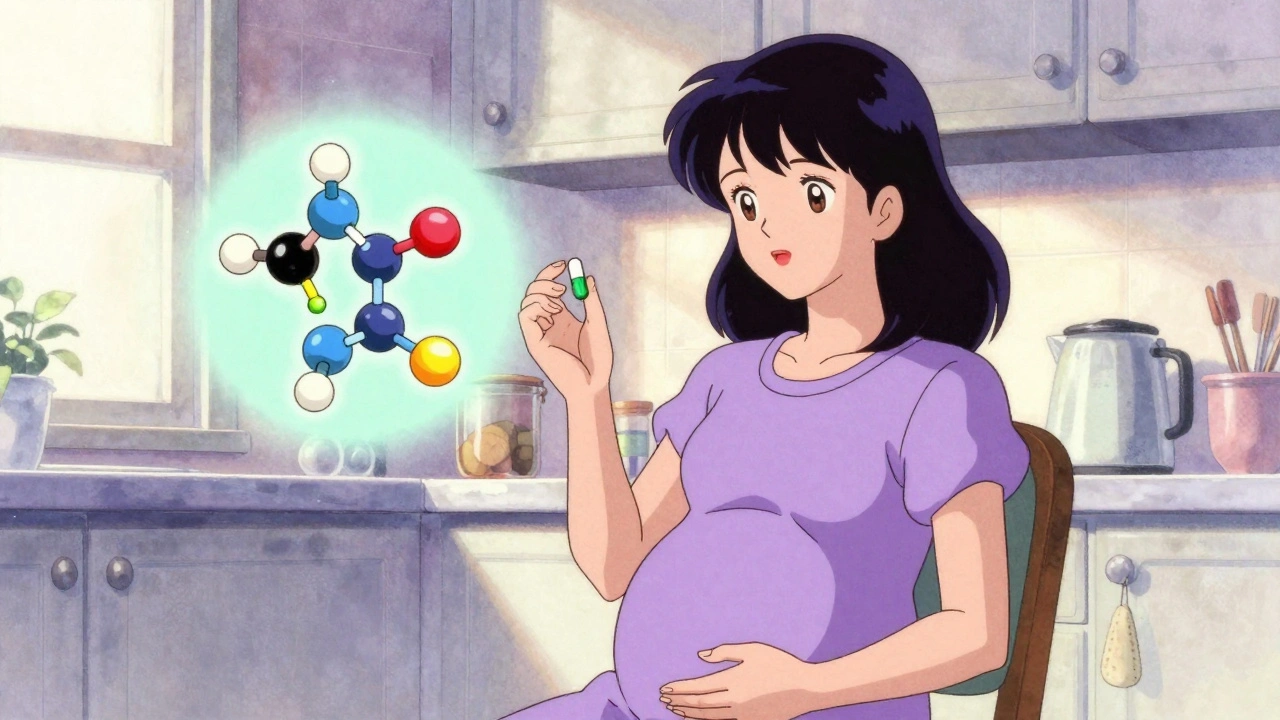
Prenatal Meds: What You Need to Know About Medications During Pregnancy
When you're pregnant, every pill you take matters. prenatal meds, medications prescribed or taken during pregnancy to manage health conditions or support fetal development. Also known as pregnancy-safe drugs, these aren't just about vitamins—they include everything from insulin for gestational diabetes to thyroid hormones, antidepressants, and even antibiotics. The big question isn't whether you need them—it's whether they're safe for you and your baby. Many women assume all meds are risky, but skipping a needed treatment can be far more dangerous. For example, untreated hypothyroidism during pregnancy can affect your baby's brain development, and uncontrolled gestational diabetes raises the risk of preterm birth and large birth weight.
Not all drugs are created equal. levothyroxine, a synthetic thyroid hormone used to treat underactive thyroid in pregnancy, is considered safe and often required to keep both mom and baby healthy. On the other hand, some common meds like certain NSAIDs or ACE inhibitors can cause serious problems if taken during pregnancy. Then there are meds that seem harmless—like sedating antihistamines—but can worsen conditions like restless legs syndrome, which already affects many pregnant women. Even something as simple as an OTC nasal spray can lead to rebound congestion, and that’s just one more thing to manage when your body is already changing.
Managing prenatal meds isn’t just about picking the right pill—it’s about understanding how your body processes drugs differently when pregnant. Blood volume increases, kidney function speeds up, and liver metabolism shifts. That means a dose that worked before might not work now—or could build up to unsafe levels. That’s why monitoring matters. Women on thyroid meds need regular TSH checks. Those with gestational diabetes need to track blood sugar and adjust diet or insulin. And if you're on any chronic medication, you need to talk to your doctor before getting pregnant, not after.
You’re not alone in this. Millions of pregnant women take some form of medication, and the science behind what’s safe keeps getting better. But misinformation still spreads fast. That’s why it’s crucial to rely on data, not rumors. The posts below cover real cases: how drug reactions like AGEP or NMS can show up unexpectedly, why mail-order generics might not be the best choice when you’re pregnant, how team-based care helps reduce errors in prescribing, and what to do if you notice side effects you didn’t expect. You’ll find practical advice on managing gestational diabetes with meal plans, how to avoid dangerous interactions with common drugs, and why some meds that work fine outside pregnancy need a complete rethink inside it.
There’s no one-size-fits-all answer with prenatal meds. What’s safe for one person might not be for another. But with the right info, you can make confident choices—without fear or guesswork. The posts ahead give you the facts you need, straight from real-world cases and medical evidence. No fluff. No fearmongering. Just what works, what doesn’t, and what you should ask your doctor next time you’re handed a prescription.