Steroid Use MS: Risks, Benefits, and What You Need to Know
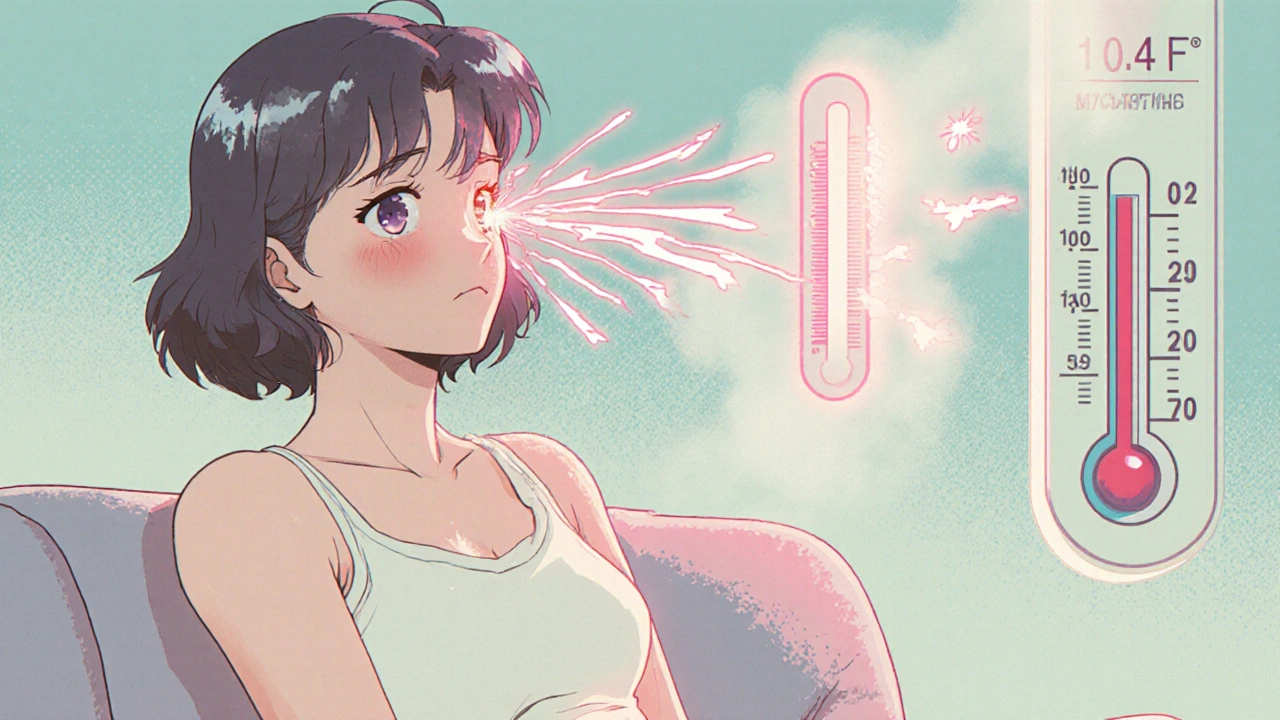
When someone with multiple sclerosis, a chronic autoimmune condition that affects the central nervous system. Also known as MS, it has a flare-up, doctors often turn to corticosteroids, powerful anti-inflammatory drugs that mimic natural hormones in the body to calm things down fast. These aren’t just any pills—they’re high-dose, short-term treatments meant to reduce swelling in the brain and spinal cord, helping people regain function after a relapse. But they’re not harmless. The steroid use MS debate isn’t about whether they work—it’s about how much you’re willing to pay for that relief.
Many people with MS get a few days of high-dose IV methylprednisolone or oral prednisone during a flare. It can make the difference between being stuck at home and getting back to work or walking without help. But the side effects? They’re real. Insomnia, mood swings, stomach upset, elevated blood sugar, and even a weird metallic taste in the mouth. And if you use them too often? Your bones thin out, your immune system weakens, and your body starts to rely on the drug to feel normal. That’s why doctors don’t prescribe them for daily use—they’re a fire extinguisher, not a smoke detector.
What’s often overlooked is how steroid use MS fits into the bigger picture. It doesn’t stop the disease. It doesn’t slow progression. It just masks the symptoms when they’re loud. That’s why people who rely on steroids too often end up with more frequent flares down the line. And when steroids stop working as well, the next step might be stronger disease-modifying drugs—ones with their own risks, like liver damage or infections. The real question isn’t whether steroids help during a flare. It’s whether you’re using them as a crutch instead of a tool.
There’s also the cost of misusing them. Some people buy steroids online without a prescription, thinking they’re just boosting energy or fighting fatigue. That’s dangerous. Steroids aren’t energy pills. They’re hormone-altering drugs that can trigger diabetes, heart problems, or even psychosis in rare cases. And if you’re already managing MS, adding uncontrolled steroid use into the mix? It’s like mixing gasoline and fire.
What you’ll find in the posts below are real, practical insights from people who’ve been there. You’ll see how betamethasone, a potent corticosteroid used for severe allergic reactions and inflammation is sometimes prescribed off-label for MS-related inflammation, how OTC nasal sprays, commonly used for congestion but linked to rebound effects can accidentally worsen MS symptoms, and why generic drugs, lower-cost versions of brand-name medications that must meet FDA bioequivalence standards are sometimes just as effective for MS care—but not always. These aren’t theory pieces. They’re based on actual patient experiences, clinical data, and pharmacy safety checks.
By the end of this collection, you’ll know exactly when steroids make sense for MS, when they’re a bad idea, and what alternatives actually work without the side effects. No fluff. No marketing. Just what you need to decide what’s right for your body.