Transcription Errors: How Mistakes in Prescriptions Can Harm Your Health
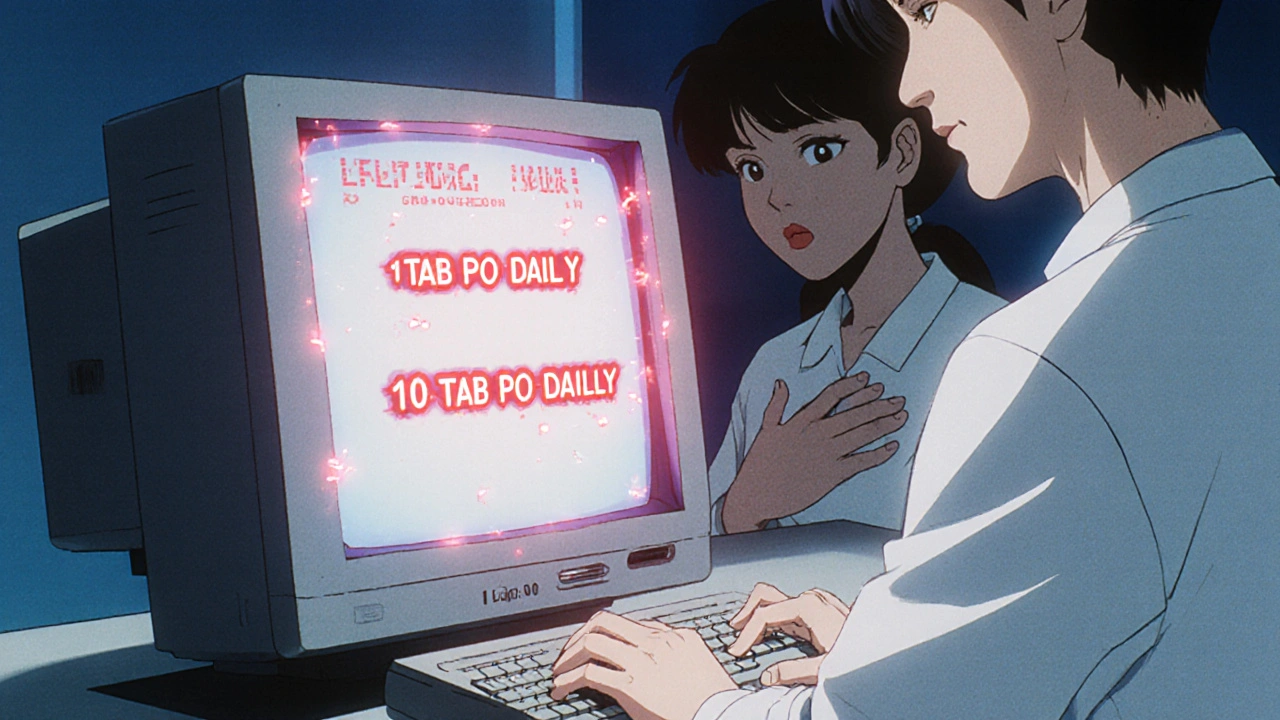
When a doctor writes a prescription and a pharmacist or nurse types it into a system, a simple typo can turn a life-saving drug into a dangerous one. This is a transcription error, a mistake made when handwritten or verbal orders are incorrectly entered into digital systems. Also known as copy error, it’s one of the most common causes of preventable harm in U.S. healthcare. These aren’t just small typos—they’re life-or-death mistakes. A single misplaced decimal point can turn a 5 mg dose into 50 mg. A confused abbreviation like "qd" (once daily) for "qid" (four times daily) can overload your body with medication. And when drugs like insulin, warfarin, or opioids are involved, the consequences can be fatal.
These errors don’t just happen at the pharmacy. They start in clinics, hospitals, and even telehealth visits where handwriting is unclear or voice-to-text tools mishear "Lisinopril" as "Lisinopril 10" or "Lisinopril 100." The medication error, any preventable mistake that causes harm during prescribing, dispensing, or taking a drug often begins with a transcription slip. Studies show that over 7,000 deaths each year in the U.S. are linked to these kinds of mistakes. And while electronic prescribing helped reduce some errors, new ones popped up—like selecting the wrong drug from a dropdown menu or missing a critical alert because of alert fatigue.
Some drugs are far more dangerous when miswritten. Blood thinners like warfarin, diabetes meds like insulin, and seizure drugs like phenytoin have narrow safety windows. A small dose error can trigger bleeding, coma, or seizures. Even common drugs like hydrochlorothiazide or metformin can cause serious harm if the dosage is wrong. And when you’re taking multiple medications—like a combination of roflumilast, venlafaxine, or atazanavir—the risk of a bad interaction skyrockets if one pill’s dose is misrecorded.
The system isn’t broken—it’s overwhelmed. Doctors are rushed. Pharmacists juggle dozens of scripts at once. Nurses are stretched thin. But you don’t have to be passive. Always double-check your prescription label against what your doctor told you. Ask: "Is this the right drug? Is this the right dose?" If you’re given a new pill and it looks different than before, speak up. That’s not just being cautious—it’s protecting your life.
What follows are real cases and practical guides from people who’ve been caught in these errors—and how they fought back. You’ll find posts on how generic drugs are tested for safety, how to spot dangerous interactions between statins and antifungals, and how to store HIV meds correctly to avoid breakdowns. You’ll learn how to read labels, question confusing prescriptions, and use tools like dissolution testing and FDA guidelines to verify your meds are what they claim to be. This isn’t about blaming the system. It’s about giving you the power to stop mistakes before they hurt you.