Prescription Drug Costs: What You Really Pay and Why It Matters
When you pick up a prescription, the price on the receipt often feels random—sometimes it’s $5, sometimes it’s $500. That’s because prescription drug costs, the amount patients pay out-of-pocket for medications prescribed by doctors. Also known as pharmaceutical costs, they’re shaped by patents, insurance rules, and global manufacturing—not just how much the drug costs to make. Unlike groceries or gas, drug prices don’t follow supply and demand. A generic version of a heart drug might cost $4 at Walmart but $120 at your local pharmacy if your insurance doesn’t cover it. That’s not a mistake. It’s the system.
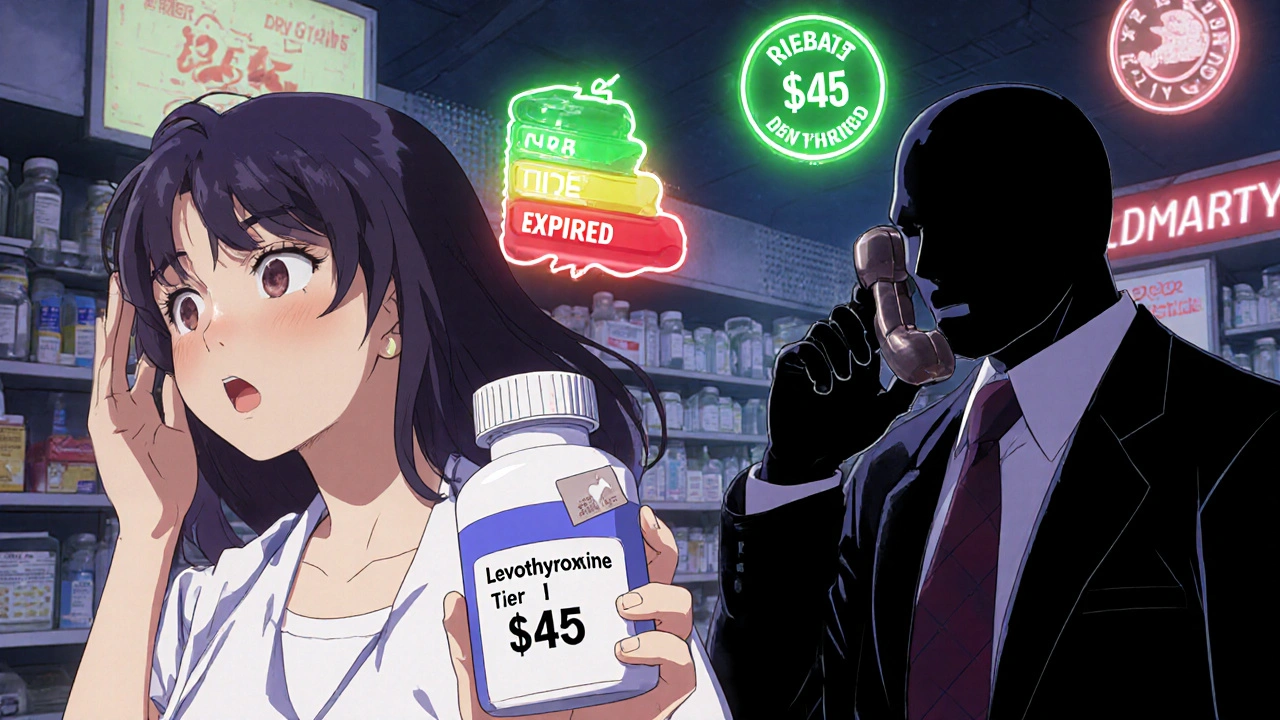
Behind every price tag are hidden players: generic drugs, medications that contain the same active ingredients as brand-name pills but are sold after the patent expires. Also known as off-patent drugs, they’re supposed to lower costs—but even these can spike in price if only one factory makes them. Take the diabetes drug metformin: it’s been around for decades, made in India or China, and costs pennies to produce. Yet, in some states, a 30-day supply jumped from $4 to $30 overnight because the manufacturer cut supply. Meanwhile, medication affordability, how easily patients can pay for their prescriptions without skipping meals or skipping doses. Also known as drug access, it’s not just about income—it’s about insurance networks, pharmacy benefit managers, and whether your doctor knows which pills are actually affordable. Many people don’t know their insurance has a formulary—a list of approved drugs. If your pill isn’t on it, you pay more. Or worse, you get denied.
Some drugs, like roflumilast for COPD or even a simple antibiotic, cost hundreds because the maker holds a patent or controls distribution. Others, like generic statins or blood pressure pills, are dirt cheap—but only if you know where to look. The prescription drug costs you see at the counter aren’t the real cost. They’re what’s left after insurers, PBMs, and pharmacies take their cut. And if you’re on multiple meds, those small differences add up fast. One person might pay $200 a month for their diabetes and heart meds. Another, with the same conditions, pays $20—because they switched to a different pharmacy, used a coupon, or asked their doctor for an alternative.
It’s not just about money. Skipping doses because of cost leads to hospital visits, worse outcomes, and higher long-term bills. That’s why so many posts here focus on real solutions: how to compare Fosamax with cheaper bone drugs, how to get help with roflumilast, or how to spot when a generic isn’t working right. You’ll find guides on how to talk to your pharmacist about lower-cost options, how to use patient assistance programs, and why some drugs cost more just because they’re marketed better—not because they’re better.
What you’ll find below isn’t theory. It’s real stories, real data, and real strategies from people who’ve been there. Whether you’re paying for SGLT2 inhibitors, statins, or antibiotics, you’re not alone—and you don’t have to accept whatever price you’re given. The system is broken, but there are ways to fight back. Let’s look at how.