug, or during allergy season. The key is tracking: keep a simple journal of symptoms, what you were doing, and how you felt. That info helps your neurologist decide if it’s a relapse or something else, and whether you need steroids, plasma exchange, or just rest.
There’s no magic cure for an MS relapse, but treatment can shorten it. High-dose corticosteroids like methylprednisolone are the go-to—they reduce inflammation fast. But they’re not for everyone. If you’ve got diabetes, high blood pressure, or a history of mood disorders, your doctor will adjust the plan. Some people recover fully within weeks. Others are left with lasting changes. That’s why managing disease progression, the long-term accumulation of disability in multiple sclerosis matters more than treating single episodes. The real goal isn’t just surviving relapses—it’s preventing them.
That’s where the posts below come in. You’ll find real-world advice on how medications like interferons and oral therapies actually work over time, what side effects to watch for, and how to avoid mistakes that make relapses more likely. We cover everything from managing fatigue and muscle spasms to how storage conditions for your pills can affect your health. No fluff. Just what works—for your body, your routine, and your life.