Pseudorelapse: What It Is, Why It Happens, and How to Tell It Apart from Real Flare-Ups
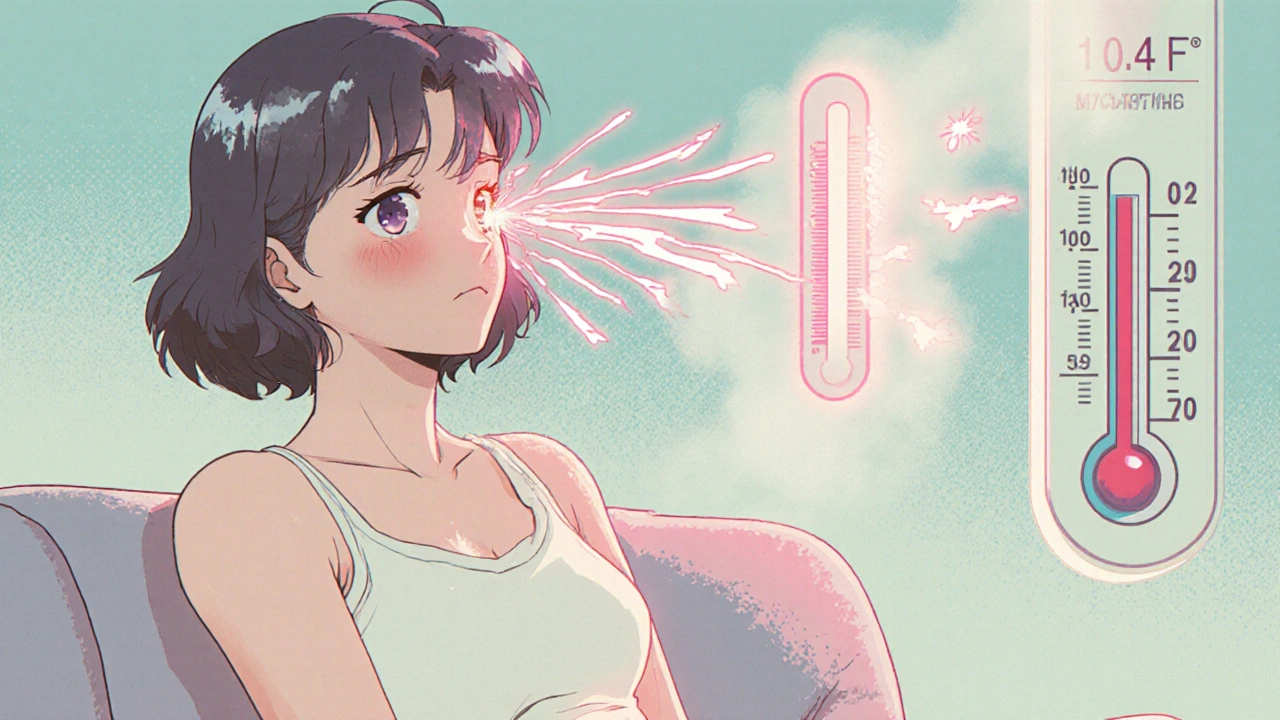
When your symptoms come back after months of feeling fine, it’s natural to panic—is this a pseudorelapse, a return of symptoms that looks like a disease flare-up but is actually caused by medication changes, stress, or withdrawal. Also known as drug-induced symptom rebound, it’s often mistaken for the real thing. But here’s the catch: pseudorelapse isn’t your disease coming back. It’s your body reacting to something else—like a missed dose, a new medication, or even just running on too little sleep.
Think of it like this: if you’ve been on an antidepressant for a year and suddenly feel low again after switching brands, that’s not your depression returning—it might be your brain adjusting to a slightly different chemical balance. Same with Parkinson’s patients who start shaking again after changing their levodopa dose. Or someone on long-term steroids who gets a rash and thinks it’s their original condition flaring, when it’s really just steroid withdrawal. These aren’t relapses. They’re medication side effects, unintended reactions caused by changes in drug formulation, timing, or dosage. And they’re way more common than most doctors admit.
Then there’s drug tolerance, when your body gets used to a medication and needs more to get the same effect. That’s not disease progression—it’s physiology. Your nervous system adapts. Your liver processes the drug faster. Your receptors downregulate. Suddenly, you feel worse. You panic. You think you’re getting sicker. But you’re not. You’re just in a phase where your body needs a tweak, not a total treatment overhaul.
And don’t forget withdrawal symptoms, the body’s response when you cut back or stop a medication too quickly. These can mimic the original illness perfectly—fatigue, brain fog, muscle aches, mood swings. People think they’re relapsing. Doctors think they’re relapsing. But it’s just your body screaming for the drug it’s been used to.
What makes pseudorelapse so tricky is that it doesn’t show up on scans or blood tests. There’s no biomarker. No lab value to prove it’s not real. That’s why so many people get stuck on the wrong treatment path—more drugs, higher doses, unnecessary tests—all because no one looked at the timing, the dose changes, or the lifestyle shifts.
Here’s what you can do: track your symptoms with dates. Note every change in meds—even a generic switch. Write down your sleep, stress, and diet. If your symptoms started right after you changed pills, skipped a dose, or cut back on caffeine, it’s probably not your disease. It’s your body reacting. And that’s fixable. Often, just adjusting the timing, adding a short-term support med, or giving your system time to reset makes all the difference.
The posts below dive into real cases—people who thought they were relapsing, only to find out it was something else entirely. You’ll see how a change in generic brand triggered tinnitus, how stopping a nasal spray caused rebound congestion that felt like a sinus infection, and why switching from brand to generic thyroid meds made someone feel like they were getting sicker. These aren’t rare stories. They’re everyday mistakes that cost people time, money, and peace of mind. What you’ll find here isn’t theory. It’s what actually happens when people confuse pseudorelapse with relapse—and how to fix it before it gets worse.