- Oct, 21 2025
- 14 Comments
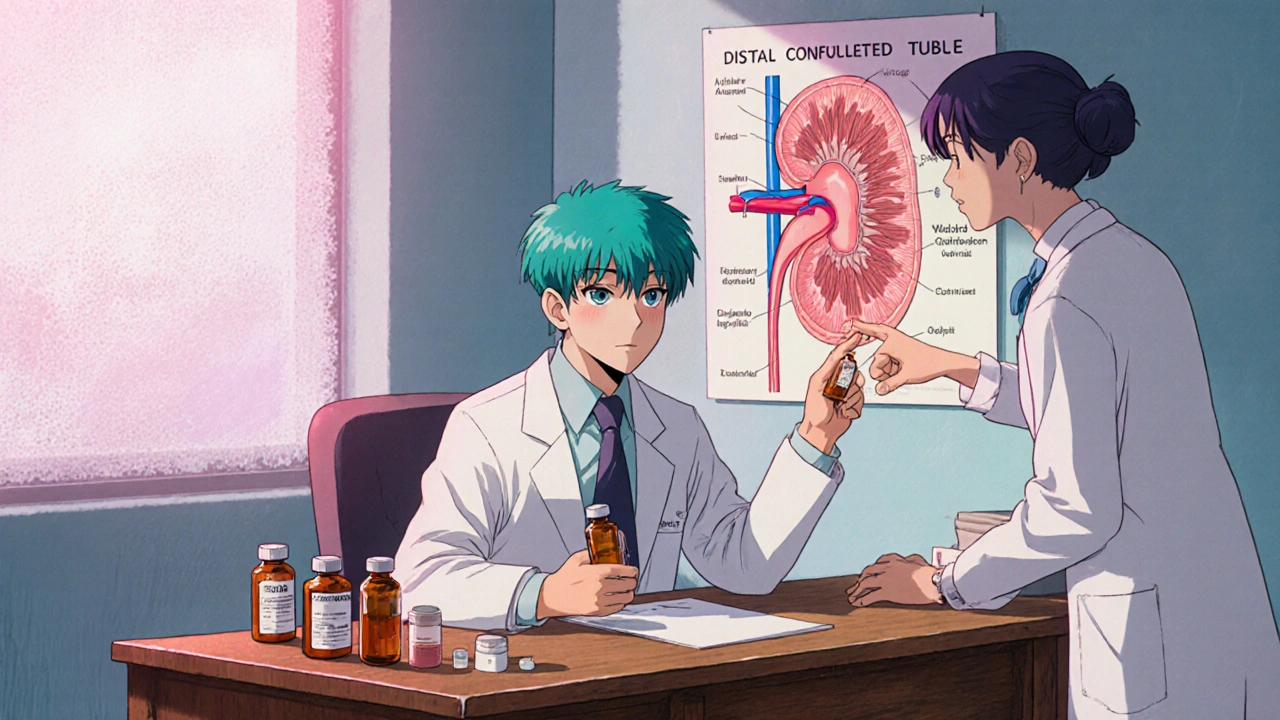
Thiazide Diuretic Overview and Practical Guide
When working with thiazide diuretic, a low‑dose medication that promotes sodium and water excretion through the kidneys. Also known as thiazide‑type diuretic, it is a cornerstone for treating hypertension, elevated arterial pressure that strains the heart and vessels and for preventing fluid overload, excess fluid buildup often seen in heart failure. The drug class works by inhibiting the Na⁺/Cl⁻ transporter in the distal convoluted tubule, which leads to increased urinary loss of sodium and a modest drop in water volume. This mechanism directly reduces blood pressure, making thiazide diuretics one of the first‑line choices in most treatment guidelines.
Key Considerations When Using Thiazide Diuretics
Understanding the relationship between a thiazide diuretic, electrolyte balance, and the concentration of sodium, potassium, and magnesium in the blood is essential. Because the drug pushes sodium out, the body may also lose potassium and magnesium, which can trigger muscle cramps, arrhythmias, or fatigue. Regular labs help catch these shifts early, and a potassium‑rich diet or a potassium‑sparing partner drug (like spironolactone) can offset the drop. Kidney function is another pivotal factor; patients with reduced glomerular filtration rate may experience diminished diuretic efficacy and heightened risk of electrolyte disturbances. In such cases, dosing adjustments or alternative diuretic classes (like loop diuretics) become necessary. Moreover, thiazides can raise uric acid levels, so people with gout should be monitored closely.
Beyond the core pharmacology, thiazide diuretics intersect with many other health topics covered on our site. For instance, patients with type 2 diabetes, a condition that affects glucose metabolism and often co‑exists with hypertension may benefit from the modest glucose‑lowering effect some thiazides exhibit, but they must watch for potential increases in blood sugar. Similarly, anyone taking metformin, a first‑line diabetes medication that can also influence weight should be aware of overlapping side‑effects like gastrointestinal upset. The breadth of our article collection—from the role of sitagliptin‑metformin in weight loss to the safety of generic warfarin—means readers can find complementary guidance that fits their broader medication regimen.
Practical advice for everyday use starts with timing: most clinicians suggest taking thiazide diuretics in the morning to avoid nighttime bathroom trips. Start at a low dose (often 12.5–25 mg of hydrochlorothiazide) and titrate based on blood pressure response and lab results. Encourage patients to stay hydrated, but not over‑hydrate, and to keep an eye on signs of low blood pressure—dizziness, light‑headedness, or blurred vision. Lifestyle tweaks, such as reducing dietary sodium, adding a modest amount of potassium‑rich foods (bananas, avocados, leafy greens), and regular exercise, amplify the drug’s impact. Finally, remind readers to report any muscle pain, sudden weight gain, or persistent fatigue, as these could signal electrolyte issues or an adverse reaction.
Below, you’ll find a curated list of articles that dive deeper into related medications, disease management strategies, and nutritional tips—all chosen to help you get the most out of a thiazide diuretic regimen while staying safe and informed.