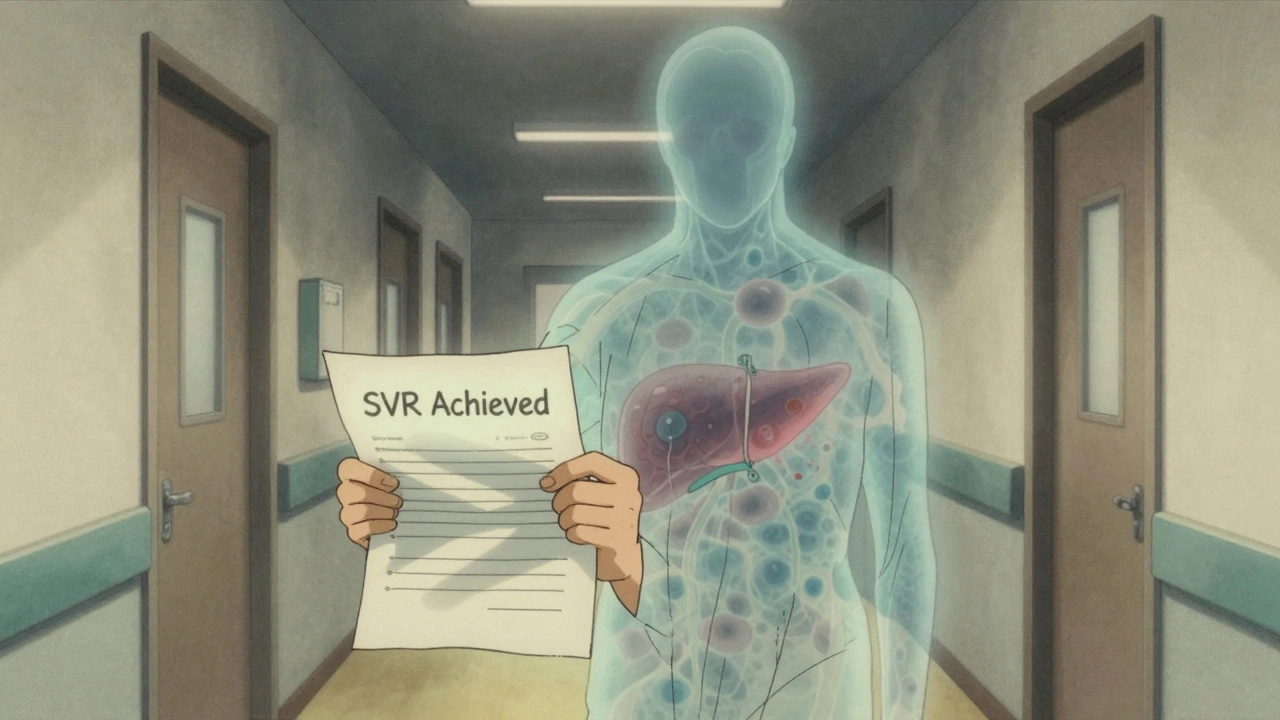
Post-SVR Liver Cancer: Risks, Monitoring, and What Comes After Hepatitis C Treatment
When someone with hepatitis C achieves SVR, Sustained Virologic Response, meaning the virus is undetectable in the blood 12 weeks after finishing treatment. Also known as cured hepatitis C, it’s a major win — but not the end of the story. Many assume that once the virus is gone, the liver heals completely and cancer risk disappears. That’s not true. Even after SVR, people with advanced scarring — cirrhosis — still face a real risk of developing liver cancer, a type of cancer called hepatocellular carcinoma that starts in liver cells. This is called post-SVR liver cancer, liver cancer that develops after successful hepatitis C treatment. It’s not common, but it happens often enough that skipping follow-up can be dangerous.
Why does this happen? The damage from years of hepatitis C doesn’t vanish overnight. Scar tissue from cirrhosis stays in place, and those damaged liver cells can still turn cancerous over time. Studies show that about 1 to 3% of people with cirrhosis develop liver cancer each year, even after SVR. That risk drops compared to before treatment, but it doesn’t disappear. People who had cancer before treatment, those with ongoing alcohol use, or those with diabetes or obesity are at even higher risk. The liver doesn’t reset — it needs watching.
This is where monitoring comes in. Regular ultrasounds every six months, sometimes with blood tests like AFP, are the standard. These aren’t optional checkups — they’re lifesavers. Early detection means treatment options like surgery, ablation, or targeted drugs work far better. Waiting until symptoms appear — like belly pain, weight loss, or yellow skin — often means it’s too late. Many patients assume they’re safe after treatment and skip follow-ups. That’s the biggest mistake.
And it’s not just about cancer. Even after SVR, liver function can stay impaired. Fatty liver, alcohol, or metabolic syndrome can keep pushing damage forward. That’s why lifestyle changes — cutting alcohol, losing weight, controlling blood sugar — aren’t just good advice. They’re part of your long-term protection plan. Your doctor isn’t being overly cautious. They’re helping you avoid a second battle you thought you already won.
The posts below cover the real-world details you need: how doctors track liver health after cure, what blood tests actually tell you, why some people still get cancer despite treatment, and how to reduce your risk without relying on guesswork. You’ll find practical advice on monitoring schedules, what to ask your provider, and how to interpret your own lab results. This isn’t theory. It’s what’s happening in clinics right now — and what you need to know to stay safe.