Serrated Polyp Guidelines: What You Need to Know About Detection and Risk
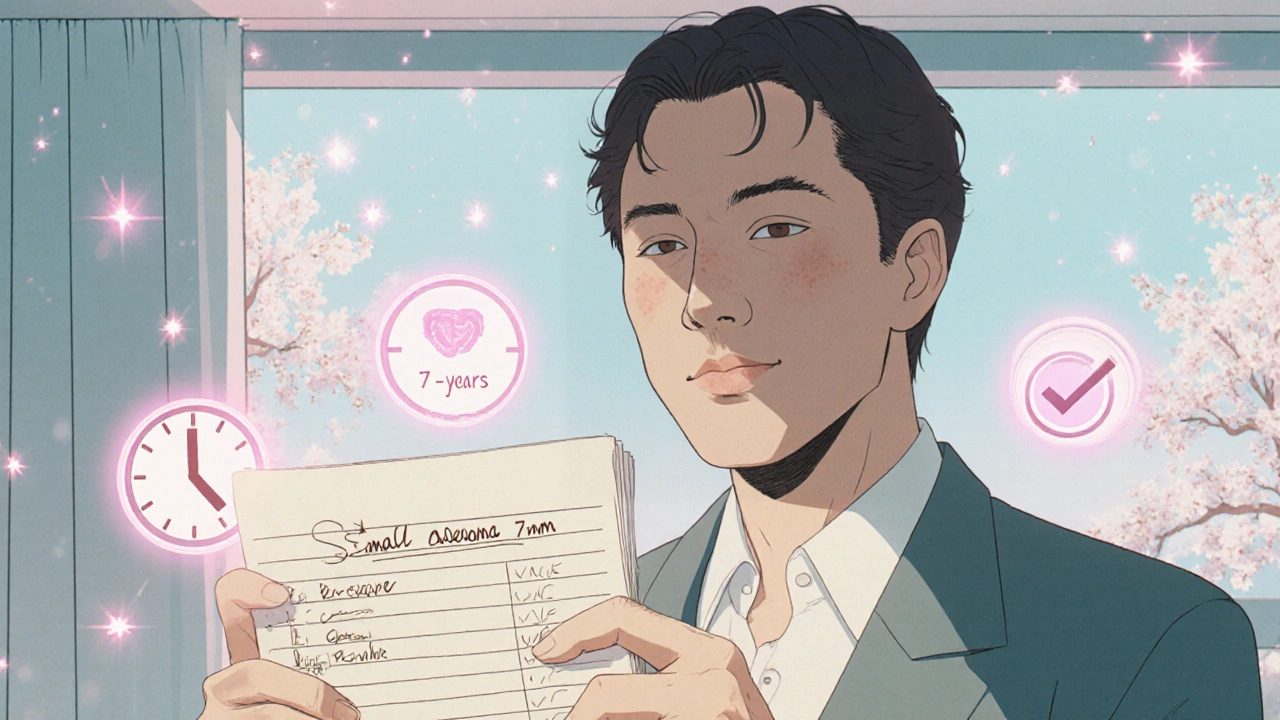
When it comes to colon cancer prevention, serrated polyp guidelines, a set of medical recommendations for identifying and managing serrated polyps during colonoscopies. These guidelines matter because serrated polyps are sneaky—they don’t look like the typical adenomas, yet they can turn into cancer faster and without warning. Unlike regular polyps that grow slowly over years, some serrated polyps, especially those in the right side of the colon, can become malignant in just 5 to 7 years. That’s why the colonoscopy guidelines, standard protocols used by gastroenterologists to screen for colorectal abnormalities have changed. The American College of Gastroenterology and the U.S. Multi-Society Task Force now treat serrated polyps differently based on size, location, and number.
Not all serrated polyps are the same. There are three main types: hyperplastic polyps (usually harmless), sessile serrated lesions (SSLs), and traditional serrated adenomas (TSAs). SSLs are the biggest concern—they’re flat, hard to spot, and often hide in the upper colon. That’s why colorectal cancer screening, the process of testing for early signs of colon cancer before symptoms appear now demands high-quality colonoscopies with careful inspection, not just a quick sweep. If a doctor misses one, the risk of future cancer goes up. That’s why guidelines now recommend longer withdrawal times during colonoscopy and better bowel prep. If you’ve had one serrated polyp, especially if it’s larger than 10 mm, you’ll likely need a follow-up colonoscopy sooner than the standard 10 years—sometimes as soon as 3 to 5 years.
What you won’t find in most public health ads is that serrated polyps are more common in older adults, smokers, and people with obesity. They’re also linked to certain genetic patterns, though most cases aren’t inherited. The good news? If caught early, they’re almost always removable during colonoscopy. The bad news? Many people don’t get screened on time, or their doctor doesn’t recognize the signs. That’s why understanding these guidelines isn’t just for doctors—it’s for anyone over 45 who wants to stay ahead of colon cancer. Below, you’ll find real-world insights from patients and clinicians on how these guidelines play out in practice: from what happens after a polyp is found, to how often you really need a repeat colonoscopy, and what symptoms might be ignored until it’s too late.